Treatment of Large Bone Defect of Long Bones: Comparison of Free Vascularized Fibular Graft with Compression-Distraction Technique
Article Information
Kuk-Chol Kim*, Song-Gun Ri, Myong-Guk Jang, Su-Ryon Ryang
Pyongyang Medical College, KIM IL SUNG University, Pyongyang, Democratic People’s Republic of Korea
*Corresponding Author: Kuk-Chol Kim, Pyongyang Medical College, KIM IL SUNG University, Pyongyang, Democratic People’s Republic of Korea
Received: 25 July 2019; Accepted: 08 August 2019; Published: 05 September 2019
Citation: Kuk-Chol Kim, Song-Gun Ri, Myong-Guk Jang, Su-Ryon Ryang. Treatment of Large Bone Defect of Long Bones: Comparison of Free Vascularized Fibular Graft with Compression-Distraction Technique. Journal of Orthopaedics and Sports Medicine 1 (2019): 066-077.
View / Download Pdf Share at FacebookAbstract
We treated 18 patients with congenital pseudarthrosis of tibia and 27 patients with acquired bone loss. Out of 18 cases of congenital pseudarthrosis of tibia the free vascularized fibular grafts (FVFGs) were performed in 16 cases and compression-distraction techniques in 2 cases. In patients with angular deformities and shortenings in the lower leg soft tissue distraction and correction were conducted. The mean soft tissue distraction period was 78.4 days, the length of bone defect 10.7 cm, the mean operative time 3.2 hours, and primary bone healing achieved in 12 cases. The mean union period was 7.3 months and the mean period of full weight bearing was 10.8 months. In 4 cases pseudarthroses and deformities developed and healed secondarily, and the treatment period ranged from 16 months to 26 months. The mean length of bone defects was 9.7 cm and the mean period of full weight bearing 14 months. The mean length of bone defects in the group of Ilizarov technique was 6.6 cm, the mean period of distraction 82 days and the mean period of full weight bearing 12.2 months. The complications include pseudarthrosis, refracture, angular deformity, equinovarus and temporary peroneal nerve palsy in the FVFG group and in the group of compression-distraction technique, refracture, equinovarus and temporary peroneal nerve palsy. The FVFG is suitable for the treatment of pseudarthrosis in young patients and the compression-distraction technique is effective option for the treatment of bone defects of patients with infection and deformity.
Keywords
Large bone defect, Free vascularized fibular graft (FVFG), Ilizarov external fixator, Compression-distraction
Bone defect articles Bone defect Research articles Bone defect review articles Bone defect PubMed articles Bone defect PubMed Central articles Bone defect 2023 articles Bone defect 2024 articles Bone defect Scopus articles Bone defect impact factor journals Bone defect Scopus journals Bone defect PubMed journals Bone defect medical journals Bone defect free journals Bone defect best journals Bone defect top journals Bone defect free medical journals Bone defect famous journals Bone defect Google Scholar indexed journals Vascularized fibular graft articles Vascularized fibular graft Research articles Vascularized fibular graft review articles Vascularized fibular graft PubMed articles Vascularized fibular graft PubMed Central articles Vascularized fibular graft 2023 articles Vascularized fibular graft 2024 articles Vascularized fibular graft Scopus articles Vascularized fibular graft impact factor journals Vascularized fibular graft Scopus journals Vascularized fibular graft PubMed journals Vascularized fibular graft medical journals Vascularized fibular graft free journals Vascularized fibular graft best journals Vascularized fibular graft top journals Vascularized fibular graft free medical journals Vascularized fibular graft famous journals Vascularized fibular graft Google Scholar indexed journals Skeletal defects articles Skeletal defects Research articles Skeletal defects review articles Skeletal defects PubMed articles Skeletal defects PubMed Central articles Skeletal defects 2023 articles Skeletal defects 2024 articles Skeletal defects Scopus articles Skeletal defects impact factor journals Skeletal defects Scopus journals Skeletal defects PubMed journals Skeletal defects medical journals Skeletal defects free journals Skeletal defects best journals Skeletal defects top journals Skeletal defects free medical journals Skeletal defects famous journals Skeletal defects Google Scholar indexed journals Soft tissue damage articles Soft tissue damage Research articles Soft tissue damage review articles Soft tissue damage PubMed articles Soft tissue damage PubMed Central articles Soft tissue damage 2023 articles Soft tissue damage 2024 articles Soft tissue damage Scopus articles Soft tissue damage impact factor journals Soft tissue damage Scopus journals Soft tissue damage PubMed journals Soft tissue damage medical journals Soft tissue damage free journals Soft tissue damage best journals Soft tissue damage top journals Soft tissue damage free medical journals Soft tissue damage famous journals Soft tissue damage Google Scholar indexed journals Congenital pseudarthrosis articles Congenital pseudarthrosis Research articles Congenital pseudarthrosis review articles Congenital pseudarthrosis PubMed articles Congenital pseudarthrosis PubMed Central articles Congenital pseudarthrosis 2023 articles Congenital pseudarthrosis 2024 articles Congenital pseudarthrosis Scopus articles Congenital pseudarthrosis impact factor journals Congenital pseudarthrosis Scopus journals Congenital pseudarthrosis PubMed journals Congenital pseudarthrosis medical journals Congenital pseudarthrosis free journals Congenital pseudarthrosis best journals Congenital pseudarthrosis top journals Congenital pseudarthrosis free medical journals Congenital pseudarthrosis famous journals Congenital pseudarthrosis Google Scholar indexed journals Osteomyelitis articles Osteomyelitis Research articles Osteomyelitis review articles Osteomyelitis PubMed articles Osteomyelitis PubMed Central articles Osteomyelitis 2023 articles Osteomyelitis 2024 articles Osteomyelitis Scopus articles Osteomyelitis impact factor journals Osteomyelitis Scopus journals Osteomyelitis PubMed journals Osteomyelitis medical journals Osteomyelitis free journals Osteomyelitis best journals Osteomyelitis top journals Osteomyelitis free medical journals Osteomyelitis famous journals Osteomyelitis Google Scholar indexed journals Bone tumors articles Bone tumors Research articles Bone tumors review articles Bone tumors PubMed articles Bone tumors PubMed Central articles Bone tumors 2023 articles Bone tumors 2024 articles Bone tumors Scopus articles Bone tumors impact factor journals Bone tumors Scopus journals Bone tumors PubMed journals Bone tumors medical journals Bone tumors free journals Bone tumors best journals Bone tumors top journals Bone tumors free medical journals Bone tumors famous journals Bone tumors Google Scholar indexed journals Fracture articles Fracture Research articles Fracture review articles Fracture PubMed articles Fracture PubMed Central articles Fracture 2023 articles Fracture 2024 articles Fracture Scopus articles Fracture impact factor journals Fracture Scopus journals Fracture PubMed journals Fracture medical journals Fracture free journals Fracture best journals Fracture top journals Fracture free medical journals Fracture famous journals Fracture Google Scholar indexed journals Tibia articles Tibia Research articles Tibia review articles Tibia PubMed articles Tibia PubMed Central articles Tibia 2023 articles Tibia 2024 articles Tibia Scopus articles Tibia impact factor journals Tibia Scopus journals Tibia PubMed journals Tibia medical journals Tibia free journals Tibia best journals Tibia top journals Tibia free medical journals Tibia famous journals Tibia Google Scholar indexed journals Angular deformities articles Angular deformities Research articles Angular deformities review articles Angular deformities PubMed articles Angular deformities PubMed Central articles Angular deformities 2023 articles Angular deformities 2024 articles Angular deformities Scopus articles Angular deformities impact factor journals Angular deformities Scopus journals Angular deformities PubMed journals Angular deformities medical journals Angular deformities free journals Angular deformities best journals Angular deformities top journals Angular deformities free medical journals Angular deformities famous journals Angular deformities Google Scholar indexed journals Neurofibromatosis articles Neurofibromatosis Research articles Neurofibromatosis review articles Neurofibromatosis PubMed articles Neurofibromatosis PubMed Central articles Neurofibromatosis 2023 articles Neurofibromatosis 2024 articles Neurofibromatosis Scopus articles Neurofibromatosis impact factor journals Neurofibromatosis Scopus journals Neurofibromatosis PubMed journals Neurofibromatosis medical journals Neurofibromatosis free journals Neurofibromatosis best journals Neurofibromatosis top journals Neurofibromatosis free medical journals Neurofibromatosis famous journals Neurofibromatosis Google Scholar indexed journals Traumatic fracture articles Traumatic fracture Research articles Traumatic fracture review articles Traumatic fracture PubMed articles Traumatic fracture PubMed Central articles Traumatic fracture 2023 articles Traumatic fracture 2024 articles Traumatic fracture Scopus articles Traumatic fracture impact factor journals Traumatic fracture Scopus journals Traumatic fracture PubMed journals Traumatic fracture medical journals Traumatic fracture free journals Traumatic fracture best journals Traumatic fracture top journals Traumatic fracture free medical journals Traumatic fracture famous journals Traumatic fracture Google Scholar indexed journals Iatrogenic injuries articles Iatrogenic injuries Research articles Iatrogenic injuries review articles Iatrogenic injuries PubMed articles Iatrogenic injuries PubMed Central articles Iatrogenic injuries 2023 articles Iatrogenic injuries 2024 articles Iatrogenic injuries Scopus articles Iatrogenic injuries impact factor journals Iatrogenic injuries Scopus journals Iatrogenic injuries PubMed journals Iatrogenic injuries medical journals Iatrogenic injuries free journals Iatrogenic injuries best journals Iatrogenic injuries top journals Iatrogenic injuries free medical journals Iatrogenic injuries famous journals Iatrogenic injuries Google Scholar indexed journals Stress fracture articles Stress fracture Research articles Stress fracture review articles Stress fracture PubMed articles Stress fracture PubMed Central articles Stress fracture 2023 articles Stress fracture 2024 articles Stress fracture Scopus articles Stress fracture impact factor journals Stress fracture Scopus journals Stress fracture PubMed journals Stress fracture medical journals Stress fracture free journals Stress fracture best journals Stress fracture top journals Stress fracture free medical journals Stress fracture famous journals Stress fracture Google Scholar indexed journals Femoral defects articles Femoral defects Research articles Femoral defects review articles Femoral defects PubMed articles Femoral defects PubMed Central articles Femoral defects 2023 articles Femoral defects 2024 articles Femoral defects Scopus articles Femoral defects impact factor journals Femoral defects Scopus journals Femoral defects PubMed journals Femoral defects medical journals Femoral defects free journals Femoral defects best journals Femoral defects top journals Femoral defects free medical journals Femoral defects famous journals Femoral defects Google Scholar indexed journals
Article Details
1. Introduction
Skeletal defects can be classified as primary or secondary defects according to their etiology. Primary bone defects result from high-energy trauma, which can produce an open fracture with extensive soft tissue damage, osseous comminution and even extrication of bone fragments. Secondary bone defects result from excision of pathological tissue. Pathologic processes involving the skeleton may be congenital, as in congenital pseudarthrosis of the tibia, or acquired, as in aseptic and septic nonunions, osteomyelitis and bone tumors [1]. Congenital pseudarthrosis of the tibia has an incidence of approximately one in 250,000 live births [2]. Once a true pseudarthrosis of the tibia develops, it cannot be expected to heal when treated by casting or bracing alone. Resection of the pseudarthrosis with reconstruction using a free vascularized bone grafts also has been described with good results [3]. Good preliminary results were also reported with the Ilizarov technique.
Nonunions are estimated to occur in 2% to 15% of all tibial fractures. The development of a tibial nonunion is closely related to the type and severity of the injury, but other factors may play a role, such as degree of fracture comminution, open fracture, degree of soft tissue injury, medical comorbidities, and patient lifestyle (tobacco use, nutritional status, medications). The free vascularized fibular graft (FVFG) is the one that has found the most widespread application in the management of large skeletal defects and will be reviewed in detail. It was not until 1975, that free transfer of a vascularized fibular graft using microvascular techniques became possible and was reported by Taylor et al. [4]. Approximately 3 months are necessary for incorporation of a graft in the upper extremity. In the lower extremity 4-5 months may be needed, with considerably earlier union, even in 2 months, in young patients operated for congenital pseudarthrosis of the tibia [1].
Finally, vascularised autografts are able to undergo hypertrophy resulting in increased strength. Unfortunately, the strength of a vascularized ?bular ?ap may be insuf?cient until hypertrophy occurs. This has been reported to occur on average 18 months after surgery. The Ilizarov external fixator is a labor-intensive, but very effective, tool in the treatment of nonunions. It is especially useful in nonunions associated with defects, shortening, and deformities. More traditional pin external fixators, using the Ilizarov principles, also can be used in the management of nonunions, especially when complicated by infection [5-6]. We treated large bone defects using both the FVFG and compression-distraction technique by Ilizarov external fixator to compare their efficacy.
2. Materials and Methods
We treated 18 cases with congenital pseudarthrosis and 27 cases with acquired large bone defects between 1998 and 2015. There were 13 males and 5 females among cases with congenital pseudarthrosis of the tibia and their average age was 7.4 (3-13). Among them, 16 cases were treated using the FVFG and 2 cases using the compression-distraction technique by Ilizarov external fixator. There were 11 cases (61.1%) with diagnosis of neurofibromatosis among them. All the patients had shortenings of affected limbs which were 7.8 cm (4-15 cm) and angular deformities of 25-45 degrees (in average 33 degrees) together with anterior bowling at the level of pseudarthrosis. The Boyd classification of congenital pseudoarthrosis of the tibia was performed based on initial X-ray film [2]. 13 cases belong to Boyd II type, 5 cases to Boyd III type and all cases with neurofibromatosis belong to Boyd II type. The compression-distraction technique by Ilizarov apparator was performed in 2 cases with two-site angular deformities and disalignment who had several conventional operations. In the group of the FVFG the unilateral external fixator was used in 11 cases and intramedullary nailing in 5 cases. In all the patients with congenital pseudarthrosis, soft tissue lengthening and correction of angular deformities were performed by bilateral or Ilizarov external fixator before the FVFG and the lengthening was done 1-2 cm longer than the normal limb. In case of considerable shortening of the operated limb after bone union compared to normal limb, additional lengthening was performed. In case of nonunion or partial bone absorption although enough healing period passed, the compression and secondary distraction were performed.
There were 20 males and 7 females among cases with acquired large bone defects and their average age was 27.9 (9-52). 8 patients had the FVFG and 19 patients had the compression- distraction technique by Ilizarov external fixator. 18 patients had tibial defect (15 from traumatic fracture and infection and 3 from hematogenous osteomyelitis), 6 patients femoral defect (all from traumatic fracture and infection) and 3 patients radial defect (all from hematogenous osteomyelitis). 3 surgical interventions had been done in average and 7 in maximum 8 patients who underwent the FVFG included 3 radial defects and 5 tibial defects and their average age was 17.2 (9-31). All the osteomyelitis healed completely and the bone defect was 9.7 cm (7.5-13.2 cm) in average. The stabilization after the FVFG had been done by unilateral external fixator. The period of bone defect ranged from 11 months to 7 years (2.5 years). 5 patients out of them had suffered from chronic osteomyelitis and wound treatment on alternative days. Angular deformities were present in 17 cases and the angle ranged from 5 to 30 degrees (14 degrees in average). The size of bone defect was 6.6 cm (4-20 cm). The complications include 2 tibial nerve and 4 peroneal nerve injuries. These injuries were not related with procedures by external fixator but with initial damages and iatrogenic injuries.The Ilizarov external fixator is applied to the affected limb, one or two 2 mm wires are transfixed through the proximal and distal fragments with wires tensioned by a calibrated wire-tensioning device and distraction is performed less than 1mm per day along the direction of the limb.
3. Result of Study
3.1 Congenital pseudarthrosis of tibia
The duration of elongation of soft tissue before performing the FVFG was 78.4 days in average and at this time the bone defect was 4.7 cm. The bone defect after resection of consolidated bone at the site of pseudarthrosis was 10.7 cm (8.4-15.6). The duration of the FVFG was 3.2 hours in average. In 12 out of 16 cases primary bone healing achieved. The duration of bone healing ranged from 3 to 13 months (7.3 months in average). The period of complete weight bearing ranged from 7 to 17 months (10.8 months in average). The follow-up period ranged from 1.5 to 13 years (5 years in average). 6 stress fractures occurred in 4 patients and early fractures developed 2 to 4 years after the FVFG. The fixation was done by unilateral external fixator and intramedullary nailing. Secondary fractures occurred at 5 and 8 years and bone healing achieved by unilateral external fixator. In the follow-up period shortening of the affected limb compared to the healthy limb was observed and it was 3.8cm in average (2-6 cm). In 6 cases distraction of the shortened leg was done using the Ilizarov technique and the length of distraction was 4.7 cm in average (3-6 cm).
Pseudarthrosis due to bone absorption developed in the proximal end of fibular graft in 2 out of 4 cases (3 cases by external fixator and 1 by intramedullary nailing) and in the distal end in one patient with anterior angular deformities of 15, 20, 5 degrees respectively. In case of 15 degrees deformity, under anesthesia the angular deformity had been corrected by manipulation and bone healing achieved by compression using unilateral apparatus. In case of 20 degrees deformity, the angular deformity had been corrected by surgical procedure and bone healing achieved by compression using unilateral apparatus. The length of shortening of the leg was 1 cm and 2 cm respectively. In case of 5 degrees deformity (intramedullary nailing) the nail had been removed, the region of pseudarthrosis resected, compression applied by unilateral apparatus with the shortening 2 cm. In one patient bone absorption progressed gradually at the proximal end of the graft and a half of the graft absorbed 6 months later.
One year after the FVFG, bone healing achieved by iliac bone graft and compression by external fixator. In this patient additional 6 cm lengthening had been done 6 years later. The period of bone healing ranged from 16 to 26 months in 4 cases in whom secondary bone healing achieved, and them of all were patients of with either neurofibromatosis. In addition, the complications observed during the follow-up include 5 cases of malunion with angular deformities (15-25 degrees), 3 cases of equinovarus and 2 cases of transient peroneal paralysis. In 2 cases of severe angular deformities, correction surgery had been performed and in 3 cases of equinovarus, correction had been done by elongation of calcaneal tendon or wedge osteotomy. In 2 cases of compression-distraction treatment the shortening of the leg was 8 cm and 15 cm respectively, and they were treated by bifocal compression-distraction technique. The duration of distraction was 62 days and 118 days respectively, and the duration of wearing Ilizarov apparator was 11 months and 16 months respectively. After that 2 months of cast immobilization performed followed by gradual ambulation. The period of full weight bearing ranged from 15 and 21 months.
OP: Operation; PA: Pseudoarthrosis; IN: Intramedullary Nailing; UEF: Unilateral External Fixator; CD: Compression-Distraction; AD: Angularn Deformity; TPNP: Temporary PNP; EV: Equinovarus
Table 1: Demographic Data of the Patients of congenital Pseudarthrosis.
HO: Hemotogenous Osteomyelitis; CF: Comminuted Fracture; Om: Osteomyelitis; R: Radius; U: Ulna; T: Tibia
Table 2: Demographic Data of the Patients of the Bone Defect and Shortening (FVFG).
3.2 Acquired bone defect
Initial bone healing was achieved in all cases of the FVFG and the period of bone healing ranged from 3.5 to 10 months. The period of hypertrophy in tibia ranged from 7 to 22 months. The younger the patient, the faster the hypertrophy and in elder patients the hypertrophy was late and also the period of complete weight bearing was late.
In the follow-up period up to 4 years the period of complete weight bearing was 14 months in average (8-22 months). In one case, stress fracture occurred 3 years after the FVFG and healed by external fixator.
The group of compression-distraction treatment by Ilizarov apparatus includes 13 tibial (5 cases with present osteomyelitis) and 2 femoral defects. The size of bone defect was 5.2 cm in average (1.5-3.7 cm), the shortening 2.5 cm in average (1.5-3.7 cm) and the period of bone distraction 82 days (55-112 days). The period of wearing external fixator was 10.7 months (7-14 months). At the end of compression both bone ends of pseudarthrosis site freshened with its frequency 1.7 times in case of osteomyelitis and 1.1 times in case of aseptic pseudarthrosis. The infection at wire site occurred in 7 out of 15 cases, but all improved by use of antibiotics and dressings. The period of full weight bearing was 12.2 months (9-17 months) postoperatively.
Om: Osteomyelitis; Fr: Fracture; TNP: Tibial nerve paralysis; PNP: Peroneal nerve paralysis; TPNP: Temporary PNP; EV: equinovarus; KA: Knee Ankylosis
Table 3: Demographic Data of the Patient of the Bone Defect and Shortening (Compression-Distraction).
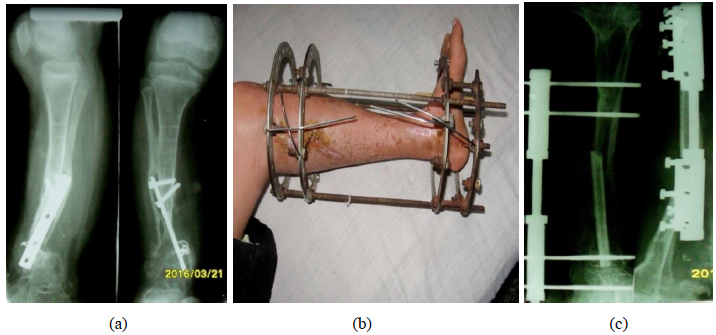
Figure 1: (Patient no. 15) (a) Congenital pseudarthrosis in female aged 7, three intramedullary nailings and plate and screw procedure, the length of bone defect 15 cm; (b) Lengthening of soft tissue by Ilizarov apparatus; (c) Stabilization by unilateral external fixator after the FVFG.
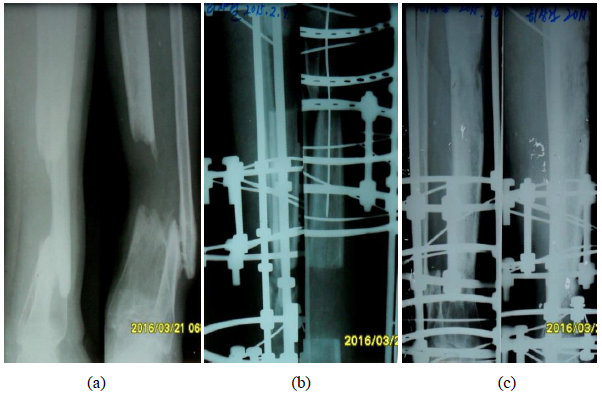
Figure 2: (a) X-ray film of right tibial defect after resection of sequestrum infected post open comminuted fracture in male aged 43. The length of defect 6.5 cm, shortening of limb 2 cm; (b) Compression-distraction by Ilizarov apparatus; (c) Consolidation of callus after completion of compression and distraction.
During the follow-up period (3-10 years), 7 fractures occurred in 5 cases. 3 fractures occurred by motor accidents and 4 were stress fractures. Fractures at the level of wire insertion occurred in 2 cases within 1 year after removal of external fixator. Complications included 2 cases with tibial nerve palsy and 4 cases with peroneal nerve palsy.
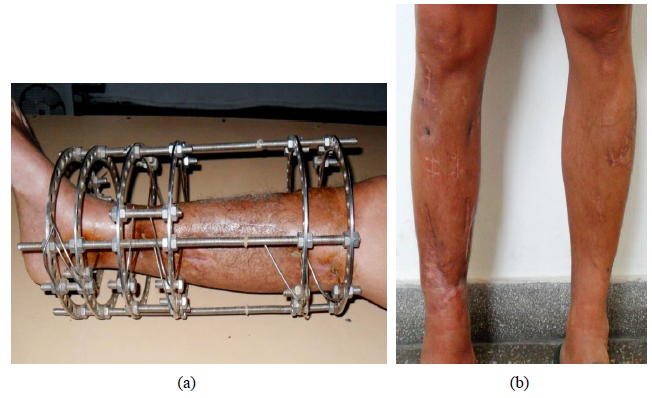
Figure 3: (a) Finding of compression and distraction of 8.5cm by Ilizarov apparatus; (b) Full weight bearing 13 months post operation.
2 peroneal nerve palsies recovered gradually after removal of external fixators but 2 iatrogenic tibial and 2 peroneal nerve palsies not recovered. For them transfer of tibialis posterior tendon and ankle arthrodesis were carried out to improve disability. In 7 cases ROM of the knee joint was limited but after removal of external apparatus knee flexion recovered up to mean 75 degrees. Equinovarus deformity of the ankle occurred in 5 cases. Because of no improvement through rehabilitation elongation of Achilles tendon in all cases and wedge osteotomy in 2 cases performed. 11 out of 15 patients returned to their original jobs and 4 to less burden jobs. The length of distraction in 4 cases with shortening of femur ranged from 6.5 to 22 cm and in case of 22 cm long bone defect, bifocal compression-distraction was performed. The distraction period ranged from 92 to 190 days and in 1 case elongation of Achilles tendon performed and knee joint ankylosed. The period of full weight bearing ranged from 8 to 15 months.
4. Discussion
A skeletal defect represents loss of osseous tissue, which alters the anatomy and architecture, the biomechanical properties and the functional ability of the affected bone [1]. Congenital pseudarthrosis is a specific type of nonunion that at birth is either present or incipient. Congenital pseudarthrosis most commonly involves the distal half of the tibia and often that of the fibula in the same limb [2]. In the past congenital pseudarthrosis of the tibia was treated by bone grafting or amputation. Osseous union is more difficult to obtain in this condition. In congenital anomalies, the soft tissues are the greatest obstacle to lengthening. Generally, this surgical intervention should precede skeletal maturity since the soft tissues are more resistant to lengthening later. Vascularized fibular grafts may be indicated for pseudarthroses with gaps of more than 5 cm and for pseudarthroses in which multiple surgical procedures have failed [7, 8]. The use of free vascularized fibular grafts has been advocated by some for treatment of osteonecrosis of the femoral head [9-11]. Others have used it to treat bone defects associated with tumor resections [7, 12, 13].
The straight configuration and the anatomic size and shape of the fibula make it match exactly the forearm bones and fit into the medullary canal of the humerus, the femur and the tibia. Therefore, it constitutes an ideal graft for extremity reconstruction. A posterior approach for graft harvesting was originally described by Taylor, but the lateral approach, as described by Gilbert, has found widespread application. Stabilization of the fibula can be accomplished by a variety of osteosynthesis techniques. Osteosynthesis techniques that have been employed include plate, external and intramedullary fixation. Furthermore, hypertrophic bone fractures have been reported and therefore some advocate protecting the vascularised fibular flap in the lower limb for the first few years after implantation [9, 12, 14]. The Ilizarov external fixator continues to be an effective and versatile method for treatment of difficult nonunions complicated by complex deformity, infection, and bone loss [10, 11, 15]. One advantage of external fixation is that it is relatively noninvasive and does not disturb soft tissues surrounding the nonunion. Because of the frequency of infection in tibial nonunions, external fixation is an attractive option. External fixation allows correction of multiple deformities and bridging of large fracture gaps by bone transport techniques [16].
High rates of union have been reported with the Ilizarov method, especially in complicated nonunions. The union rate of vascularized fibular graft is reported in the literature to be 74-100% [17]. The period of union in our patients who obtained primary union was 7.3 months in average, which coincides with data that vascularized fibular graft healed within 10 months. The period of full weight bearing is 12.8 months and early recovery is possible. The failure rates of vascularized fibular graft are reported in the literatures to be 15.4%. Postoperative complications are not avoidable and include fractures, pseudarthrosis and infections [18-24]. In our study, pseudarthrosis and partial bone absorption developed in 25% of patients. The period of bone healing in patients with these complications ranged from 16 months to 26 months and was significantly longer than in patients who obtained primary healing. Other complications include malunion (32.2%), equinovarus (18.7%) and temporary peroneal nerve palsy (12.5%) and they were treated by rehabilitations and surgical techniques. The rate of stress fracture ranged from 7.7% to 40%.
We applied stabilizations including casts after removing the external fixators and allowed full weight bearing when the hypertrophy of the graft reached the bone thickness of the recipient area. During the follow-up from one and half to 5 years the rate of stress fracture in our study was 37.5% and 2 refractures occurred in 2 cases. In 6 cases limb-length discrepancy developed during growth and distraction by Ilizarov apparatus performed. The treatments of congenital pseudarthrosis by compression-distraction technique are reported and techniques such as compression-distraction technique of pseudarthrosis sites and distraction after corticotomy of proximal tibia are widely used. The mean treatment period was 5.6 months and angular deformities at pseudarthrosis sites were fully corrected [25]. The mean treatment period in 2 cases with pseudarthrosis we treated was 15 months and 21 months, respectively, and it is thought to be due to severe osteoporosis and longer period of bone formation and consolidation. The FVFGs in patients with acquired bony defects showed better results and more rapid bone healing compared to patients with congenital pseudarthrosis [26-29]. On the contrary hypertrophy took a longer time and overall longer treatment time. It is sure that there are some differences as per the age.
The history of pseudarthrosis in patients with acquired bony defects ranged from 5 to 10 years and full weight bearing and recovery of working ability gained in 74.8% of patients treated by Ilizarov technique. According to the literature, the bony defects ranging from 1 to 23 cm have been treated by Ilizarov apparatus with no deformity and limb shortening and good functioning in 85-91% of patients obtained and treatment period ranged from 9 to 16 months. The most important early complications in our study include angular deformity and equinovarus and late complication was stress fracture. Bone formation depends greatly on nutritional status and appetite, which are important factors to determine treatment results. The FVFG in young patients with bony defects including congenital pseudarthrosis is effective option, and Ilizarov technique is reliable and useful treatment for patients with complex deformities including infective bone defects and pseudarthrosis.
References
- Malizos KN, Zalavras CG, Dailiana Z, et al. The Free Vascularized Fibula Graft. In Eds.: Malizos KN. Reconstructive Microsurgery. Georgetown. Landes Bioscience (2003): 154-169.
- Canale ST, Beaty JH. Campbell’s operative orthopaedics. St Louis: Mosby (2012): 1018-1022, 2977-2998.
- Brown KLB. Staged treatment of severe congenital pseudoarthrosis of the tibia with limb lengthening and free vascularized fibular graft. Pediatr Orthop Society Meeting. Toronto (1987): 17-20.
- Taylor GI, Miller DH, Ham FJ. The free vascularised bonegraft. A clinical extension of microvascular techniques. PRS 55 (1975): 533-544.
- Ilizarov GA, Ledyaev VI. The replacement of long tubular bone defects by lengthening distraction osteotomy of one of the fragments. Clin Orthop Relat Res 280 (1992): 7-10.
- Paley D, Maar DC. Ilizarov bone transport treatment for tibialdefects. J Orthop Trauma 14 (2000): 76-85.
- Belt PJ, Dickinson IC, Theile DR. Vascularised free fibular flap in bone resection and reconstruction. Br J Plast Surg 58 (2005): 425-430.
- Falder S, Sinclair JS, Rogers CA, et al. Long-term behavior of the free vascularised fibula following reconstruction of large bony defects. Br J Plast Surg 56 (2003): 571-584.
- Arai K, Toh S, Tsubo K, et al. Complications of vascularized fibula graft for reconstruction of long bones. Plast and Reconstr Surgery 109 (2002): 2301-2306.
- Croce F, Risorto M, Coviello M, et al. Vascularised fibulatransplant: Technique, early results, indications and limitations. Ital J Orthop Traumatol 12 (1986): 447-454.
- Baschera D, Kingwell D, Wren M, et al. A holistic perspective of patients’ lives post-Ilizarov external fixation. ANZ J Surg 84 (2014): 776-780.
- Pollock R, Stalley P, Lee K, et al. Free vascularized fibula grafts in limb-salvage surgery. J Reconstr Microsurg 21 (2005): 79-84.
- Hsu RWW, Wood MB, Sim FH, et al. Free vascularized fibular grafting for reconstruction after tumour resection. J Bone Joint Surg Br 79 (1997): 36-42.
- Lovisetti G, Sala F. Clinical strategies at the docking site of distraction osteogenesis: Are open procedures superior to the simple compression of Ilizarov? Injury, Int. J. Care Injured 44 (2013): 1, 58-62.
- Abdel-Aal AM. Ilizarov bone transport for massive tibial bone defects. Orthop 29 (2006): 70-74.
- Aaronovich AM, Shlyachov VI, Payevski SA, et al. Rehabilitation by Ilizarov technique of patients with bony defects of the tibia complicated by chronic osteomyelitis.In Experimental Theoretical and Clinical Aspects of Transosseous Osteosynthesis Developed at the KNIIEKOT, 2nd International Conference Abstracts, Kurpn, USSR 74 (1986): 3-5.
- Chew WYC, Low CK, Tan SK. Long-term results of free vascularized fibular graft. Clin Orthop 311 (1995): 258-261.
- Brunelli G, Vigasio A, Battiston B, et al. Free microvascular fibular versus conventional bone grafts. Int Surg 76 (1991): 33-42.
- Manfrini M. The role of vascularized fibula in skeletal reconstruction. La Chirurgia degli Organi di Movimento 88 (2003): 137-142.
- Pollock R, Stalley P, Lee K, et al. Free vascularized fibula grafts in limb-salvage surgery. J Recons Microsurgery 21 (2005): 79-84.
- Tsuchiya H, Tomita K. Distraction osteogenesis for treatment of bone loss in the lower extremity. J Orthop Sci 8 (2003): 116-124.
- Rozbruch SR, Weitzman AM, Tracey Watson J, et al. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 20 (2006): 197-205.
- Thomas H, Mccoy JR, Kim HJ, et al. Bilateral Fibular Graft: Biological Reconstruction after Resection of Primary Malignant Bone Tumors of the Lower Limb. J Surg Oncology 107 (2013): 343-352.
- Paley D. Problems, Obstacles, and Complications of Limb Lengthening by the Ilizarov Technique Clin Orthop and Relat Res 250 (1990): 81-104.
- Paley D, Catagni M, Argnani F, et al. Treatment of Congenital Pseudoarthrosis of the Tibia Using the Ilizarov Technique Clin Orthop and Relat Research 280 (1992): 81-93.
- Robert RS, Weitzman AM, Tracey WJ, et al. Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 20 (2006): 197-205.
- Dagher F, Roukoz S. Compound tibial fractures with bone loss treated by the Ilizarov technique. J Bone Joint Surg Br 73 (991): 316-321.
- Ghert M, Colterjohn N, Manfrini M. The use of free vascularized fibular grafts in skeletal reconstruction for bone tumors in children. J Am Academy of Orthop Surgeons 15 (2007): 577-587.
- Gao YS, Chen SB, Jin DX, et al. Modified surgical techniques of free vascularized fibular grafting for treatment of the osteonecrosis of femoral head: Results from a series of 407 cases. Microsurg 33 (2013): 646-651.
