Wyburn Mason Syndrome: Novel presentation with Bilateral Retinal Arteriovenous malformation
Article Information
Deepesh Aroraa*, Kanika Guptaa, Yogesh kumarb, Dinesh sharmaa
aAmritsar Eye Clinic, 122/1, Municipal Road, Dehradun, 248001, Uttarakhand, India
bAssociate Professor of Ophthalmology, Shaheed Hasan khan Mewati Govt Medical College, Nuh, Mewat, Haryana, India
*Corresponding Author: Deepesh Arora, Vitreo-retina consultant, Amritsar Eye Clinic, 122/1, Municipal Road, Dehradun, 248001, Uttarakhand, India
Received: 11 October 2020; Accepted: 22 October 2020; Published: 02 November 2020
Citation: Deepesh Arora, Kanika Gupta, Yogesh kumar, Dinesh sharma. Wyburn Mason Syndrome: Novel presentation with Bilateral Retinal Arteriovenous malformation. Journal of Ophthalmology and Research 3 (2020): 79-85.
View / Download Pdf Share at FacebookAbstract
A five-year-old girl with poor vision on examination and left eye esotropia was found to have bilateral intraorbital and unilateral intracranial arteriovenous malformation (AVM) and unilateral optic neuropathy. Magnetic Resonance Imaging with contrast revealed a small AVM involving the left ophthalmic artery and a large AVM involving the junction of anterior cerebral artery and anterior communicating artery. The simultaneous presence of retinal and intracranial AVM constitutes the Wyburn- Mason Syndrome (Retinoencephaloangiomatosis). Wyburn mason syndrome is associated with unilateral retinal racemose hemangioma with few cases with bilateral symmetrical involvement been reported in the literature. The present case has asymmetric bilateral retinal AVM and optic neuropathy, rare presentation of rare disease.
Keywords
AVM; Optic neuropathy; Esotropia
Article Details
Introduction
The Wyburn-Mason syndrome is racemose haemangioma involving ipsilateral midbrain and retina [1]. It is non familial rare disorder of phacomatoses, occasionally presenting with facial angiomas and is also known as Bonnet-Dechaume-blanc syndrome [1,2,3]. Worldwide incidence is rare with less than 100 cases reported in literature [4]. Pioneering work came from large series of 27 cases reported by Wyburn Mason, 22 of which also had intracranial vascular malformation [1]. WMS has unilateral ocular presentation and only few cases with bilateral symmetrical retinal AVM (arterio venous malformation) have been reported [4].
Case Report
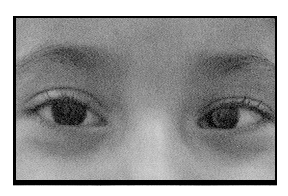
A 6-year-old girl from hill state of Uttarakhand was brought to our outpatient department by her parents with complaint of left eye inward deviation since birth. She had been examined elsewhere and had been referred for specialist evaluation at a higher centre. Visual acuity was OD 6/6 and OS 6/60. Ocular examination revealed OS esotropia (Figure 1) with normal pupillary reaction in right eye and relative afferent pupillary defect (RAPD) in left eye.
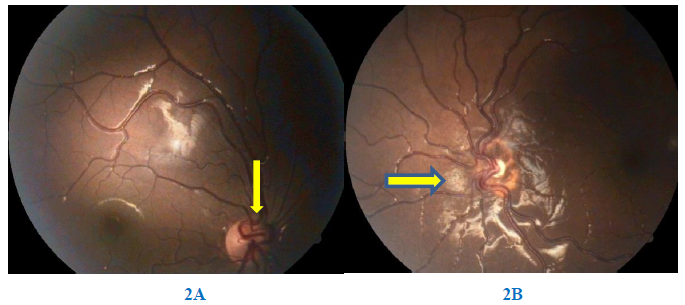
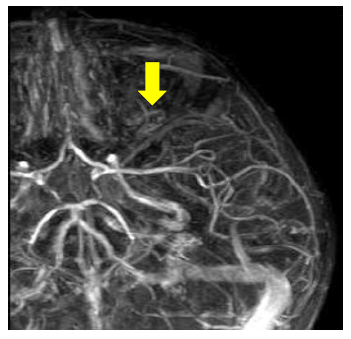
Posterior segment examination showed arteriovenous anastomosis over both optic nerve head along with dilated and tortuous vessels with AV communications and optic atrophy of left eye.(Figure 2: A, B).
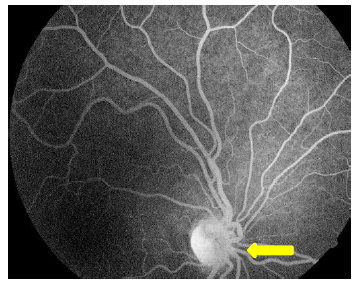
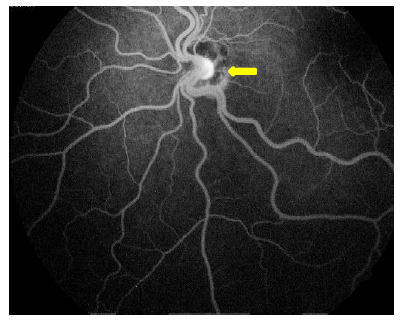
AVMs in right eye and left eye were of group II and group III respectively. Fundus fluorescein angiography (Figure 2-C & D: FFA) showed no leakage from the AVMs in both eyes with late phase staining of optic nerve head.
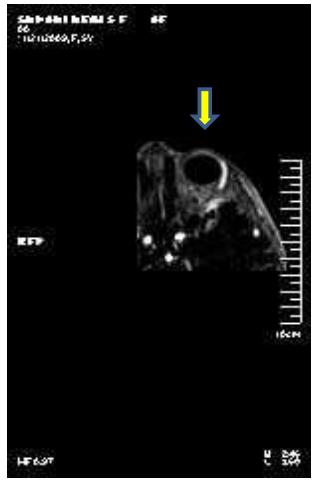
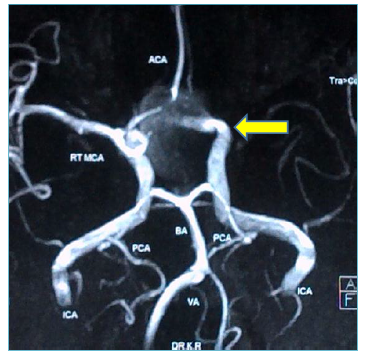
Orbit and brain magnetic resonance imaging with contrast (MRI) disclosed a small AVM in the intraconal space behind left globe involving ophthalmic artery and another involving junction of anterior cerebral and anterior communicating artery. (Figure 2 E, F and G).
Discussion
AVMs in Wyburn-Mason may be seen anywhere along the visual pathway from retina to occipital cortex [5]. The retinal lesion may appear as a dilated and tortuous arteriole in anastomosis with a venule or main vein seen over the optic disc and retina [6,7]. These may appear as tumour like vascular masses [8]. The disorder occurs as a result of hindrance in embryological development of vascular mesoderm [6]. Early identification of the retinal lesion may help in searching for intracranial AVM [6]. Theron et al reviewed 80 cases of retinal AVM and found 25 cases to have CNS (central nervous system) AVM and of these 10 cases also had facial AVM. It is estimated that 8% of patient who have such lesions in CNS may also have retinal lesions [3]. Visual symptoms and signs may be variable depending on the type and extent of vascular malformation as suggested by Archer et al. As per the classification group 1 have abnormal capillary plexus between artery and vein with no vascular decompensation or visual change and intracranial AVM are rare, group 2 shows direct arteriovenous communication with absence of capillary network and occasional retinal decompensation and low risk of intracranial AVM’s, group 3 lesion cause retinal, optic nerve and vascular decompensation, thereby causing profound visual loss with risk of intraorbital and intracranial AVM being high [7] as was detected in present case. Retinal AVM remain stable as well as stationary do not grow or bleed and usually do not cause visual loss [7,10]. However, thrombosis of draining venous channels or sclerosis of vessels wall may occur giving rise to [5] branch retinal vein obstruction [8] and development of neovascular glaucoma due to AV shunting [5,8,9]. Decreased visual acuity in some cases of orbitocranial AVM may be related to progressive optic neuropathy [9,10] as was seen in our case.
The most common site for CNS lesion in Wyburn-Mason syndrome is midbrain [1]. Neurological presentation may vary depending on the site, size and extent of lesion. Neuro-ophthalmological features include optic atrophy, papilledema, pupillary changes, gaze paresis, strabismus, nystagmus, cranial nerve palsies and amblyopia [4]. In present case we detected esotropia and optic atrophy in the left eye explaining the presence of RAPD. Among the 27 patients of retinal AVM seen by Wyburn-Mason, 22 (81%) had signs of intracranial AVM [5], as diagnostic imaging or autopsy information evidence was available only for 21 cases [10]. The presentations were variable and on basis of symptoms 11 cases were correlated to intracranial AVM [1,10], 7 to optic neuropathy [9, 10] and 3 to extracranial AVM [10]. Our case had AVM involving left ophthalmic artery and another at junction of anterior cerebral artery with anterior communicating artery with intracranial being asymptomatic (Figure 2 E, F).
Fundus fluorescein angiography (FFA) helps in further classification of disease. Stability is shown by most AVMs with fluorescein angiography showing rapid transit of dye with presence of no leakage [10] as was seen in this case (Figure 2 C, D).
Intracranial arteriovenous malformations are best diagnosed with catheter angiography which demonstrates the characteristics of feeding arteries and draining veins [4,10]. MRI with contrast was used in present case revealing AVM involving left ophthalmic and junction of anterior cerebral and anterior communicating artery. Available data for intracranial AVM in Wyburn Mason show their presentations similar to isolated AVMs which have a rupture rate of 2.2% per year [10]. The AVMs in Wyburn Mason however are large and deep seated in the midbrain making them less easily accessible for surgery. Procedures as stereotactic radiosurgery, endovascular embolization, surgical resection and irradiation [4,10] may be used to treat these cases keeping in mind the risk factors involved. In our case we kept the child under observation due to its asymptomatic nature and also due to deep seated and multiple locations of the AVM.
Conclusion
WMS is rare type of phacomatoses with unilateral or bilateral symmetrical ocular presentation with associated intracranial AVM. Asymmetric bilateral ocular presentation with unilateral optic neuropathy is rare presentation as seen in our case. Severe ocular involvement in WMS warrants imaging and as in our case proves frequent association with intracranial AVM. Observation and frequent follow up is recommended due to asymptomatic nature of AVM in majority of cases. In our case we kept the child under observation for asymptomatic and deep seated multiple AVM.
Disclosure Statement:
The authors do not have any financial disclosure.
Funding Sources:
None
References
- Wyburn-Mason R. Arteriovenous aneurysm of mid-brain and retina, facial naevi and mental changes. Brain 66 (1943): 163-203.
- Bonnet P, Dechaume J, Blanc E. L’anévrysme cirsoïde de la rétine (anévrysme recémeux): ses relations avec l’anéurysme cirsoïde de la face et avec l’anévrysme cirsoïde du cerveau. J Med Lyon 18 (1937): 165-178.
- Theron J, Newton TH, Hoyt WF. Unilateral retinocephalic vascular malformations. Neuroradiology 7 (1974): 185-196.
- Lee AG, Al-Zubedi N, Byoung UR. Wyburn-Mason Syndrome: clinical presentation, work, treatment and management. Phacomatosis. Articles in Ophthalmology. Drugs and Disease. Medscape (2019).
- Ferry AP; other phacomatoses. Retina Vol.1. Second Edition. St Louis Baltimore Boston Chicago London Madrid Philadelphia Sydney Toronto. Mosby (1989): 653-656.
- Selhorst JB. Phacomatoses. In: Miller NR, Newman NJ, eds. Walsh and Hoyt Clinical Neuro-Ophthalmology, 5th ed. Baltimore: Williams and Wilkins (1998): 2725-2729.
- Brown GC. Congenital retinal arteriovenous communications (racemose hemangiomas). Retina-vitreous-macula. Philadelphia: WB Saunders (1999): 1172-1174.
- Guyer DR, Yannuzzi LA, Chang S, et al. Retina-vitreous-macula. Retina 19 (1999): 265.
- Shields CL, Shields JA; Phakomatoses. Retina Vol.3. Fifth Edition. London Newyork Oxford St Louis Sydney Toronto. Saunders-Elseviers (2013): 2176-2177.
- Effron L, Zakov ZN, Tomsak RL. Neovascular glaucoma as a complication of the Wyburn-Mason syndrome.J Clin Neuroophthalmol (1985): 95-98.
Reck SD, Zack DN, Eibschitz-Tsimhoni M. Retinal and Intracranial Arteriovenous Malformations: Wyburn-Mason Syndrome. Journal of Neuro-ophthalmology (2005): 205-208.