A Case of Impending Cardiac Tamponade Caused by Effusive Constrictive Pericarditis
Article Information
Catalina Sanchez-Alvarez1, Monia Werlang1, Oludamilola Oluleye2, Mohamad H Yamani2*
1Departments of Internal Medicine, Mayo Clinic, Jacksonville, Florida, United States
2Cardiovascular Medicine, Mayo Clinic, Jacksonville, Florida, United States
*Corresponding Author: Dr. Mohamad H Yamani, Cardiovascular Medicine, Mayo Clinic, Davis 7E, 4500 San Pablo Rd, Jacksonville, Florida 32224, United States, Tel: 904-953-7279; Fax: 904-953-2911;
Received: 12 October 2018; Accepted: 19 October 2018; Published: 23 October 2018
Citation: Catalina Sanchez-Alvarez, Monia Werlang, Oludamilola Oluleye, Mohamad H Yamani. A Case of Impending Cardiac Tamponade Caused by Effusive Constrictive Pericarditis. Archives of Clinical and Medical Case Reports 2 (2018): 157-161.
View / Download Pdf Share at FacebookAbstract
Pericarditis is the most common pericardial disease worldwide, and can be recurrent in one third of the patients with viral and idiopathic pericarditis [1]. The diagnosis of pericarditis should be based on clinical criteria, history, clinical findings, electrocardiographic (ECG) changes and evidence of a pericardial effusion [2]. Elevation of the inflammatory markers and evidence of pericardial inflammation by an imaging technique such as contrast enhancement on the pericardium-CT scan or pericardial edema and pericardial late gadolinium enhancement on cardiac magnetic resonance imaging (MRI) are additional supportive criteria in the diagnosis [1].
Keywords
Cardiac Tamponade, Pericarditis, Pericardium-CT scan, Magnetic resonance imaging
Cardiac Tamponade articles Cardiac Tamponade Research articles Cardiac Tamponade review articles Cardiac Tamponade PubMed articles Cardiac Tamponade PubMed Central articles Cardiac Tamponade 2023 articles Cardiac Tamponade 2024 articles Cardiac Tamponade Scopus articles Cardiac Tamponade impact factor journals Cardiac Tamponade Scopus journals Cardiac Tamponade PubMed journals Cardiac Tamponade medical journals Cardiac Tamponade free journals Cardiac Tamponade best journals Cardiac Tamponade top journals Cardiac Tamponade free medical journals Cardiac Tamponade famous journals Cardiac Tamponade Google Scholar indexed journals Pericarditis articles Pericarditis Research articles Pericarditis review articles Pericarditis PubMed articles Pericarditis PubMed Central articles Pericarditis 2023 articles Pericarditis 2024 articles Pericarditis Scopus articles Pericarditis impact factor journals Pericarditis Scopus journals Pericarditis PubMed journals Pericarditis medical journals Pericarditis free journals Pericarditis best journals Pericarditis top journals Pericarditis free medical journals Pericarditis famous journals Pericarditis Google Scholar indexed journals Pericardium-CT scan articles Pericardium-CT scan Research articles Pericardium-CT scan review articles Pericardium-CT scan PubMed articles Pericardium-CT scan PubMed Central articles Pericardium-CT scan 2023 articles Pericardium-CT scan 2024 articles Pericardium-CT scan Scopus articles Pericardium-CT scan impact factor journals Pericardium-CT scan Scopus journals Pericardium-CT scan PubMed journals Pericardium-CT scan medical journals Pericardium-CT scan free journals Pericardium-CT scan best journals Pericardium-CT scan top journals Pericardium-CT scan free medical journals Pericardium-CT scan famous journals Pericardium-CT scan Google Scholar indexed journals Magnetic resonance imaging articles Magnetic resonance imaging Research articles Magnetic resonance imaging review articles Magnetic resonance imaging PubMed articles Magnetic resonance imaging PubMed Central articles Magnetic resonance imaging 2023 articles Magnetic resonance imaging 2024 articles Magnetic resonance imaging Scopus articles Magnetic resonance imaging impact factor journals Magnetic resonance imaging Scopus journals Magnetic resonance imaging PubMed journals Magnetic resonance imaging medical journals Magnetic resonance imaging free journals Magnetic resonance imaging best journals Magnetic resonance imaging top journals Magnetic resonance imaging free medical journals Magnetic resonance imaging famous journals Magnetic resonance imaging Google Scholar indexed journals CT scan articles CT scan Research articles CT scan review articles CT scan PubMed articles CT scan PubMed Central articles CT scan 2023 articles CT scan 2024 articles CT scan Scopus articles CT scan impact factor journals CT scan Scopus journals CT scan PubMed journals CT scan medical journals CT scan free journals CT scan best journals CT scan top journals CT scan free medical journals CT scan famous journals CT scan Google Scholar indexed journals cytology articles cytology Research articles cytology review articles cytology PubMed articles cytology PubMed Central articles cytology 2023 articles cytology 2024 articles cytology Scopus articles cytology impact factor journals cytology Scopus journals cytology PubMed journals cytology medical journals cytology free journals cytology best journals cytology top journals cytology free medical journals cytology famous journals cytology Google Scholar indexed journals health care articles health care Research articles health care review articles health care PubMed articles health care PubMed Central articles health care 2023 articles health care 2024 articles health care Scopus articles health care impact factor journals health care Scopus journals health care PubMed journals health care medical journals health care free journals health care best journals health care top journals health care free medical journals health care famous journals health care Google Scholar indexed journals ventricle articles ventricle Research articles ventricle review articles ventricle PubMed articles ventricle PubMed Central articles ventricle 2023 articles ventricle 2024 articles ventricle Scopus articles ventricle impact factor journals ventricle Scopus journals ventricle PubMed journals ventricle medical journals ventricle free journals ventricle best journals ventricle top journals ventricle free medical journals ventricle famous journals ventricle Google Scholar indexed journals pathology articles pathology Research articles pathology review articles pathology PubMed articles pathology PubMed Central articles pathology 2023 articles pathology 2024 articles pathology Scopus articles pathology impact factor journals pathology Scopus journals pathology PubMed journals pathology medical journals pathology free journals pathology best journals pathology top journals pathology free medical journals pathology famous journals pathology Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals
Article Details
Untitled Document
1. Case Study
A 33 year old man, with history of recurrent pericarditis, presented with a new episode of chest pain, associated with EKG changes suggestive of pericarditis (Figure 1). A cardiac MRI showed normal thickness of the pericardium with trace effusion (Figure 2). There was no delayed gadolinium enhancement of the pericardium. Patient had extensive workup that was positive for Coxsackie B infection. Patient was started on aspirin and colchicine. A week later, patient presented to the emergency department with worsening symptoms of shortness of breath. On physical examination, blood pressure 90/66 mm hg, pulse 90/min, elevated jugular venous pressure with y descent, pulsus paradoxus, pulsatile hepatomegaly, and mild peripheral edema. Laboratory testing showed ESR of 36 mm/hr, and a CRP of 156.6 mg/L. Chest X-ray showed enlargement of the cardiac silhouette (Figure 3). A high resolution CT scan of the chest showed moderate size pericardial effusion (Figure 4) that was not present before in the initial MRI. A transthoracic echocardiography (TTE) showed evidence of a large circumferential pericardial effusion (Figure 5) with inferior vena cava (IVC) plethora (Figure 6) and both right atrium (RA) and right ventricle (RV) collapse consistent with impending cardiac tamponade. An urgent pericardiocentesis was performed and drained a one liter of sero-sanguineous pericardial fluid with WBC: 1403; PMN: 44%, Lymph: 45%. Cultures were negative and cytology was negative for malignancy. A follow up TTE evidenced resolution of the pericardial effusion, and diffuse thickening of the pericardium, with persistence of a mild respiratory variation in the left ventricle (LV) and right ventricle (RV) filling concerning for pericardial constriction (Figure 7). A heart catheterization confirmed ventricular intra-dependence on simultaneous measurements of the LV and RV consistent with pericardial constriction. Patient was diagnosed with an effusive constrictive pericarditis, and was started on a trial of steroids following which he had significant clinical improvement.
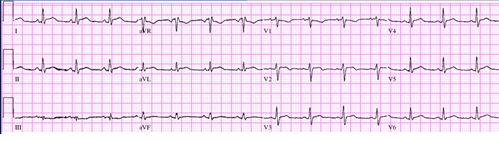
Figure 1: ECG.
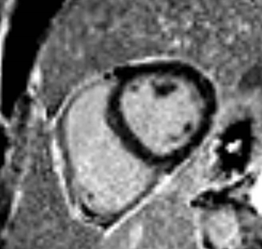
Figure 2: Cardiac MRI.
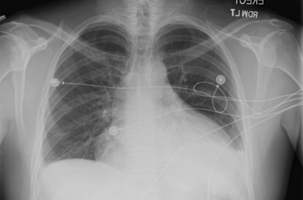
Figure 3: Chest X-ray.

Figure 4: Chest CT scan.
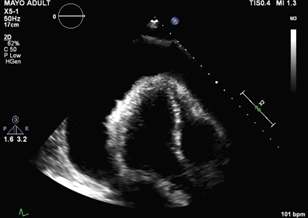
Figure 5: Transthoracic echocardiography.
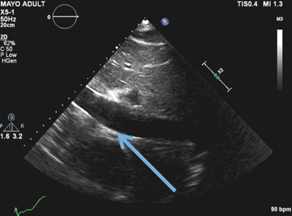
Figure 6: Inferior Vena cava.
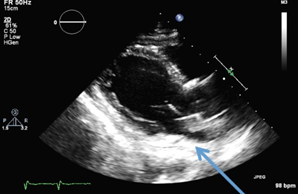
Figure 7: Transthoracic echocardiography post pericardiocentesis.
2. Discussion
Cardiac imaging is frequently used in the diagnosis of pericardial disease. The multimodal integration of different imaging techniques is needed in certain cases [3, 4]. TTE should be used in all the cases of acute pericarditis to identify effusions, and to evaluate for hemodynamic compromise as a reflection of cardiac tamponade [5, 6]. Other diagnostic approaches: hemodynamic cardiac catheterization may be necessary in establishing the diagnosis of constrictive pericarditis when the echocardiogram findings are not conclusive [5]. MRI has become the gold standard for the evaluation of the pericardium. The advantages include: lack of ionizing radiation, better anatomic evaluation and providing physiologic information regarding the cardiac function and wall motion in a non-invasive manner [7]. The sensitivity for late gadolinium enhancement has been reported to range from 94-100% [8, 9]. Even highly sensitive modalities may initially be noncontributory in the initial phase of the disease. Particularly in our case the evidence of a normal MRI could have been due to an early stage of the disorder. And sometimes multiple imaging techniques are used in association with clinical findings to provide a confident diagnosis [8]. Although an important number of patients will require pericardiectomy, some cases have a predominantly inflammatory and reversible pericardial reaction, so a trial of anti-inflammatory agents should be considered before advocating pericardiectomy [10].
References
- Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA 314 (2015): 1498-1506.
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial Disease: Diagnosis and Management. Mayo Clin Proc 85 (2010): 572-593.
- Verhaert D, Gabriel RS, Johnston D, et al. The Role of Multimodality Imaging in the Management of Pericardial Disease. Circ Cardiovasc Imaging 3 (2010): 333-343.
- Cosyns B, Plein S, Nihoyanopoulos P, et al. European Association of Cardiovascular Imaging (EACVI) position paper: Multimodality imaging in pericardial disease. Eur Heart J Cardiovasc Imaging 16 (2015): 12-31.
- Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr off Publ Am Soc Echocardiogr 26 (2013): 965-1012.
- Imazio M, Trinchero R. Myopericarditis: Etiology, management, and prognosis. Int J Cardiol 127 (2008): 17-26.
- Groves R, Chan D, Zagurovskaya M, et al. MR Imaging Evaluation of Pericardial Constriction. Magn Reson Imaging Clin 23 (2015): 81-87.
- Young PM, Glockner JF, Williamson EE, et al. MR imaging findings in 76 consecutive surgically proven cases of pericardial disease with CT and pathologic correlation. Int J Cardiovasc Imaging 28 (2012): 1099-1109.
- Taylor AM, Dymarkowski S, Verbeken EK, et al. Detection of pericardial inflammation with late enhancement cardiac magnetic resonance imaging: initial results. Eur Radiol 16 (2006): 569-574.
- Syed F, Ntsekhe M, Mayosi B, et al. Effusive-constrictive pericarditis. Heart Failure Reviews 18 (2012): 277-287.
Citation: Catalina Sanchez-Alvarez, Monia Werlang, Oludamilola Oluleye, Mohamad H Yamani. A Case of Impending Cardiac Tamponade Caused by Effusive Constrictive Pericarditis. Archives of Clinical and Medical Case Reports 2 (2018): 157-161.
