A Case of Chronic Subdural Haematoma, A Rare Complication of Eclampsia in Pregnancy
Article Information
Rahul Khatri1*, Bhoomika Jain1, Sabrina Mhapankar2, Sushil Kumar3
1Junior Resident, Department of Obstetrics and Gynaecology, MGM Medical College and Research Centre, Navi Mumbai, India
2Assistant Professor, Department of Obstetrics and Gynecology, MGM Medical College and Research Centre, Navi Mumbai, India
3Professor and HOD, Department of Obstetrics and Gynecology, MGM Medical College and Research Centre, Navi Mumbai, India
*Corresponding Author: Rahul Khatri, MBBS, Junior Resident, Department of Obstetrics and Gynaecology, MGM Medical College and research Center, Navi Mumbai, India
Received: 26 November 2020; Accepted: 09 December 2020; Published: 27 January 2021
Citation: Rahul Khatri, Bhoomika Jain, Sabrina Mhapankar, Sushil Kumar. A Case of Chronic Subdural Haematoma, A Rare Complication of Eclampsia in Pregnancy. Obstetrics and Gynecology Research 4 (2021): 007-011.
View / Download Pdf Share at FacebookAbstract
Hypertensive disorders of pregnancy constitute one of the leading causes of maternal and perinatal mortality worldwide. Chronic subdural hematoma is extremely uncommon in Pregnancy. Intracranial haemorrhage (ICH) is deadly complication, if it occurs in pregnancy both mother and fetus gets compromised. Here we present a rare case of Subdural Hematoma in a patient with eclampsia in pregnancy, in which both the mother and baby were discharged with a multidisciplinary approach and early detection of the condition.
Keywords
Chronic Subdural Hematoma, Hypertensive Disorders
Chronic Subdural Hematoma articles Chronic Subdural Hematoma Research articles Chronic Subdural Hematoma review articles Chronic Subdural Hematoma PubMed articles Chronic Subdural Hematoma PubMed Central articles Chronic Subdural Hematoma 2023 articles Chronic Subdural Hematoma 2024 articles Chronic Subdural Hematoma Scopus articles Chronic Subdural Hematoma impact factor journals Chronic Subdural Hematoma Scopus journals Chronic Subdural Hematoma PubMed journals Chronic Subdural Hematoma medical journals Chronic Subdural Hematoma free journals Chronic Subdural Hematoma best journals Chronic Subdural Hematoma top journals Chronic Subdural Hematoma free medical journals Chronic Subdural Hematoma famous journals Chronic Subdural Hematoma Google Scholar indexed journals Hypertensive Disorders articles Hypertensive Disorders Research articles Hypertensive Disorders review articles Hypertensive Disorders PubMed articles Hypertensive Disorders PubMed Central articles Hypertensive Disorders 2023 articles Hypertensive Disorders 2024 articles Hypertensive Disorders Scopus articles Hypertensive Disorders impact factor journals Hypertensive Disorders Scopus journals Hypertensive Disorders PubMed journals Hypertensive Disorders medical journals Hypertensive Disorders free journals Hypertensive Disorders best journals Hypertensive Disorders top journals Hypertensive Disorders free medical journals Hypertensive Disorders famous journals Hypertensive Disorders Google Scholar indexed journals pregnancy articles pregnancy Research articles pregnancy review articles pregnancy PubMed articles pregnancy PubMed Central articles pregnancy 2023 articles pregnancy 2024 articles pregnancy Scopus articles pregnancy impact factor journals pregnancy Scopus journals pregnancy PubMed journals pregnancy medical journals pregnancy free journals pregnancy best journals pregnancy top journals pregnancy free medical journals pregnancy famous journals pregnancy Google Scholar indexed journals fetus articles fetus Research articles fetus review articles fetus PubMed articles fetus PubMed Central articles fetus 2023 articles fetus 2024 articles fetus Scopus articles fetus impact factor journals fetus Scopus journals fetus PubMed journals fetus medical journals fetus free journals fetus best journals fetus top journals fetus free medical journals fetus famous journals fetus Google Scholar indexed journals Obstetrics articles Obstetrics Research articles Obstetrics review articles Obstetrics PubMed articles Obstetrics PubMed Central articles Obstetrics 2023 articles Obstetrics 2024 articles Obstetrics Scopus articles Obstetrics impact factor journals Obstetrics Scopus journals Obstetrics PubMed journals Obstetrics medical journals Obstetrics free journals Obstetrics best journals Obstetrics top journals Obstetrics free medical journals Obstetrics famous journals Obstetrics Google Scholar indexed journals Gynaecology articles Gynaecology Research articles Gynaecology review articles Gynaecology PubMed articles Gynaecology PubMed Central articles Gynaecology 2023 articles Gynaecology 2024 articles Gynaecology Scopus articles Gynaecology impact factor journals Gynaecology Scopus journals Gynaecology PubMed journals Gynaecology medical journals Gynaecology free journals Gynaecology best journals Gynaecology top journals Gynaecology free medical journals Gynaecology famous journals Gynaecology Google Scholar indexed journals maternal articles maternal Research articles maternal review articles maternal PubMed articles maternal PubMed Central articles maternal 2023 articles maternal 2024 articles maternal Scopus articles maternal impact factor journals maternal Scopus journals maternal PubMed journals maternal medical journals maternal free journals maternal best journals maternal top journals maternal free medical journals maternal famous journals maternal Google Scholar indexed journals perinatal articles perinatal Research articles perinatal review articles perinatal PubMed articles perinatal PubMed Central articles perinatal 2023 articles perinatal 2024 articles perinatal Scopus articles perinatal impact factor journals perinatal Scopus journals perinatal PubMed journals perinatal medical journals perinatal free journals perinatal best journals perinatal top journals perinatal free medical journals perinatal famous journals perinatal Google Scholar indexed journals Vaginal articles Vaginal Research articles Vaginal review articles Vaginal PubMed articles Vaginal PubMed Central articles Vaginal 2023 articles Vaginal 2024 articles Vaginal Scopus articles Vaginal impact factor journals Vaginal Scopus journals Vaginal PubMed journals Vaginal medical journals Vaginal free journals Vaginal best journals Vaginal top journals Vaginal free medical journals Vaginal famous journals Vaginal Google Scholar indexed journals gestation articles gestation Research articles gestation review articles gestation PubMed articles gestation PubMed Central articles gestation 2023 articles gestation 2024 articles gestation Scopus articles gestation impact factor journals gestation Scopus journals gestation PubMed journals gestation medical journals gestation free journals gestation best journals gestation top journals gestation free medical journals gestation famous journals gestation Google Scholar indexed journals
Article Details
1. Introduction
Hypertensive disorders of pregnancy constitute one of
the leading causes of maternal and perinatal mortality worldwide. It has been estimated that preeclampsia complicates 2–8% of pregnancies globally [1]. Although maternal mortality is much lower in high-income countries than in developing countries, 16% of maternal deaths can be attributed to hypertensive disorders [1, 2].
Intracranial Haemorrhage is a rare complication of Pre-eclampsia/Eclampsia in pregnancy. When stroke (ischemic or haemorrhagic) occurs during pregnancy, both women and the child may have devastating outcomes [3]. The incidence of stroke in pregnant patients is estimated at 34.2 per 100,000 deliveries, and the mortality rate is 1.4 per 1,00,000 [4] deliveries, accounting for both types.
Here we present a rare case of Subdural Hematoma in a
patient with Eclampsia in pregnancy, in which both mother and baby were discharged uneventfully.
2. Case Report
A 28 year-old female G2P1D1 previous Vaginal Delivery with 29 weeks of gestation was brought to the casualty in an unconscious state with a history of convulsions. On examination, Her general condition was poor, her Pulse was 120 beats per minute, with BP of 130/90mmHg, SpO2 - 99% on RA, Respiratory Rate of 22 per minute. There was No pallor/icterus. Bilateral pedal oedema was present with urine albumin of +2. On systemic examination, heart sound s1s2 was present, no murmur was heard, and air entry was bilaterally equal.
On CNS examination, she was unconscious, not responding to commands, anisocoria was noted, and a corneal reflex was present. On Per Abdomen, Uterus was 28-30wks, the size and lie of fetus was Longitudinal with cephalic, Fetal heart sounds were well appreciated, and Uterus was relaxed. On Per Speculum examination, Cervix & Vagina was Healthy. On Per Vaginal examination, the cervical os was closed. No signs of external trauma were seen.
Patient intubated in view of poor GCS (Glasgow Coma Scale), Urgent MRI brain was done, which was s/o a Subdural Hematoma on the left fronto-temporo-parietal region as seen in Figure 1. Her Blood investigations were normal with haemoglobin of 12.2gm/dl, total counts of 15,210 and platelets of 2.56lakhs. Her coagulation profile was within normal limits; her prothrombin time was 11.6seconds with a test time of 11.7seconds and INR of 0.99 and aPTT of 27.90 seconds with a test time of 32 seconds.
Liver function test suggested total bilirubin of 0.80mg/dl, direct bilirubin of 0.14mg/dl, SGOT of 22U/L and SGPT of 9U/L. She had normal kidney function with creatinine of 0.49mg/dl. Urgent Neurosurgery opinion was sought, and the decision of emergency Craniectomy was taken. After High-risk consent, the patient shifted to OT. Craniectomy was done, left temporal bone removed, Dura mater opened, chronic subdural haemorrhage seen, clots removed of weighting around 100grams, and closure done after ensuring haemostasis.
Patient shifted to SICU for further management. In SICU, the patient went into spontaneous labor on post-operative day 5 and delivered vaginally, a male baby of 1.9kg, baby shifted to NICU i/v/o preterm low birth weight. Recovery period was uneventful. Repeat CT Brain Suggested no haemorrhage/clot. Patient recovered well, both mother and baby were discharged on post-operative day 28. Temporal Bone replacement surgery was done after 6 months.
Intra-operative photos, Figure 2 showing the clot seen post-dural flap retraction, Figure 3 showing clots being evacuated, and Figure 4 showing how haemostasis achieved.

Figure 1: MRI brain T2 weighted image.
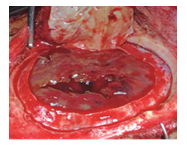
Figure 2: Opening dura mater, Clots seen.
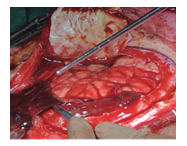
Figure 3: Clots being removed.
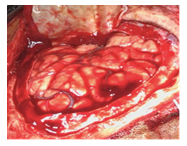
Figure 4: Hemostasis achieved.
3. Discussion
Pre-eclampsia and eclampsia, physiological changes peculiar to pregnancy, are major causes of intracranial haemorrhage during pregnancy and in the puerperium [5, 6] HELLP syndrome is the combination of haemolysis (H), elevated liver enzymes (EL),and low platelet count (LP). Cases of spontaneous intracranial haemorrhage with or without HELLP syndrome, thrombotic microangiopathy, or thrombocytopenia are reported in the literature. The most recent report on enquiries into maternal death in the United Kingdom showed that the majority of women with preeclampsia died from intracranial haemorrhage [7]. Some cases of preeclampsia with subdural haemorrhage and how they presented are stated below according to the literature.
Table 1: Similar cases found in previous case studies.
4. Conclusion
Subdural Hematoma is a complication of pre-eclampsia/eclampsia although it is rare but can happen anytime without the presence of HELLP Syndrome/ thrombocytopenia or any other coagulation abnormality. It may be because of stretching and tearing of bridging veins between the cortex and dural venous sinuses. Chronic subdural hematoma is extremely uncommon in Pregnancy. Intracranial haemorrhage (ICH) is a deadly complication, if it occurs in pregnancy and both the mother and fetus get compromised. Moreover can lead to lifelong morbidity, so prompt and accurate identification of signs and symptoms and early intervention with a multidisciplinary approach can prevent maternal and fetal morbidity and mortality. Urgent neurosurgical conditions usually outweigh obstetric considerations and the treatment of ICH is generally the same as nonpregnant women. Effective decision making demands thorough knowledge, thus multidisciplinary obstetric disaster preparedness is essential for all institutions.
References
- Steegers EA, von Dadelszen P, Duvekot JJ, et al. Pre-eclampsia. Lancet 376 (2010): 631-644.
- Khan KS, Wojdyla D, Say L, et al. WHO analysis of causes of maternal death: a systematic review. Lancet 367 (2006): 1066-1074.
- Fairhall JM, Stoodley MA. Intracranial haemorrhage in pregnancy. Obstet Med 2 (2009): 142-148.
- James AH, Bushnell CD, Jamison MG, et al. Incidence and risk factors for stroke in pregnancy and puerperium. Obstet Gynecol 106 (2005): 509-516.
- Bateman B, Schumacher H, Bushnell C, et al. Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology 67 (2006): 424-429.
- Sharshar T, Lamy C, Mas JL, et al. Incidence and causes of stroke associated with pregnancy and puerperium. A study in public hospitals of Île de France. Stroke 26 (1995): 930-936.
- The Confidential Enquiry into Maternal and Child Health (CEMACH). In: Lewis G,editor. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer – 2003–2005. The seventh report on confidential enquiries into maternal deaths in the United Kingdom. London: CEMACH (2007).
- Giannina G, Smith D, Belfort M A, et al. Atraumatic Subdural Hematoma Associated with Pre-Eclampsia. Journal of Maternal-Fetal and Neonatal Medicine 6 (1997): 93-95.
- Maitree Pandey, Namita Saraswat, Homay Vajifdar, et al. Subdural hematoma in pregnancy-induced idiopathic thrombocytopenia: conservative management. Indian J Anaesth 54 (2010): 470-471.
- Sâmia Y, Wottrich J, Uggeri D, et al. Spontaneous acute subdural hematoma and intracerebral hemorrhage in a patient with thrombotic microangiopathy during pregnancy. Rev Bras Ter Intensiva 25 (2013): 175-180.
- Djoubairou B O, Onen J, Doleagbenou A K, et al. Chronic subdural haematoma associated with preeclampsia: Case report and review of the literature. Neurochirurgie 60 (2014): 48-50.
