Tophaceous Gout In a Patient of Thalassemia Intermedia: A Case Report
Article Information
Dr Shweta Priti, Dr Rashmi Dixit*, Dr Prerana Saraswat, Dr Anju Garg, Dr Gaurav Pradhan
Department of Radiodiagnosis, Maulana Azad Medical College, New Delhi, India.
*Corresponding Author: Dr Rashmi Dixit, Department of Radiodiagnosis, Maulana Azad Medical College, New Delhi, India.
Received: 03 July 2022; Accepted: 14 July 2022; Published: 19 January 2023
Citation:
Dr Shweta Priti, Dr Rashmi Dixit*, Dr Prerana Saraswat, Dr Anju Garg, Dr Gaurav Pradhan. Tophaceous Gout In A Patient of Thalassemia Intermedia: A Case Report. Journal of Radiology and Clinical Imaging. Journal of Radiology and Clinical Imaging 6 (2023): 01-04.
View / Download Pdf Share at FacebookAbstract
Thalassemia is an important hemoglobinopathy that poses a significant burden on the Indian health system. It has a prevalence of ~3-4 % in the Indian population. Thalassemia has an autosomal recessive inheritance and co-inheritance with haemoglobin variants like HbE is not uncommon. Here we present an interesting case of tophaceous gout in a patient of thalassemia intermedia.
Case Report articles
metacarpophalangeal join articles metacarpophalangeal join Research articles metacarpophalangeal join review articles metacarpophalangeal join PubMed articles metacarpophalangeal join PubMed Central articles metacarpophalangeal join 2023 articles metacarpophalangeal join 2024 articles metacarpophalangeal join Scopus articles metacarpophalangeal join impact factor journals metacarpophalangeal join Scopus journals metacarpophalangeal join PubMed journals metacarpophalangeal join medical journals metacarpophalangeal join free journals metacarpophalangeal join best journals metacarpophalangeal join top journals metacarpophalangeal join free medical journals metacarpophalangeal join famous journals metacarpophalangeal join Google Scholar indexed journals X -Ray articles X -Ray Research articles X -Ray review articles X -Ray PubMed articles X -Ray PubMed Central articles X -Ray 2023 articles X -Ray 2024 articles X -Ray Scopus articles X -Ray impact factor journals X -Ray Scopus journals X -Ray PubMed journals X -Ray medical journals X -Ray free journals X -Ray best journals X -Ray top journals X -Ray free medical journals X -Ray famous journals X -Ray Google Scholar indexed journals erythrocytes articles erythrocytes Research articles erythrocytes review articles erythrocytes PubMed articles erythrocytes PubMed Central articles erythrocytes 2023 articles erythrocytes 2024 articles erythrocytes Scopus articles erythrocytes impact factor journals erythrocytes Scopus journals erythrocytes PubMed journals erythrocytes medical journals erythrocytes free journals erythrocytes best journals erythrocytes top journals erythrocytes free medical journals erythrocytes famous journals erythrocytes Google Scholar indexed journals microscopic haematuria articles microscopic haematuria Research articles microscopic haematuria review articles microscopic haematuria PubMed articles microscopic haematuria PubMed Central articles microscopic haematuria 2023 articles microscopic haematuria 2024 articles microscopic haematuria Scopus articles microscopic haematuria impact factor journals microscopic haematuria Scopus journals microscopic haematuria PubMed journals microscopic haematuria medical journals microscopic haematuria free journals microscopic haematuria best journals microscopic haematuria top journals microscopic haematuria free medical journals microscopic haematuria famous journals microscopic haematuria Google Scholar indexed journals renal tubular dysfunction articles renal tubular dysfunction Research articles renal tubular dysfunction review articles renal tubular dysfunction PubMed articles renal tubular dysfunction PubMed Central articles renal tubular dysfunction 2023 articles renal tubular dysfunction 2024 articles renal tubular dysfunction Scopus articles renal tubular dysfunction impact factor journals renal tubular dysfunction Scopus journals renal tubular dysfunction PubMed journals renal tubular dysfunction medical journals renal tubular dysfunction free journals renal tubular dysfunction best journals renal tubular dysfunction top journals renal tubular dysfunction free medical journals renal tubular dysfunction famous journals renal tubular dysfunction Google Scholar indexed journals Fine Needle Aspiration Cytology articles Fine Needle Aspiration Cytology Research articles Fine Needle Aspiration Cytology review articles Fine Needle Aspiration Cytology PubMed articles Fine Needle Aspiration Cytology PubMed Central articles Fine Needle Aspiration Cytology 2023 articles Fine Needle Aspiration Cytology 2024 articles Fine Needle Aspiration Cytology Scopus articles Fine Needle Aspiration Cytology impact factor journals Fine Needle Aspiration Cytology Scopus journals Fine Needle Aspiration Cytology PubMed journals Fine Needle Aspiration Cytology medical journals Fine Needle Aspiration Cytology free journals Fine Needle Aspiration Cytology best journals Fine Needle Aspiration Cytology top journals Fine Needle Aspiration Cytology free medical journals Fine Needle Aspiration Cytology famous journals Fine Needle Aspiration Cytology Google Scholar indexed journals purine metabolism articles purine metabolism Research articles purine metabolism review articles purine metabolism PubMed articles purine metabolism PubMed Central articles purine metabolism 2023 articles purine metabolism 2024 articles purine metabolism Scopus articles purine metabolism impact factor journals purine metabolism Scopus journals purine metabolism PubMed journals purine metabolism medical journals purine metabolism free journals purine metabolism best journals purine metabolism top journals purine metabolism free medical journals purine metabolism famous journals purine metabolism Google Scholar indexed journals Imaging articles Imaging Research articles Imaging review articles Imaging PubMed articles Imaging PubMed Central articles Imaging 2023 articles Imaging 2024 articles Imaging Scopus articles Imaging impact factor journals Imaging Scopus journals Imaging PubMed journals Imaging medical journals Imaging free journals Imaging best journals Imaging top journals Imaging free medical journals Imaging famous journals Imaging Google Scholar indexed journals extramedullary hematopoiesis articles extramedullary hematopoiesis Research articles extramedullary hematopoiesis review articles extramedullary hematopoiesis PubMed articles extramedullary hematopoiesis PubMed Central articles extramedullary hematopoiesis 2023 articles extramedullary hematopoiesis 2024 articles extramedullary hematopoiesis Scopus articles extramedullary hematopoiesis impact factor journals extramedullary hematopoiesis Scopus journals extramedullary hematopoiesis PubMed journals extramedullary hematopoiesis medical journals extramedullary hematopoiesis free journals extramedullary hematopoiesis best journals extramedullary hematopoiesis top journals extramedullary hematopoiesis free medical journals extramedullary hematopoiesis famous journals extramedullary hematopoiesis Google Scholar indexed journals Thalassemia articles Thalassemia Research articles Thalassemia review articles Thalassemia PubMed articles Thalassemia PubMed Central articles Thalassemia 2023 articles Thalassemia 2024 articles Thalassemia Scopus articles Thalassemia impact factor journals Thalassemia Scopus journals Thalassemia PubMed journals Thalassemia medical journals Thalassemia free journals Thalassemia best journals Thalassemia top journals Thalassemia free medical journals Thalassemia famous journals Thalassemia Google Scholar indexed journals
Article Details
1. Introduction
Thalassemia is an important hemoglobinopathy that poses a significant burden on the Indian health system. It has a prevalence of ~3-4 % in the Indian population. Thalassemia has an autosomal recessive inheritance and co-inheritance with haemoglobin variants like HbE is not uncommon[1]. There occurs a defect in globin component in haemoglobin in red blood cells with resultant ineffective erythropoiesis and hemolysis[2]. Because of high cell turnover owing to chronic haemolysis, hyperuricemia is not uncommon[2]. However, presence of tophaceous gout, is distinctly unusual with only few isolated case reports available so far.
Here we present an interesting case of tophaceous gout in a patient of thalassemia intermedia.
2. Case History
A 31 year old male presented to medicine out patient department with complaints of multiple joint swellings involving first the little finger of right hand, followed by involvement of right 5th toe and later both ankles (Figure 1A-B). The swellings in right hand and feet were nodular, non-tender, hard in consistency and non-mobile without any loss of sensation. The patient also had pallor, frontal bossing with depressed nasal bridge.
Following this the patient was investigated with Xray of hand, foot and skull which showed diffuse osteopenia with coarsened trabeculae, medullary space widening with punched out lytic periarticular lesions with overhanging margins involving distal interphalangeal joint of right fifth toe, 2nd metacarpophalangeal joint (MCP) and proximal interphalangeal (PIP) joints of index and little finger with associated soft tissue swelling; Xray skull showed widened diploic space, coarsened trabeculae with a typical “hair on end appearance”(Figure 2A-C).
The patient was then admitted for detailed examination. On general examination, patient was conscious and oriented to time, place, and person. His vitals were stable with pulse rate of 76/minute, blood pressure 102/56mmHg and respiratory rate 22/minute. The patient was also noted to have scoliosis. Nodules were seen on bilateral earlobes. On auscultation, bilateral air entry was normal and both heart sounds, S1 and S2 were heard with presence of murmur in mitral and tricuspid areas. Massive splenomegaly was found on per abdominal examination. On probing, the patient gave history of chronic anaemia, having received 3 blood transfusions over the past year.
Routine hemogram revealed anaemia with haemoglobin of 5.2 g/dl with haematocrit of 7.7 and decreased red cell counts(2.9cells/ cubic mm). In addition, hyperbilirubinemia(3.3md/dl) was seen with mildly reduced serum calcium(8mg/dl) and raised serum phosphate levels(5.2mg/dl). Along with these, there was significantly high serum uric acid levels(10mg/dl). However, the renal function test was within normal limits with blood urea of 21mg/dl and serum creatinine of 0.8mg/dl. The peripheral blood smear showed hypochromic microcytic cells, tear drop cells, fragmented and target cells with marked degenerative changes in white blood cells. Ultrasonography of abdomen was also done which demonstrated hepatosplenomegaly.
Xray dorsolumbar spine was done in view of scoliosis which revealed diffuse osteopenia with biconcave appearance of vertebral bodies and partial collapse at multiple levels in lumbar spine causing scoliotic deformity with lobulated paravertebral soft tissue shadow along the lower dorsal spine on left side, due to extramedullary hematopoiesis (Figure 3 A and B). All the above findings suggested a provisional diagnosis of hemolytic anemia with gout.
Diagnosis of thalassemia was confirmed by High Performance Liquid Chromatography (HPLC) done subsequently which revealed HbF of 14.6%, HbA2 of 76.8% and HbA of 10 % suggesting possibility of double heterogenous for HbE and beta-thalassemia (Figure 4).
Fine Needle Aspiration Cytology(FNAC) from swelling in right little finger and right toe was also done which showed features of gouty tophous(numerous brownish needle like crystals ) which were confirmed on polarized light.
Based on patient history with supportive laboratory and histopathological findings, a final diagnosis of thalassemia intermedia with multiple tophaceous deposits was made.
Patient was started on tablet febuxostat 40mg for managing hyperuricemia, symptomatic treatment was given along with it. Packed cells were also transfused to manage anaemia. Patient condition improved and was discharged on medication.

FIGURE : 1 A-B: (A)Multiple joint swelling in right hand involving second and third metacarpophalangeal joints and interphalangeal joints of fifth finger(marked with arrows). (B) Swelling in interphalangeal joints of right fifth toe(marked with arrow).

FIGURE: 2 A-B: Plain radiograph of right hand PA view(A) and both feet AP view(B) shows diffuse osteopenia with coarsened trabeculae and medullary space widening. Punched out lytic periarticular lesions with overhanging margins in right 2nd metacarpophalangeal joint and proximal interphalangeal joints of index, little finger and right fifth toe with associated soft tissue swelling(marked with arrow in A and B).
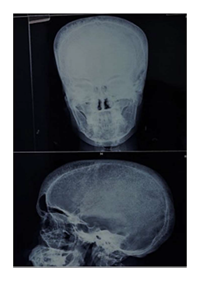
FIGURE: 2 C: Xray skull (Anteroposterior and Lateral views) show widening of diploic space. Coarsened trabeculae producing a typical “hair on end appearance” also seen.
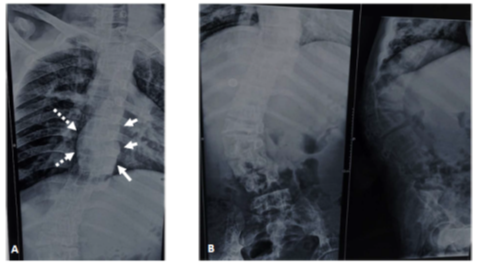
FIGURE 3 A-B: Xray dorsolumbar spine(Anteroposterior and lateral views) showing diffuse osteopenia with biconcave appearance of vertebral bodies and partial collapse at multiple levels in lumbar spine causing scoliotic deformity. Lobulated paravertebral soft tissue shadow also seen along the lower dorsal spine on left side suggestive of extra-medullary hematopoiesis(marked with arrows in A). The aortic shadow is seen to the right of spine consequent to scoliosis(marked with dashed arrows in A).
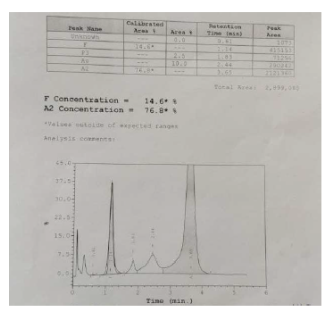
FIGURE 4: High performance liquid chromatography showing levels of HbF at 14.6%, HbA2 at 76.8% and HbA at10 % suggesting possibility of double heterogenous for HbE and beta-thalassemia.
3. Discussion
Beta thalassemia is a genetic condition characterized by decreased beta chain synthesis and inadequate HbA formation. However, synthesis of alpha chain continues unimpaired, forming unstable aggregates in red cells and causing inadequate and ineffective erythropoiesis. Such red cells undergo destruction in marrow itself or in spleen. There is increased destruction of immature erythrocytes (containing nuclei) which results in increased uric acid production, an end product of purine metabolism (present in nucleic acids). The uric acid has tendency to get crystalized in various tissues when the serum is supersaturated, at about 7.0mg/dl, and above this level there is increased risk of gout or renal stones[3]. Although hyperuricemia is common in thalassemia, clinical gout is distinctly uncommon. However, the raised serum uric acid levels in thalassemia patients at times leads to hyperuricosuria which results in microscopic haematuria, renal tubular dysfunction and GFR abnormalities[2,4]. The deranged renal function and prolonged hyperuricemia finally leads to development of gouty arthritis. In our case, however, gout was present although renal function tests were within normal limits. According to previous literature only small percentage of patients of thalassemia with hyperuricemia develop gout. Few cases have been reported featuring clinically proven tophaceous gout in thalassemia patient, all of them surviving to their middle age, which is an important factor, as it gives adequate time to develop gout[5].
On imaging gout is seen as arthritis most commonly involving metatarsophalangeal joints, midfoot, hand and wrists. Imaging findings include erosion of phalanges, punched out lytic lesion involving joints with sclerotic margins and overhanging bony edges and associated soft tissue swelling. Gold standard for diagnosis is the presence of birefringent monosodium urate crystals under polarized light which can be established by biopsy or FNAC from the soft tissue swelling or from joint effusion aspirate[6,7], a feature seen in our case.
Hemolytic anemia like thalassemia also leads to erythroid hyperplasia and reticulocytosis in bone marrow which on radiographs is seen as coarsened trabeculae and thinned out cortex with widening of marrow spaces as in this case. The patient also showed extramedullary hematopoiesis (EMH) on radiographs. The decreased red cell count is a stimulator for erythropoietin production which in turn leads to EMH mostly seen in imaging as liver and spleen enlargement or paravertebral soft tissue swelling[8]. According to a study by Abolhasani Foroughi, Amin et al EMH is more commonly seen in thalassemia intermedia than thalassemia major, probably due to long time treatment with blood transfusion in thalassemia major patients, with inhibits EMH[9].
4. Conclusion
Patients with thalassemia may develop hyperuricemia due to increased cell turnover. A small percentage of these patients develop gout which may occur due to renal dysfunction. In presence of relevant clinical-laboratory and imaging findings, the diagnosis of secondary gout in thalassemia patients should be considered and managed accordingly.
References
- Colah R, Italia K, Gorakshakar A. Burden of thalassemia in India: The road map for control. Pediatr Hematol Oncol J. 2 (2017): 79–84.
- Chaloemwong J, Tantiworawit A, Rattanathammethee T Hyperuricemia, urine uric excretion, and associated complications in thalassemia patients. Ann Hematol. 98 (2019): 1101–1110.
- Deborah Campano G, Holmes EW. Hyperuricemia and Gout. Med Clin North Am. 70 (1986): 419–436.
- Demosthenous C, Vlachaki E, Apostolou C. Beta-thalassemia: Renal complications and mechanisms: a narrative review. Hematology. 24 (2019): 426-438.
- Paik CH, Alavi I, Dunea G. Thalassemia and Gouty Arthritis. JAMA. 213 (1970): 296–297
- Harris MD, Siegel LB, Alloway JA. Gout and hyperuricemia. Am Fam Physician. 59 (1999): 925–934.
- Chowalloor PV, Siew TK, Keen HI. Imaging in gout: A review of the recent developments. Therapeutic Advances in Musculoskeletal Disease. 6 (2014): 131-143.
- Mishra V, Sorabjee J, Mirgh S. Tophaceous gout in thalassemia intermedia: a rare association. Oxf Med Case Rep. 5 (2016): 105–106.
- Abolhasani Foroughi A, Ghaffari H, Haghpanah SComparative study of radiographic and laboratory findings between Beta thalassemia major and Beta thalassemia intermedia patients with and without treatment by hydroxyurea. Iranian Red Crescent medical journal, 17 (2015): 23607.
