The Benefits of Radical Laparoscopic Surgery and a Modified Endometriosis Health Profile-36 (EHP-36) on Quality of Life
Article Information
Ekine A A1*, Fulop I1, Rucz A1, Koppan A2, Siklos P1, Koppan M3
1Department of Obstetrics and Gynaecology, Robert Karoly Private Hospital, Budapest, Hungary
2Faculty of Health Sciences, University of Pecs, Pecs, Hungary
3Department of Obstetrics and Gynaecology, University of Pecs, Pecs, Hungary
*Corresponding author: Atombosoba Adokiye Ekine, Department of Obstetrics and Gynaecology, Robert Károly Private Hospital, Budapest, Hungary
Received: 23 August 2020; Accepted: 02 September 2020; Published: 14 September 2020
Citation:
Ekine A A, Fulop I, Rucz A, Koppan A, Siklos P, Koppan M. The Benefits of Radical Laparoscopic Surgery and a Modified Endometriosis Health Profile-36 (EHP-36) on Quality of Life. Journal of Women’s Health and Development 3 (2020): 379-397.
View / Download Pdf Share at FacebookAbstract
Objective: This study investigates the outcomes for women up to 2 years after radical laparoscopic excision of endometriosis, and its effect on quality of life (QoL) and wellbeing using a modified Endometriosis Health Profile-36 questionnaire (EHP-36).
Design: A prospective cohort clinical study.
Setting: Robert Károly Hospital, Budapest, Hungary, Endoscopic Unit.
Population: Eighty-seven patients with proven investigative signs, symptoms and complaints of invasive endometriosis undergoing hysterolaparoscopic surgery in the hospital between 1 January 2017 and 31 December 2018.
Method: This study proscribes the use of questionnaires on patient’s quality of life and wellbeing with postoperative follow-up (for 6, 12 and 24 months).
Result: All 87 patients completed the questionnaires (response rate was 100%). Mean age was 34.2 ± 5.9 years; the average age of onset of endometriosis was 24.5 ± 5.710 years (15–37). The majority of patients (n = 65, 74.7%) were in stages III and IV. A total of 72 patients (82.76%) frequently described their pain as a pricking pain. The NRS-11 pain score reduced from 94.8% with moderate to severe pain preoperatively to 18.4% with mild pain postoperatively. There was a significant improvement in the QoL in this regard (p <0.001). The VAS pain score decreased from 8 ± 2.11 (86.0%) moderate to severe pain preoperatively to 0.47 ± 1.24 (93.1%) negligible to no pain postoperatively (p <0.001). 58.45% (32/61) of women with infertility, became pregnant, live birth was 77.4% (24/61). Perception of QoL before surgery as very bad in 89.6% (78/87) of women and the perception of QoL significantly improved in 93.1% (81/87) of women after surgery. General wellbeing was rated very low by 93.1% (81/87) of women before surgery.
Keywords
Endometriosis, Laparoscopic surgery, Infertility, EHP-36 Questionnaire, Quality of life
Endometriosis articles Endometriosis Research articles Endometriosis review articles Endometriosis PubMed articles Endometriosis PubMed Central articles Endometriosis 2023 articles Endometriosis 2024 articles Endometriosis Scopus articles Endometriosis impact factor journals Endometriosis Scopus journals Endometriosis PubMed journals Endometriosis medical journals Endometriosis free journals Endometriosis best journals Endometriosis top journals Endometriosis free medical journals Endometriosis famous journals Endometriosis Google Scholar indexed journals Infertility articles Infertility Research articles Infertility review articles Infertility PubMed articles Infertility PubMed Central articles Infertility 2023 articles Infertility 2024 articles Infertility Scopus articles Infertility impact factor journals Infertility Scopus journals Infertility PubMed journals Infertility medical journals Infertility free journals Infertility best journals Infertility top journals Infertility free medical journals Infertility famous journals Infertility Google Scholar indexed journals Laparoscopic surgery articles Laparoscopic surgery Research articles Laparoscopic surgery review articles Laparoscopic surgery PubMed articles Laparoscopic surgery PubMed Central articles Laparoscopic surgery 2023 articles Laparoscopic surgery 2024 articles Laparoscopic surgery Scopus articles Laparoscopic surgery impact factor journals Laparoscopic surgery Scopus journals Laparoscopic surgery PubMed journals Laparoscopic surgery medical journals Laparoscopic surgery free journals Laparoscopic surgery best journals Laparoscopic surgery top journals Laparoscopic surgery free medical journals Laparoscopic surgery famous journals Laparoscopic surgery Google Scholar indexed journals EHP-36 Questionnaire articles EHP-36 Questionnaire Research articles EHP-36 Questionnaire review articles EHP-36 Questionnaire PubMed articles EHP-36 Questionnaire PubMed Central articles EHP-36 Questionnaire 2023 articles EHP-36 Questionnaire 2024 articles EHP-36 Questionnaire Scopus articles EHP-36 Questionnaire impact factor journals EHP-36 Questionnaire Scopus journals EHP-36 Questionnaire PubMed journals EHP-36 Questionnaire medical journals EHP-36 Questionnaire free journals EHP-36 Questionnaire best journals EHP-36 Questionnaire top journals EHP-36 Questionnaire free medical journals EHP-36 Questionnaire famous journals EHP-36 Questionnaire Google Scholar indexed journals Quality of life articles Quality of life Research articles Quality of life review articles Quality of life PubMed articles Quality of life PubMed Central articles Quality of life 2023 articles Quality of life 2024 articles Quality of life Scopus articles Quality of life impact factor journals Quality of life Scopus journals Quality of life PubMed journals Quality of life medical journals Quality of life free journals Quality of life best journals Quality of life top journals Quality of life free medical journals Quality of life famous journals Quality of life Google Scholar indexed journals chronic articles chronic Research articles chronic review articles chronic PubMed articles chronic PubMed Central articles chronic 2023 articles chronic 2024 articles chronic Scopus articles chronic impact factor journals chronic Scopus journals chronic PubMed journals chronic medical journals chronic free journals chronic best journals chronic top journals chronic free medical journals chronic famous journals chronic Google Scholar indexed journals economic articles economic Research articles economic review articles economic PubMed articles economic PubMed Central articles economic 2023 articles economic 2024 articles economic Scopus articles economic impact factor journals economic Scopus journals economic PubMed journals economic medical journals economic free journals economic best journals economic top journals economic free medical journals economic famous journals economic Google Scholar indexed journals cytometry articles cytometry Research articles cytometry review articles cytometry PubMed articles cytometry PubMed Central articles cytometry 2023 articles cytometry 2024 articles cytometry Scopus articles cytometry impact factor journals cytometry Scopus journals cytometry PubMed journals cytometry medical journals cytometry free journals cytometry best journals cytometry top journals cytometry free medical journals cytometry famous journals cytometry Google Scholar indexed journals socioeconomic articles socioeconomic Research articles socioeconomic review articles socioeconomic PubMed articles socioeconomic PubMed Central articles socioeconomic 2023 articles socioeconomic 2024 articles socioeconomic Scopus articles socioeconomic impact factor journals socioeconomic Scopus journals socioeconomic PubMed journals socioeconomic medical journals socioeconomic free journals socioeconomic best journals socioeconomic top journals socioeconomic free medical journals socioeconomic famous journals socioeconomic Google Scholar indexed journals premenopausal articles premenopausal Research articles premenopausal review articles premenopausal PubMed articles premenopausal PubMed Central articles premenopausal 2023 articles premenopausal 2024 articles premenopausal Scopus articles premenopausal impact factor journals premenopausal Scopus journals premenopausal PubMed journals premenopausal medical journals premenopausal free journals premenopausal best journals premenopausal top journals premenopausal free medical journals premenopausal famous journals premenopausal Google Scholar indexed journals
Article Details
1. Introduction
Endometriosis is a proven chronic benign disease, with occasional malignant transformation affecting close to 2–17% of women in their reproductive years [1-4]. The pelvic organs are most frequently affected, although the literature has disclosed distant extra pelvic organ involvement, such as the lungs, skin, intestinal structures etc., except the spleen [5]. However, this assertion is contested by an animal model study conducted by Elham et al. in 2019, where using flow cytometry and immunofluorescence analysis demonstrated the presence of endometriosis-derived cells in multiple organs (including the lungs, spleen, liver and brain) in the murine model with endometriosis [6]. Endometriosis is characterized by pain-related symptoms (i.e., dysmenorrhea, dysuria, dyspareunia and dyschezia), with the capacity to threaten physical, psychological and socioeconomic wellbeing [7]. It is also presumed to be strongly associated with infertility by many pieces of literature [8]. Based on these facts, it is assumed to have a significantly adverse impact on the woman, the health care system and the respectful immediate environment. However, the management, diagnosis and aetiology are still uncertain and contested, causing a big challenge to the gynaecologist [9]. The economic burden is increasing as new cases of the disease are recorded daily, coupled with an increased cost in health care provisions [10-12]. In a study conducted by Winkel et al. [13] in the United States of America, they estimated $5805 for surgical cost and $2418 for medical cost.
This study excluded indirect costs as a result of reduced productivity while at work due to fatigue, chronic pain, and also time lost from complete absenteeism. Productivity lost could greatly influence the financial status of the family and will eventually affect the gross domestic product (GDP) of countries adversely, since a substantial number of women in their early carrier ages are the most affected [12, 14]. Regardless of the socioeconomic implications involved or the complexity of the disease symptomatically, a diagnosis is always delayed, resulting in a long period of suffering of those individuals [7, 9, 12]. Most times the disease is uncovered during a workup investigating infertility, since an accurate diagnosis is often achieved during laparoscopy or laparotomy interventions [1, 12, 15]. Although the socioeconomic and physical burden of endometriosis is very high, the psychological-emotional components attached cannot be ignored. These emotional stresses are associated with dyspareunia, infertility (which reduces the self-esteem of women) and disrespect by peers and family members and often cause broken homes, which could eventually lead to severe depression. A study conducted by Berek et al. [16] reported that endometriosis was associated with chronic lower abdominal pain in 20–90% of women presenting with chronic lower abdominal pain, while more than 30–50% of women with unexplained infertility exhibited involvement of the disease at various stages. A study conducted by Fadhlaoui reported that the prevalence of endometriosis rose to 50% in women with infertility [17, 18].
2. Material and Methods
2.1 Study design
This is a cross-sectional prospective study.
2.2 Place and duration of the study
The study was performed from January 2016 to December 2018 at the Department of Gynaecology and Obstetrics at Robert Károly Private Hospital.
2.3 Recruitment and study population
A total of 87 consecutive premenopausal women aged 18–45 years attending the Ob/Gyn clinics with symptoms and complaints related to endometriosis, such as endometriosis-associated chronic pelvic pain (EACPP), dysmenorrhea, dyspareunia, and or subfertility who were scheduled for laparoscopic surgery were recruited prospectively to participate in the study. The patients were asked to fulfil the 116-item questionnaire in their language with the assistance of a trained medical supervisor. Women were also contacted later to complete a follow-up 10-item questionnaire strictly about their post-surgical emotional perception. Women also made their contacts available, which included email addresses and telephone numbers.
2.4 Exclusion criteria
- Women with a previous surgical diagnosis of endometriosis
- Patients beyond the age limits
- Patients suffering from any form of chronic illness
- Patients with a psychological disorder
- Patients who decline to participate in the study
- Patient with polycystic ovarium disease (PCOD), pelvic inflammatory disease (PID); major medical conditions; neurological and psychiatric disorders; history of gastrointestinal, urological, or orthopaedic diseases; and current use of drugs affecting cognition and mood.
2.5 Questionnaires
The administered questionnaires were multifocal, with components such as the Endometriosis Health Profile-36 (EHP-36), visual analogue scale (VAS), Numeric Rating Scale (NRS-11), general characteristics, and other information (i.e., lifestyle, nutrition and genetic exposure) incorporated in the questionnaires. The EHP-36) questionnaire is used to measure demographics, physical and mental health, emotional problems, and general perception of health and quality of life (QoL). The VAS and NRS-11 were employed to measure painful distress associated with the endometriosis. Other complementary information was included, which was used to test for a possible association of lifestyle, nutrition, and genetic exposure. The questionnaire was pretested using some voluntary hospital staff nurses to complete it, and the average time was noted.
2.6 Methods
A total of 87 women agreed to enter the study. They were recruited after signing written informed consent for the surgery and completing the questionnaire. Women were asked to make their contacts available, which included email address and telephone numbers, which they willingly provided. Further investigations including gynaecological examination; pelvic transvaginal ultrasonography; MRI, CT, cystoscopy etc., when indicated; and critical medical patient history were prepared for diagnostic and operative laparoscopies [19]. The study period lasted from January 2017 through December 2018, when the surgeries and questionnaires were completed. Validated instruments were used to assess the QoL, including the EHP-36 (a questionnaire used to measure demographics and physical, mental and socioeconomic wellbeing). The VAS and NRS-11 were employed to measure painful distress. Additional information also included investigating any association with lifestyle, nutrition and genetic exposure with the endometriosis in the questionnaires, which was completed preoperatively. The VAS is a 10-point scale, while the NRS-11 is an 11-point scale for patient self-reporting of pain for endometriosis-related painful symptoms (i.e., dyspareunia, dysChezia, non-menstrual pelvic pain, and dysmenorrhea). We commenced with 0 representing no pain and 10 representing the most miserable painful stress. None of the patients received preoperative adjuvant therapy, such as hormonal treatment. All the patients underwent radical laparoscopic surgery, depending on the degree of damage, stages, and desire. Those with infertility or subfertility issues had a combined hysterolaparoscopic procedure, with a dye test.
The stage of endometriosis was determined intraoperatively, and the disease severity was staged using the revised American Fertility Society (rAFS) classification: I (minimal), II (mild), III (moderate), or IV (severe) [20]. Postoperative follow-up was performed at 6 months, 12 months and 24 months later by postal questionnaire using the electronic platform (email) and by direct telephone conversation. The post-surgical questionnaire was dispatched on different occasions depending on the date of surgery, and each patient was followed-up for a maximum of 24 months. Further checks were also introduced by revisiting patient medical records in the hospital database on control to confirm information retrieved directly from the completed questionnaires. The essence of control at a different period is with the hope to demonstrate any positive impact on the wellbeing of women after radical laparoscopy surgery for endometriosis. During the follow-up period, we evaluated their symptoms and complaints, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, dysChezia and infertility, as well as their general wellbeing.
2.7 Consent
The purpose of the study was explained to all participants, and written and oral informed consent was obtained.
2.8 Ethical approval
The study protocol was approved by the Ethical Committee of the Robert Károly Private Hospital, Budapest, Hungary.
2.9 Data management
We used chi-square analyses and Fisher exact tests to study categoric variables in the Stata program (v.11). We investigated continuous variables using independent-samplet-testor non-parametric Mann-WhitneyUtest as appropriate. Multiple logistic and linear regression analyses were used to study associations between variables and outcomes, adjusting for potential confounders independently associated with exposure and outcome of interest in univariate analysis.A p-value < 0.05 was considered nominally significant.
3. Result
>
A total of 87 patients was enrolled in this study. They completed the modified EHP-36 questionnaire and underwent laparoscopic surgical procedures, with a follow-up of at least 24 months. The epidemiological characteristics of the patients studied were as follows: mean age at diagnosis 34.2 ± 5.97 years (with a minimum age of 22 and a maximum age of 48), duration of infertility 3.8 ± 2.1 years and average duration between symptoms to diagnosis 9.7 ± 0.35 years. All Caucasians, a minimum of completing a higher level of education, a higher income category and nulliparous women accounted for 81.6% of patients. The most prevalent complaints/symptoms reported included infertility issues (70.1%), dysmenorrhea (82.8%), dyspareunia (60.9%), abdominal bloating (93.1%) and urinary disorders (49.4%).
Table 1 illustrates general information on the patients in the study. The left ovary was the most affected single organ (42.5%). Additionally, there was involvement of the rectovaginal septum (55.2%), including infiltrating endometriosis, and superficial peritoneal implants (66.7%). The third stage of endometriosis was the most frequent finding (48.3%). Surgical interventions included adhesiolysis (70.1%) and bladder resection (9.2%). Post-surgical evaluations revealed spontaneous pregnancy achieved in 37.7% of patients and IVF-ET in 14.1% of patients with a live birth rate of 75.0%. The mean pain score using the NRS-11 preoperatively revealed 94.8% of patients had moderate to severe pain. Post-surgical pain perception improved to 81.6%, as patients reported none or insignificant periodic discomfort. The VAS before surgery revealed 94.3% of patients had moderate to severe pain. In the postoperative VASs during follow-up, pain declined tremendously, with 93.1% of patients reporting minimal to no pain at all. The completion rate by the participants was 100%, except the three cases where the monitoring of their pregnancy was discontinued in the middle of the pregnancy due to relocation.
Table 2 and Figure 1 illustrates the possible psychoemotional impact on women, during the presurgical and postsurgical periods calculated in a numerical form (scores from 1–10), with 1 representing less of an emotional effect and 10 representing a severe emotional effect on an individual. In the postsurgical analysis, all the patients reported significant changes and improvements in their lives (all the MANOVA tests revealed a significant decrease in all the disturbing negative feelings and symptoms associated with endometriosis (p = 0.001)). Figure 2 demonstrates the pain rating scores using the NRS-11 and VAS. As the Mauchly variance homogeneity test proved heteroscedasticity (chi-squared (5) = 113.835, p < 0.001)), we used the MANOVA for testing the differences among the changes in pain rating scores over time, which prove significant decreases in all forms of pain after the surgery.
Figure 3 demonstrates fertility performance after the surgical procedures, which shows significant improvement throughout the follow-up period. The ratio of spontaneous pregnancy increased from 6 months to 12 months of follow-up (chi-squared = 15.94, p = 0.001). This increase also continued from 12 months to 24 months of follow-up (chi-squared = 9.07, p = 0.028). Generally, there was a consistent increase in the ratio of spontaneous pregnancy from 6 months to 24 months of follow-up (chi-squared = 41.34, p < 0.001). Table 3 demonstrates the different types of pain-associated distress encountered by women with endometriosis. The most frequent was pricking pain/discomfort, while the least frequent was rectal bleeding (p = 0.001). Figure 4 is an illustration of women’s assessments of their lives before and after the surgery. Table 4 and Figure 4 shows a tremendous improvement in all previous negative indices of their lives (p < 0.001), while Table 4 shows the outcome of women’s QoL as the follow-up period progresses. As the Mauchly variance homogeneity test proved heteroscedasticity (chi-squared (5) = 103.08, p < 0.001), we used the MANOVA for testing the differences among the QoL changes over time. The MANOVA tests showed significant increases in QoL after the surgery.
|
General characteristics of women with endometriosis in this study (n=87) |
|||
|
Mean age at menarche (years) |
13.2 ± 1.293 years (9–17) |
||
|
Mean age at diagnosis of endometriosis |
34.2 ± 5.97 years (20–48) |
||
|
Mean age at the onset of symptoms relating to endometriosis |
24.5 ± 5.710 years (15–37) |
||
|
Duration of infertility |
3.8 ± 2.1 years |
||
|
Duration of symptoms before diagnosis |
9.7 ± 0.35 years |
||
|
Characteristics |
Type |
Number (n) |
Percentage (%) |
|
Localization of endometriosis |
Superficial/deep left ovary involvement |
37 |
42.6% |
|
Deep right ovary involvement |
14 |
16.2% |
|
|
Both right and left ovary involvement |
27 |
31.0% |
|
|
Superficial (RVS)/deep rectovaginal septum involvement |
62 |
71.3% |
|
|
Superficial bladder involvement |
48 |
55.2% |
|
|
Deep bladder involvement |
10 |
11.5% |
|
|
Intestinal involvement |
13 |
14.9% |
|
|
Superficial peritoneal involvement |
58 |
66.7% |
|
|
Adenomyosis |
10 |
11.5% |
|
|
Other surgical procedures |
Adhesiolysis |
61 |
70.1% |
|
Bladder resection |
8 |
9.2% |
|
|
Dixon operation |
2 |
2.3% |
|
|
Relapse of endometriosis |
5 |
5.7% |
|
|
Stage of endometriosis |
Stage 1 |
3 |
4.9% |
|
Stage 2 |
12 |
19.7% |
|
|
Stage 3 |
29 |
47.5% |
|
|
Stage 4 |
17 |
27.9% |
|
|
Other complication |
Endometroid carcinoma |
1 |
1.6% |
|
Fertility |
Infertility issue preoperational |
61 |
70.1% |
|
Mode of pregnancy |
Spontaneous pregnancy |
23 |
37.7% |
|
IVF-ET |
9 |
14.1% |
|
|
Outcome of pregnancy |
Spontaneous delivery |
17 |
53.1% |
|
Caesarean section |
7 |
21.9% |
|
|
Missed abortion |
4 |
12.5% |
|
|
Lost to follow-up |
3 |
9.4% |
|
|
Preoperative pain score (NRS-11) |
Moderate to severe pain |
85 |
94.8% |
|
Postoperative pain score (NRS-11) |
Mild to zero pain |
71 |
81.6% |
|
Preoperative VAS score |
Moderate to severe pain |
82 |
94.3% |
|
Postoperative VAS score |
Minimal to zero pain |
81 |
93.1% |
|
Additional factors |
Family history of endometriosis |
** |
15.0% |
|
High red meat/fish |
** |
*** |
|
|
Cigar rate (≥ 5 sticks/day) |
17 |
19.5% |
|
|
Alcohol consumption (beer/wine regularly) |
8 |
9.2% |
|
|
Alcohol consumption (gin/whiskey regularly) |
14 |
16.1% |
|
|
Coffee consumption > 1 cup/daily |
29 |
33.5% |
|
|
Menstruation history |
Bleeding disorder (metrorrhagia) |
57 |
66.0% |
|
Cycles dysfunction (spotting bleeding) |
43 |
49% |
|
|
Miscellaneous issues |
Use of sanitary napkins (solely to more regularly) |
63 |
72% |
Table 1: General characteristics of women before and after surgery follow-up (6, 12 and 24 months) (n=87).
|
Emotion |
Test |
Value |
F |
Hypothesis df |
Error df |
Sig. |
|
|
Exhausting emotionally |
Pillai's Trace |
0.871 |
189.285 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.129 |
189.285 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
6.760 |
189.285 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
6.760 |
189.285 |
3 |
84 |
<0.001 |
||
|
Sickening emotionally |
Pillai's Trace |
0.725 |
73.854 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.275 |
73.854 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
2.638 |
73.854 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
2.638 |
73.854 |
3 |
84 |
<0.001 |
||
|
Unbearable |
emotionally |
Pillai's Trace |
0.883 |
211.495 |
3 |
84 |
<0.001 |
|
Wilks' Lambda |
0.117 |
211.495 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
7.553 |
211.495 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
7.553 |
211.495 |
3 |
84 |
<0.001 |
||
|
Miserable emotionally |
Pillai's Trace |
0.864 |
176.230 |
3 |
83 |
<0.001 |
|
|
Wilks' Lambda |
0.136 |
176.230 |
3 |
83 |
<0.001 |
||
|
Hotelling's Trace |
6.370 |
176.230 |
3 |
83 |
<0.001 |
||
|
Roy's Largest Root |
6.370 |
176.230 |
3 |
83 |
<0.001 |
||
|
Torturing emotionally |
Pillai's Trace |
0.885 |
215.733 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.115 |
215.733 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
7.705 |
215.733 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
7.705 |
215.733 |
3 |
84 |
<0.001 |
||
|
Depressing emotionally |
Pillai's Trace |
0.877 |
198.814 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.123 |
198.814 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
7.101 |
198.814 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
7.101 |
198.814 |
3 |
84 |
<0.001 |
||
|
Affect your work negatively |
Pillai's Trace |
0.835 |
141.547 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.165 |
141.547 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
5.055 |
141.547 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
5.055 |
141.547 |
3 |
84 |
<0.001 |
||
|
Affect your learning negatively |
Pillai's Trace |
0.812 |
121.096 |
3 |
84 |
<0.001 |
|
|
Wilks' Lambda |
0.188 |
121.096 |
3 |
84 |
<0.001 |
||
|
Hotelling's Trace |
4.325 |
121.096 |
3 |
84 |
<0.001 |
||
|
Roy's Largest Root |
4.325 |
121.096 |
3 |
84 |
<0.001 |
||
As all the Mauchly variance homogeneity test proved heteroscedasticity, we have used MANOVA for testing the differences among the changes in emotions over time. All tests had significant decreases of all depressing problems and emotions after the surgery.
Table 2: Comparison of emotional assessment of individuals before and after surgery according to timing of the follow-up (6, 12 and 24 months).
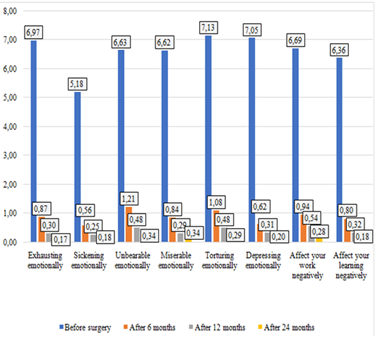
Figure 1: Comparison of emotional impact assessment of individuals before and after surgery according to timing of the follow-up (6, 12 and 24 months).
As the nauchly variance homogeneity test proved heteroscedasticity (chi-squared (5)=113.835, p0.001), we also used MANOVA for testing the differences among the changes in the pain rating scores over time. The MANOVA tests showed the significant decrease of all pain after the surgery.
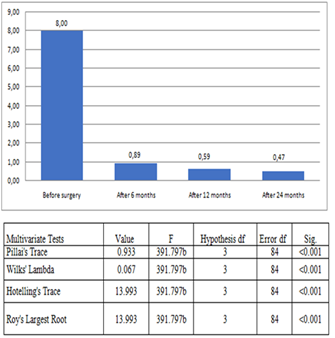
Figure 2: Comparison of NRS-11 and VAS scores before and after sugery according to timing of the follow-up (6, 12 and 24 months).
The ratio of spontaneous pregnancy increased from the 6-month to the 12-month follow-up after surgery (chi- squared 15.94, p<0.001) and from the 12-month to 24-month follow-up after surgery (chi-square 9.07, p
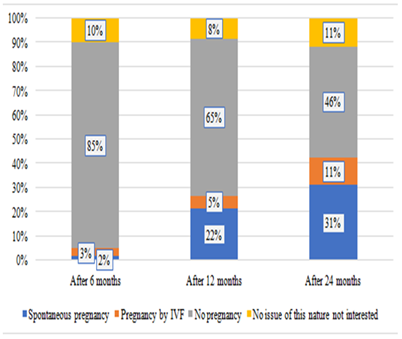
Figure 3: Comparison of EHP-36 scores before and after surgery according to timing of the follow-up (6, 12 and 24 months).
|
Symptoms |
Frequency |
Percentage |
Frequency |
Percentage |
Total |
|
Yes |
No |
Total |
|||
|
Rectal bleeding |
18 |
21% |
69 |
79% |
100% |
|
Painful defecation |
25 |
29% |
62 |
71% |
100% |
|
Urinary problems |
43 |
49% |
44 |
51% |
100% |
|
Pressing pain or discomfort |
50 |
57% |
37 |
43% |
100% |
|
Stabbing pain or discomfort |
57 |
66% |
30 |
34% |
100% |
|
Tender pain or discomfort |
59 |
68% |
28 |
32% |
100% |
|
Crushing pain or discomfort |
66 |
76% |
21 |
24% |
100% |
|
Gastrointestinal discomfort |
70 |
80% |
17 |
20% |
100% |
|
Pricking pain or discomfort |
72 |
83% |
15 |
17% |
100% |
The incidences of problems/pains significantly differ from each other. The most frequent is pricking pain or discomfort, while the least frequent is rectal bleeding.
Table 3: Frequently experienced preoperative pain and other symptoms associated with endometriosis in this study (n=87).
As the mauchly variance homogeneity test proves heteroscedasticity (chi-squared (5)=128.943, p<0.001). MANOVA for testing the differences among the QoL change during time, prove significant increase in QoL after the surgery. This improvement was experienced mostly after 12 months postsurgery.
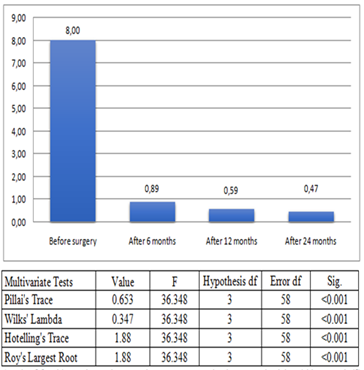
Figure 4: Comparison of EHP-36 scores before and after surgery according to timing of the follow-up (6-12-24 months).
Table 4: Improvement in quality of life and general wellbeing before and after surgery in women with endometriosis (n=87).
4. Discussion
The good physical and mental states of the populace is a necessity for a healthy state. Women occupy a special role in the nation and the building of families and societies. Therefore, what affects them exhibits a significant influence on the system (society). In this study, we hoped to established the psychoemotional, physical and economic trauma inflicted by endometriosis on women and the possible benefit of endoscopic surgery. This study demonstrates some of the usefulness of the EHP-36, VAS, and another questionnaire in evaluating the QoL and wellbeing in patients with endometriosis after radical laparoscopic surgery.
Many studies have shown that endometriosis-related symptoms and complaints are associated with numerous
handicaps on women in terms of learning abilities, infertility, reduced QoL, and loss of work productivity [21, 22]. Comparable to our study, other studies also reported the serious negative effects of endometriosis on the learning abilities of individuals [23, 24].
Likewise, just like many other previous related studies, mainly in the Western and the developed world, we encountered some challenges. This series of limitations were also confronted in those studies due to sample size, difficulty in choosing a control group (as the diagnosis is mainly surgical), delay in diagnosis, multiplicity of symptoms etc. [25, 26]. Other factors affecting the quantification of the impact of endometriosis on women and society are lack of geographical spread, educational standards within a given society, and ethnocultural differences across different countries [12, 25]. The average age of first symptoms in this study was 24.5 ± 5.710 years (15–37), which is similar to other studies reported, with an average age of first symptoms between 20 and 29 years [26-27]. In our study, the average age of diagnosis is 34.2 ± 5.97 years (20-48). In our study, we observed an average diagnostic delay of 9.7 ± 0.35 years, which is inconsistent with earlier reports from the UK and US. [28, 29]. The reasons for a delay may be numerous, including sociocultural behaviour, lack of personnel, health care cost, others strongly associated with care-seeking experiences in primary care, discrediting nature of menstruation, and risk of stigmatization [30-31]. In our study, the unbearable chronic pain, frequency of pain, fatigue and psychological symptoms (such as self-reported depression and anxiety) were significantly high, which we were able to analyse using the modified EHP-36 to compare the postsurgical state of the patient. The overall post-surgical follow-up outcome showed significant improvements in all areas of the contest, as illustrated in Tables 2, 3, 4 and in Figures 1, 2 and 3 (all p < 0.001).
The effect of endometriosis on physical wellbeing, excluding the mental distress of women, also significantly improved after surgery, using the VAS and the NRS-11 pain scores (QoL), which gradually decreased from 8.0 ± 2.11 points before surgery to 0.47 ± 1.25 points after surgery). This was an improvement over the study conducted by Alborzi et al. in 2017, where the outcome was 8.23 ± 2.03 points, which decreased to 4.46 ± 2.47 points in 93.0% of patients [25]. Using the modified EHP-36, the effect on socioemotional wellbeing was also substantively significant (p < 0.001), as illustrated in Table 2 and Figure1, which was relatively similar to some other earlier studies [32-34]. These derogatory and agonizing states around these women, due to the physical, emotional, and socioeconomic effects of endometriosis, were significantly reduced or completely eradicated with the effect of radical surgery, as close to 93.1% of patients reported substantial to complete improvement in their QoL, while 94.2% of patients reported significant to complete improvement in their general wellbeing 24 months after surgery in Table 4. Other studies also recorded some level of postsurgical success; however, their outcomes were not superior [25, 35]. Pain-related symptoms of endometriosis were attributed to be the major factors of learning dysfunction and work productivity loss in endometriosis, as in other studies conducted by Nnoaham et al. [12] and Bahrami et al. [36].
However, less emphasis was made in assessing reduced effectiveness at work rather than work absence, unfortunately, which accounts for close to 60% of total work productivity loss. The total indirect costs of productivity loss per patient per year were estimated at $9910.57, while the surgery cost per patient per year was about $1415.08 [12, 37]. The annual estimated financial burden to individuals and society varied from US $1.6 billion in Hungary, US $9.9 billion in the UK, US $12.5 billion in Germany to the US $49.6 billion in the US, as reported by Simoens et al. in 2012 [37-38]. Another study conducted by Armours et al. [11], reported an estimated cost of about US $6.50 billion, of which the majority of costs (75–84%) were due to productivity loss. Unfortunately, in this study, emphasis was not made on general productivity loss or other expenses incurred by patients, as the aim of the study was mainly on the effectiveness of laparoscopy in the management of endometriosis and QoL. In 2013, Prast et al. also conducted a retrospective study about the economic burden of endometriosis, with a total direct cost per patient per year (public insurance and out-of-pocket) of $8819.64 and a total indirect cost per patient per year (sick leave and unemployment due to endometriosis) of $3314.39 [10].
Despite, the role of painful symptoms of endometriosis affecting work productivity loss, loss of valuable time in learning, and cost involved, as shown in this study and other earlier relevant studies [21-22, 37]. Other severe derogatory implications of endometriosis are also very frequent, such as is its impact on fertility [7, 12, 39]. In accordance to this study, many studies have also reported a negative impact on fertility and as a result the medical, health, and economic downturn/cost/due to subfertility/infertility associated with the disease [21, 40]. In this present study, subfertility/infertility affected about 61% of the women, seemingly in agreement with other previous studies [25, 41]. Interestingly, the post-surgical fertility outcome was encouraging, even though the follow-up period of 24 months was short.
Pregnancy was recorded in 52.5% (32/61) of women, with a live birth rate of 78.1% (25/32) and missed abortion/incomplete abortion rate of 12.5% (4/32); 9.4% (3/32) of patients were lost to follow-up during pregnancy (p < 0.001). We obtained a better outcome than other similar studies, such as that conducted by Soriano et al. in 2016, where they reported successful deliveries in 33 women (42.3%). Three women (9%) conceived spontaneously, and all the other women conceived after IVF treatment. Women who delivered were younger (32.5 ± 4.1 years vs. 35.5 ±3.8 years), while in 2018, Roman et al. conducted a study with the following outcomes at the end of a follow-up period of 79 months: 29 patients achieved pregnancy (81%), with natural conception being recorded in 17 of them (59% of conceptions and 29 deliveries (78%)) [42-44].
Both general patient wellbeing and QoL improved significantly, with patient’s preoperative perceptions of QoL and GWB being rated from bad to very bad 89.6% and 93.1%, respectively, while patient’s postoperative perceptions significantly improved by 93.1% and 94.2%, respectively (p < 0.001). The improvement observed was mainly the result of experiencing disease-free states and the return of fertility in most cases. This outcome was in line with studies conducted by Alborzi et al. [25], Nnoaham et al. [12] and Marjaleena et al. [34]. A slight correlation was observed in the family linkage (genetics) of about 15% [46] of patients. Endometrioid carcinoma was recorded in a 45-year-old patient (1/87; 1.6%), which was similar to other studies [47]. In this study, we did not find any significant association between cigarette smoking, alcohol consumption and endometriosis, which was similar to a study conducted by Bravi et al. [48] and Thylan [49], respectively. Similarly, an association between eating habits, types of food and endometriosis was not ascertained. However, there was a tendency shift in prevalence in those who consumed more pure alcohols and cigarettes, which may be the result of the negative impact of endometriosis, triggering a soul comforting lifestyle [48]. There was no direct influence of other medical conditions, although a higher occurrence was observed in those with thyroid diseases and previous use or no use of contraceptive, antihypertensive, and antidiabetic drugs.
Additional surgical procedures were warranted due to the spread of the disease, such as the Dixon operation (2/87; 2.3%) due to intestinal involvement. Bladder resection was done in 9.2% (8/87) of patients, and adhesiolysis was performed in 70.1% (61/87) of patients, as adhesions are one of the major direct complications of endometriosis and the most frequently affected organ was the left ovary (37/87; 42%), which was similar to other studies [13, 18, 25]. A study conducted byKamalifard et al. reported that women who used cloth menstrual pads had a higher incidence of endometriosis; this outcome is similar to the unexpected outcome of our studies where more women reported the regular use of sanitary napkins (pads) (63/87; 72%) [50]. The possible mechanism of action may be slowing down the menstrual flow, thereby possibly aiding retrograde menstruation.
However, some of this result could be presumed, as there are not enough adequate scientific proofs, and therefore may warrant broader and more thorough investigations. Also, the incorporation of the additional modifications into the EHP-36 questionnaire adopted in this study also highlighted some issues to focus on when attending to patients in the outpatient units, indicating the possible presence of endometriosis. Such issues include heavy bleeding in 66% (57/87) of patients, irregular bleeding (including mid-cycle spotting) in 49% (43/87) of patients, lower abdominal pain not associated with current infectious disease relieved only by NSAIDs in 73.6% (64/87) of patients and difficulty to conceive in 66.6% (58/87) of patients in this study, which is similar to other studies [12, 13, 25, 40].
5. Conclusions
Women with endometriosis are under a severe agonizing state of mind, and their general wellbeing and QoL are significantly impaired. Individualized radical laparoscopic surgery, with an occasional combination of hysteroscopic manoeuvres, significantly improves wellbeing, QoL, sexual function, and return of fertility, regardless of stage and age of the patient, and this can be quantified and qualified. The incorporation of the EHP-36 questionnaire improves service by providers and leads to a wider scope of accessing gynaecologic patients in outpatient clinics, with an early suspicion of endometriosis as the background disease behind the patient’s symptoms.
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, A.A.E. and M.K.; methodology, IF., A.A.E.; software, A.A.E.; validation, A.A.E., M. K. and I.F.; formal analysis, A.A.E.; investigation, A.A.E; resources, Á.R.; data curation, P.S.; writing—original draft preparation, Á.K.; writing—review and editing, A.A.E.; visualization, M.K.; supervision, M.K., P.S.; project administration, Á.K.; funding acquisition, A.A.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We acknowledge the administrative staffs and the hospital technical, statistical group, and the general staff of the endoscopic unit, and the IVF unit of the hospital for their enormous support in making this article possible.
Conflicts of Interest
The authors declare no conflict of interest
References
- Lemaire G S. More than just menstrual cramps: Symptoms and uncertainty among women with endometriosis. Journal of Obstetrics and Gynecology Neonatal Nursing 33 (2004): 71-79.
- Eskenazi B, Warner M L. Epidemiology of endometriosis. Obstetrics and Gynecology Clinics of North America 24 (1997): 235-258.
- Vercellini P, Eskenazi B, Consonni D, Somigliana E, Parazzini F, Abbiati A, et al. Oral contraceptives and risk of endometriosis: A systematic review and meta-analysis. Human Reproduction Update 17 (2011): 159-170.
- Facchin F, Barbara G, Saita E, Mosconi P, Roberto A, Fedele L, et al. Impact of endometriosis on quality of life and mental health: Pelvic pain makes the difference. Journal of Psychosomatic Obstetrics & Gynecology 36 (2015): 135-141.
- Radivojevic R M, Lazic L. [Endometriosis with a rare localization]. Srpski Arhiv za Celokupno Lekarstvo 90 (1962): 871-873.
- Samani E N, Mamillapalli R, Li F, Mutlu L, Hufnagel D, Krikun G, et al. Micrometastasis of endometriosis to distant organs in a murine model. Oncotarget 10 (2017): 2282-2291.
- Chaman-Ara K, Bahrami M A, Bahrami E. Endometriosis psychological aspects: A literature review. Journal of Endometriosis and Pelvic Pain Disorders, 9 (2017): 105-111.
- Dancet E A, Apers S, Kluivers K B, Kremer J A, Sermeus W, Devriendt C, et al. The ENDOCARE questionnaire guides European endometriosis clinics to improve the patient-centeredness of their care. Human Reproduction 27 (2012): 3168-3178.
- Damewood M, Kresch A J, Metzger D, Begany T. Current approaches to endometriosis. Patient Care 31 (1997).
- Prast J, Oppelt P, Shamiyeh A, Shebl O, Brandes I, Haas D. Costs of endometriosis in Austria: A survey of direct and indirect costs. Archives of Gynecology and Obstetrics 288 (2013): 569-576.
- Armour M, Lawson K, Wood A, Smith C A, Abbott J. The cost of illness and economic burden of endometriosis and chronic pelvic pain in Australia: A national online survey. PLoS One 14 (2019): e0223316.
- Nnoaham K E, Hummelshoj L, Webster P, d’Hooghe T, de Cicco Nardone F, de Cicco Nardone C, et al. Impact of endometriosis on quality of life and work productivity: A multicenter study across ten countries. Fertility and Sterility 96 (2011): e8-373.e8.
- Winkel C A. Combined medical and surgical treatment of women with endometriosis. Clinical Obstetrics and Gynecology 42 (1999): 645-663.
- Fourquet J, Báez L, Figueroa M, Iriarte R I, Flores I. Quantification of the impact of endometriosis symptoms on health-related quality of life and work productivity. Fertility and Sterility 96 (2011) 107-112.
- Buck Louis G M, Hediger M L, Peterson C M, Croughan M, Sundaram R, Stanford J, et al. Incidence of endometriosis by study population and diagnostic method: The ENDO study. Fertility and Sterility 96 (2011): 360-365.
- Berek J S, Longacre T A, Friedlander M. Ovarian, fallopian tube and peritoneal cancer. In J. S. Berek (Ed.), Berek and Novak's gynecology, 15th ed. Philadelphia: Lippincott, Williams and Wilkins (2012): 1350-1427.
- Hart R. Unexplained infertility, endometriosis, and fibroids. BMJ 327 (2003): 721-724.
- Fadhlaoui A, Bouquet de la Jolinière J, Feki A. Endometriosis and infertility: How and when to treat?. Frontiers in Surgery 1 (2014): 24.
- Parasar P, Ozcan P, Terry KL. Endometriosis: Epidemiology, diagnosis and clinical management. Current Obstetrics and Gynecology Reports 6 (2017): 34-41.
- Alimi Y, Iwanaga J, Loukas M, Tubbs R S. The clinical anatomy of endometriosis: A review. Cureus 10 (2018): e3361.
- Jones G, Jenkinson C, Kennedy S. Evaluating the responsiveness of the endometriosis health profile questionnaire: The EHP-30. Quality of Life Research 13 (2004): 705-713.
- Florentino AVA, Pereira A M G, Martins J A, Lopes R G C, Arruda R M. Quality of life assessment by the Endometriosis Health Profile (EHP-30) questionnaire prior to treatment for ovarian endometriosis in Brazilian women. Revista Brasileira de Ginecologia e Obstetrícia 41 (2019):548-554.
- Moradi M, Parker M, Sneddon A, Lopez V, Ellwood D. Impact of endometriosis on women's lives: A qualitative study. BMC Women’s Health 14 (2014): 123.
- Sepulcri RD, do Amaral VF. Depressive symptoms, anxiety, and quality of life in women with pelvic endometriosis. European Journal of Obstetrics & Gynecology and Reproductive Biology 142 (2009): 53-56.
- Alborzi S, Hosseini-Nohadani A, Poordast T, Shomali Z. Surgical outcomes of laparoscopic endometriosis surgery: A 6-year experience. Current Medical Research Opinion 33 (2017): 2229-2234.
- Berkley K J, Rapkin A J, Papka R E. The pains of endometriosis. Science 308 (2005): 1587-1589.
- Ferrie J E, Kivimäki M, Head J, Shipley M J, Vahtera J, Marmot M G. A comparison of self-reported sickness absence with absences recorded in employers’ registers: Evidence from the Whitehall II study. Occupational & Environmental Medicine 62 (2005): 74-79.
- Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertility and Sterility 86 (2006): 1296-1301.
- Hadfield R, Mardon H, Barlow D, Kennedy S. Delay in the diagnosis of endometriosis: A survey of women from the USA and the UK. Human Reproduction 11 (1996): 878-880.
- Gilmour J A, Huntington A, Wilson H. The impact of endometriosis on work and social participation. International Journal of Nursing Practice 14 (2009): 443-448.
- Facchin F, Barbara G, Dridi D, Alberico D, Buggio L, Somigliana E, et al. Mental health in women with endometriosis: Searching for predictors of psychological distress. Human Reproduction 32 (2017): 1855-
- De Graaff A A, D'Hooghe T M, Dunselman G A, Dirksen C D, Hummelshoj L, Simoens S, et al. The significant effect of endometriosis on physical, mental and social wellbeing: Results from an international cross-sectional survey. Human Reproduction 28 (2013): 2677-2685.
- Ferreira A L L, Bessa M M M, Drezett J, de Abreu L C. [Quality of life of the woman carrier of endometriosis: Systematized review]. Reprodução & Climatério 31 (2013): 48-54.
- Setälä M, Härkki P, Matomäki J, Mäkinen J, Kössi J. Sexual functioning, quality of life and pelvic pain 12 months after endometriosis surgery including vaginal resection. Acta Obstetricia et Gynecologica Scandinavica 91 (2012): 692-698.
- Deguara C S, Pepas L, Davis C. Does minimally invasive surgery for endometriosis improve pelvic symptoms and quality of life?. Current Opinion in Obstetrics and Gynecology 24 (2012): 241-244.
- Bahrami M A, Chaman-Ara K, Bahrami E. Impact of endometriosis on work productivity and activity impairment: A descriptive literature review. Bali Medical Journal 6 (2017): 263-267.
- Simoens S, Dunselman G, Dirksen C, Hummelshoj L, Bokor A, Brandes I, et al. The burden of endometriosis: Costs and quality of life of women with endometriosis and treated in referral centres. Human Reproduction 27 (2012): 1292-1299.
- Bokor A. Endometriosis in Hungary (2010).
- Dancet E A, Nelen W L, Sermeus W, De Leeuw L, Kremer J A, D'Hooghe T M. The patients' perspective on fertility care: A systematic review. Human Reproduction Update 16 (2010):467-487.
- Abbott J A, Hawe J, Clayton R D, Garry R. The effects and effectiveness of laparoscopic excision of endometriosis: A prospective study with 2–5 year follow-up. Human Reproduction 18 (2003): 1922-1927.
- Minas V, Dada T. Laparoscopic treatment of endometriosis and effects on quality of life: A retrospective study using the short form EHP-5 endometriosis specific questionnaire. Journal of Obstetrics and Gynaecology 34 (2014): 336-340.
- Soriano D, Adler I, Bouaziz J, Zolti M, Eisenberg V H, Goldenberg M, et al. Fertility outcome of laparoscopic treatment in patients with severe endometriosis and repeated in vitro fertilization failures. Fertility and Sterility 106 (2016) 1264-1269.
- Roman H, Chanavaz-Lacheray I, Ballester M, Bendifallah S, Touleimat S, Tuech J J, et al. High postoperative fertility rate following surgical management of colorectal endometriosis. Human Reproduction, 33 (2018): 1669-1676.
- Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertility and Sterility 86 (2006): 1296-1301.
- Fourquet J, Gao X, Zavala D, Orengo J C, Abac S, Ruiz A, et al. Patients' report on how endometriosis affects health, work, and daily life. Fertility and Sterility 93 (2010): 2424-2428.
- Bloski T, Pierson R. Endometriosis and chronic pelvic pain: Unraveling the mystery behind this complex condition. Nursing for Women’s Health 12 (2008): 382-395.
- Mills A M, Liou S, Ford J M, Berek J S, Pai R K, Longacre T A. Lynch syndrome screening should be considered for all patients with newly diagnosed endometrial cancer. American Journal of Surgical Pathology 38 (2014): 1501-1509.
- Bravi F, Parazzini F, Cipriani S, Chiaffarino F, Ricci E, Chiantera V, et al. Tobacco smoking and risk of endometriosis: A systematic review and meta-analysis. BMJ Open 4 (2014): e006325.
- Thylan S. Endometriosis and moderate alcohol use. American Journal of Public Health 85 (1995): 1021-1022.
- Mollazadeh S, Kamalifard M, Oskouei B S, Mirghafourvand M, Aminisani N, Shobeiri M J. Association between health behaviours during menstruation and endometriosis. Journal of Clinical and Diagnostic Research 13 (2019): LC16-LC20.
