Wallerian Degeneration of Optic Nerve due to Neonatal Intra-cranial Hemorrhage
Article Information
Maryam Naser, Nafiseh Hashemi*
Hashemi Eye Care, Encino, CA, USA.
*Corresponding Author: Nafiseh Hashemi, MD, Hashemi Eye Care, 5353 Balboa Blvd #110, Encino, CA, USA
Received: 03 September 2020; Accepted: 14 September 2020; Published: 18 September 2020
Citation: Maryam Naser, Nafiseh Hashemi. Wallerian Degeneration of Optic Nerve due to Neonatal Intra-cranial Hemorrhage. Journal of Ophthalmology and Research 3 (2020): 61-64.
View / Download Pdf Share at FacebookAbstract
Abstract
Wallerian degeneration is a process that happens following nerve fiber damage, in which the part of the axon distal to the injury degenerates. This is also termed as anterograde or orthograde degeneration. We present a case of 16 year-old patient who was referred to neuro-ophthalmology clinic for glaucoma suspect evaluation which concluded to be related to Wallerian degeneration from neonatal intra-cranial hemorrhage.
Keywords
Wallerian degeneration; Intracranial hemorrhage; Optic neuropathy; Glaucoma suspect
Wallerian degeneration articles, Intracranial hemorrhage articles, Optic neuropathy articles, Glaucoma suspect articles
Article Details
Case Presentation
A 16-year-old hispanic male was referred to neuro-ophthalmology clinic with concern for glaucoma. The patient saw optometrist for the first time with complaint of blurry peripheral vision and allergic conjunctivitis. He denied headaches, double vision or history of trauma to the head. He does not have any significant past medical history except neonatal intra-cranial hemorrhage. The patient was born at 29 weeks. He was under oxygen in the hospital for 3 months. He continued to take oxygen for the first 5 months after discharge at home. His mother reports that the patient had intracranial hemorrhage when he was born but there was no retinopathy of prematurity or any other ophthalmic condition as a new born. There is no family history of glaucoma or any hereditary ocular conditions.
On eye exam, He has acute follicular conjunctivitis on both eyes. Vision is 20/20 and IOP is 10 OU. Color vision is full. Pachymetry shows corneal thickness of 551 mic right eye and 562 mic left eye. Gonioscopy was performed on both eyes which shows open angle (40 degrees), 1-2+ pigment on trabecular meshwork, visible ciliary body and flat
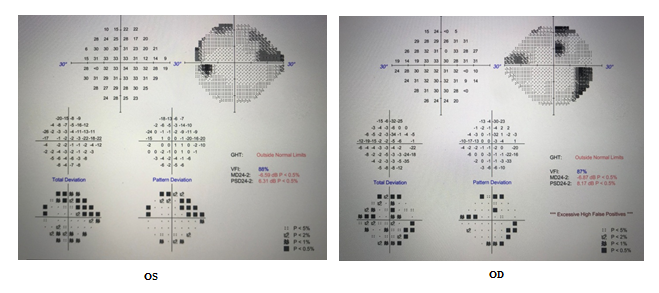
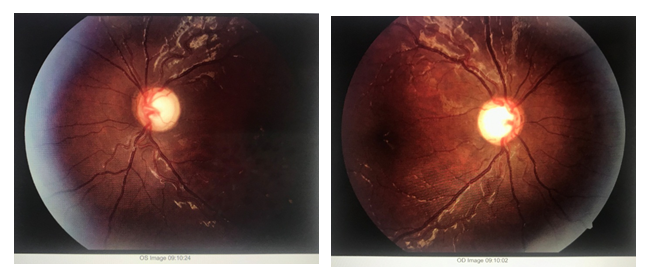
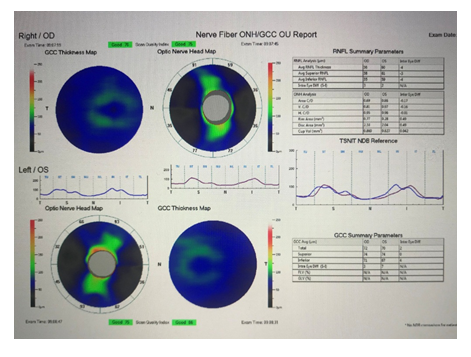
iris. Visual field showed arcuate defects consistent with optic nerve pathology on both eyes (Figure 1). Fundus photo shows cupping of optic nerve (Figure 2). OCT optic nerve reveals diffuse RNFL thinning (Figure 3).
MRI brain and orbit was performed which showed normal brain structure with bilateral optic atrophy.
Discussion
Neurological disorders and traumatic nerve damages can result in axonal degeneration. Wallerian degeneration is a phenomenon in the prototypical axonal degradation that presents after injury [1]. In central nervous system the most common causes are hemorrhage, infarction, tumors, and head injury [2]. Corticospinal tract Wallerian degeneration usually happens in deep spontaneous intracerebral hemorrhage (ICH) which is associated with weak motor and functional recovery after ICH [3]. A study on 39 neonates with hypoxia-ischemia showed that most of the time, pre-wallerian degeneration of the cerebral peduncles is causing poor motor development [4]. In children born prematurely, visual system can be affected in many different ways along its course. Visual field defects in preterm children are associated to visual pathway, retina or treatment of retinopathy of prematurity. Neurological problems such as ischemic brain injury and intraventricular hemorrhage, can lead to visual impairment later in life like our case [5,6]. In our patient, He has noticed peripheral vision loss while he was trying to learn driving. He has had normal eye exam when discharged from hospital as a new born. He passed all of childhood visual screening tests. We are not sure at what age he has developed optic atrophy. Complete eye exam rule out glaucoma or any other pathology contributed to the atrophy. We concluded that the optic nerve atrophy is related to wallerian degeneration due to intracranial atrophy as a new born.
Conclusion
We presented a case with wallerian degeneration of optic nerve secondary to remote intracranial bleeding. Careful review of neonatal history may reveal the etiology of abnormal optic nerve and associated visual field defect. The authors suggest to inform the parent of neonate with ICH about the possibility of having nerve damage and limitation in peripheral vision in the future. Retinopathy of prematurity is not the only concerning visual outcome of prematurity. In a kid with history of neonatal ICH, optic nerve damage may happen due to Wallerian degeneration.
References
- Kinoshita Y, Kondo S, Takahashi K, et al. Genetic inhibition of CRMP2 phosphorylation delays Wallerian degeneration after optic nerve injury. Biochemical and Biophysical Research Communications 514 (2019): 1037-1039.
- Valk J, van der Knaap MS. Wallerian Degeneration and Demyelination Secondary to Neuronal and Axonal Degeneration. InMagnetic Resonance of Myelin, Myelination, and Myelin Disorders (1989): 319-326.
- Venkatasubramanian C, Kleinman JT, Fischbein NJ, et al. Natural history and prognostic value of corticospinal tract Wallerian degeneration in intracerebral hemorrhage. Journal of the American Heart Association 2 (2013): e000090.
- Groenendaal F, Benders MJ, De Vries LS. Pre-wallerian degeneration in the neonatal brain following perinatal cerebral hypoxia–ischemia demonstrated with MRI. InSeminars in Perinatology 30 (2006): 146-150.
- Dobson V, Quinn GE, Abramov I, et al. Color vision measured with pseudoisochromatic plates at five-and-a-half years in eyes of children from the CRYO-ROP study. Investigative Ophthalmology & Visual Science 37 (1996): 2467-2474.
- Harvey EM, PhD VD, Scher MS. Grating acuity and visual-field development in children with intraventricular hemorrhage. Developmental Medicine & Child Neurology 39 (1997): 305-312.