Subtotal Transepithelial Phototherapeutic Keratectomy with Mitomycin C Application for Central Corneal Opacities-Three Case Series
Article Information
Tamer Adel Refai*
Research Institute of Ophthalmology, Giza, Egypt
*Corresponding Author: Tamer Adel Refai, Research Institute of Ophthalmology, Giza, Egypt
Received: 15 September 2019; Accepted: 25 September 2019; Published: 03 October 2019
Citation: Tamer Adel Refai. Subtotal Transepithelial Phototherapeutic Keratectomy with Mitomycin C Application for Central Corneal Opacities-Three Case Series. Journal of Ophthalmology and Research 2 (2019): 050-056.
View / Download Pdf Share at FacebookAbstract
Purpose: To evaluate the beneficial effects of transepithelial subtotal phototherapeutic keratectomy (PTK) with mitomycin C application for corneal opacities on patients’ visual acuity.
Methods: Three cases with central corneal opacities were subjected to transepithelial subtotal (PTK) using Excimer laser ablation with mitomycin C (0.02%) application for 2 minutes, the first case with a central post-PRK with mitomycin corneal scar 98 µ depth, where PTK ablation depth only 70 µ (thin cornea=430 µ), the second case with a central post-traumatic corneal scar 121 µ depth, with PTK ablation depth only 70 µ (thin cornea=480 µ) and the third case with right corneal (granular) dystrophy, with opacity level was 200 µ, where PTK of only 100 µ was done (young female patient).
Results: The BCVA increased from 0.2 to 0.7 in case 1 and from 0.2 to 0.5 in case 2 and from 0.05 to 0.5 in case 3, without evidence of residual haze in case 1, and with minimal residual haze in case 2 and case 3.
Conclusion: In the presence of relatively non-superficial corneal opacities of various causes, subtotal transepithelial phototherapeutic keratectomy with mitomycin C application can result in marked improvement of visual acuity without the need for keratoplasty.
Keywords
Transepithelial subtotal (PTK), Mitomycin C, Central corneal opacities
Transepithelial subtotal (PTK) articles, Mitomycin C articles, Central corneal opacities articles
Article Details
1. Introduction
Corneal opacities can arise from various etiologies, any of which can cause marked impairment of the visual acuity. Among common causes are trauma [1], Corneal degenerations [2], corneal dystrophies [3], trachoma [4], herpetic corneal diseases [5] and a variety of otherwise corneal infections [6] and following surface ablation with excimer laser [7]. Surgical treatment for corneal opacities included corneal transplantation [8], whether penetrating [9] or lamellar [10] according to the level of the opacity, in addition to phototherapeutic keratectomy by excimer laser treatment after accurate determination of opacity level by anterior segment optical coherence tomography (AS-OCT), being a non invasive and a non contact method [11-12]. Phototherapeutic keratectomy had been used in treating superficial corneal opacities with promising results [13-15]. In this article, I presented the results of three cases, in which phototherapeutic keratectomy with mitomycin C, 0.02% application was not planned to remove the whole opacity level determined by anterior segment OCT because of insufficient corneal thickness to emphasize how this partial opacity removal can be beneficial for patients.
2. Case Presentation
2.1 Case 1
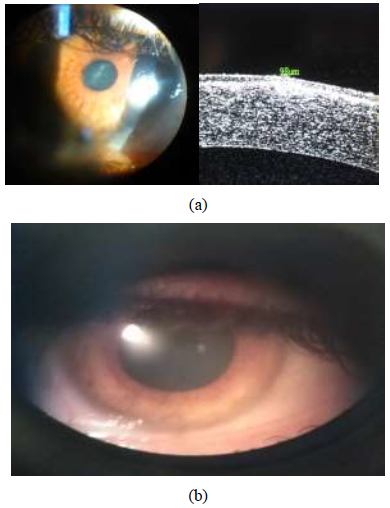
A male patient aged 34 years, he presented to refractive unit at the research institute of ophthalmology Giza-Egypt on January 2019 with bilateral myopia with high astigmatism, and owing to abnormal corneal tomography, photorefrcative keratectomy with mitomycin C application was performed in his both eyes to correct his refractive error in both eyes. He suffered from delayed epithelial healing in his left eye which ended one month after his refractive surgery with a central corneal scar which does not respond to topical steroid treatment (Figure 1a). His best corrected visual acuity in Snellen lines was reduced to 0.2 from a preoperative value of 0.7. Anterior segment OCT revealed the opacity level reaching 98 µ from the epilthelial surface, the central pachymetric reading was 430 µ, the decision was to perform transepithelial phototherapeutic keratectomy removing only 70 µ to decrease only the density of opacity without inducing a refractive error as the patient refused to wear glasses after the PTK (being a worker and he seeked refractive surgery to get rid of his glasses), the flattest Keratometric (K) reading was 37.2 Diopters (D) axis 165.8, and the steepest (K) reading was 38.2D and the average keratometric reading was 37.7D. The patient signed an informed consent. The laser ablation was performed by the Allegretto Wave Light Eye-Q 1010 (400 Hz) with active eye tracker (frequency 400 Hz) by the phototherapeutic keratectomy (PTK) programme removing only 70 µ from the corneal surface (including the epithelium) at 5.0 mm optical zone followed by mitomycin C (0.02%) application to ablated stroma for 2 minutes to avoid development of recurrent corneal haze, followed by application of a bandage contact lens. Post-operatively, the patient was given topical antibiotic and steroid drops 4 times/day each and a GABA analogue 2 tablets/day to 2 days to decrease pain sensation. The patient was examined on first, fourth post-operative day where the bandage contact lens was removed after the epithelium had healed. The patient was then instructed to increase the frequency of topical steroids to 7 times/day for further two weeks, and intraocular pressure closely monitored by applanation tonometry to guard against steroid induced glaucoma. The uncorrected visual acuity in Snellen lines was re-examined after one month which was found to be improved to 0.7 with no further improvement on trial of refraction. No trace of the opacity was noted after the PTK (Figure 1b).
Figure 1: (a) Revealing 34 male patient with left eye showing central corneal scar resulting from delayed epithelial healing after PRK with mitomycin;on the left side slit-lamp photography image and on the right side; anterior segment OCT image denoting the level of opacity; (b) Post-PTK with mitomycin C picture of same patient Lt eye in Figure 2a showing complete resolution of the central corneal scar.
2.2 Case 2
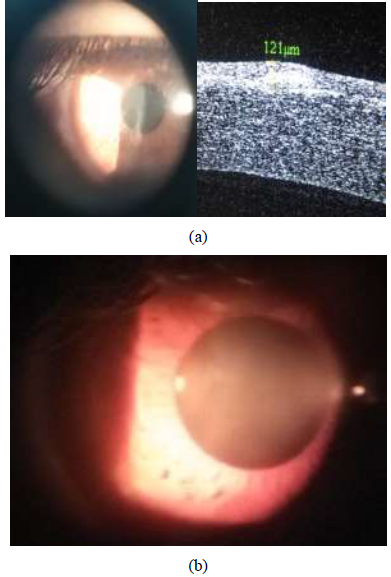
A male patient aged 33 years, he presented to refractive unit at the research institute of ophthalmology Giza-Egypt on July 2019 with right corneal opacity which was diagnosed as post-traumatic corneal scar. The patient had previously performed bilateral laser in situ keratomileusis (Lasik) several years ago. His uncorrected visual acuity in snellen lines was hardly 0.2 which did not improve on refractive correction. The anterior segment OCT revealed the opacity level reaching 121 µ from the epilthelial surface (Figure 2a).
By pentacam, the flattest keratometric readings was 40.1D axis 29.8º and the steepest keratometric readings was 42.4D, the average keratometric reading was 41.25D, the central pachymetric reading was 480 µ. Owing to the corneal thinning from previous Lasik procedure and inability to perform accurate refraction because of the corneal opacity, a decision to perform PTK with mitomycin C application removing only 70 µ to decrease the level of the opacity and provide smoothening of the corneal surface trying to improve best corrected visual acuity as much as possible, and this visual expectation was explained to the patient and he signed informed consent. The laser ablation was performed by the Allegretto Wave Light Eye-Q 1010 (400 Hz) with active eye tracker (frequency 400 Hz) by the phototherapeutic keratectomy (PTK) programme removing only 70 µ from the corneal surface (including the epithelium) at 5.0 mm optical zone followed by mitomycin C (0.02%) application to ablated stroma for 2 minutes to avoid development of recurrent corneal haze, followed by application of a bandage contact lens. Post-operatively, the patient was given topical antibiotic and steroid drops 4 times/day each and a GABA analogue 2 tablets/day to 2 days to decrease pain sensation. The patient was examined on first, fourth post-operative days where the bandage contact lens was removed after complete epithelial healing. The patient was instructed to increase the frequency of topical steroids to 10 times/day for one week, followed by tapering the frequency to 7 times/day for another week with close monitoring of intraocular pressure by applanation tonometry to guard against steroid induced glaucoma. The uncorrected visual acuity in snellen lines was re-examined after one month, which was found to be 0.2 unaided and improved to 0.5 with the addition of -1.50 sphere, there was minimal trace of the opacity post-PTK and the patient was reasonably satisfied (Figure 2b).
Figure 2: (a) Revealing 33 male patient with right eye showing central corneal scar resulting from a post-traumatic ulcer in a patient with bilateral Lasik several years age;on the left side slit-lamp photography image and on the right side; anterior segment OCT image denoting the level of opacity; (b) Post-PTK with mitomycin C picture of same patient right eye in Figure 2b: showing only minimal residual trace of the post-traumatic corneal scar.
2.3 Case 3
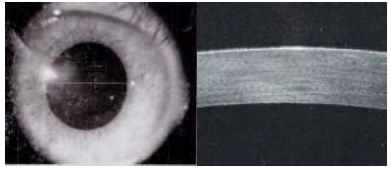
A female patient aged 18 years, she presented to cornea unit at the research institute of ophthalmology Giza-Egypt on June 2015 with bilateral corneal opacity which was diagnosed as granular dystrophy. In the right eye, the anterior segment OCT revealed the opacity level reaching 200 µ from the epilthelial surface, by pentacam the flattest keratometric readings was 42.6D axis 12.1º and the steepest keratometric readings was 47.4D, the average keratometric reading was 45D, the central pachymetric reading was 556 µ, the uncorrected visual acuity in Snellen lines was 0.05, the autorefractometer reading was -5.75D but there was no further improvement of the best corrected visual acuity on trial of the refraction further than 0.05, the patient refused keratoplasy operation and was referred to the laser ablation unit in the institute and the decision was to perform phototherapeutic keratectomy removing only 100 µ to only decrease the density of the opacity and the patient signed an informed consent. The laser ablation was performed by the Allegretto Wave Light Eye-Q 1010 (400 Hz) with active eye tracker (frequency 400 Hz) by the phototherapeutic keratectomy (PTK) programme removing only 100 µ from the corneal surface (including the epithelium) at 5.0 mm optical zone to avoid development of ectasia in this young female patient, followed by mitomycin C (0.02%) application to ablated stroma for 2 minutes to avoid development of recurrent corneal haze, followed by application of a bandage contact lens. Post-operatively, the patient was given topical antibiotic and steroid drops 4 times/day each and a GABA analogue 2 tablets /day to 2 days to decrease pain sensation. The patient was examined on first, fourth post-operative day where the bandage contact lens was removed after the epithelium had healed. The patient was instructed to increase the frequency of topical steroids to 7 times/day for further two weeks with close monitoring of intraocular pressure by applanation tonometry to guard against steroid induced glaucoma. The uncorrected visual acuity in Snellen lines was re-examined after one month which was found to be improved to 0.5 with no further improvement on trial of refraction. The central pachymetry decreased to 514 µ. The anterior segment OCT revealed the opacity to reach 145 µ from the surface with marked decrease in the density of opacity and the patient was satisfied from the improvement of her visual acuity in Snellen lines from 0.05 preoperatively to 0.5 post-operatively despite lack of complete removal of her corneal opacity (Figure 3).
3. Discussion
Central corneal opacities of various etiologies can be treated by various methods; corneal transplantation whether penetrating [9] or lamellar [10] remained a classical treatment [8], however it is considered a major relatively expensive surgical procedure with delayed visual recovery, and prolonged rehabilitation time before resuming normal daily activities with high rate of complications; including infection, raised intraocular pressure, high post-operative astigmatism and a possibility of graft rejection [16-17]. Phototherapeutic keratectomy is another good treatment modality which had been used in treating superficial corneal opacities with promising results [14-15]. The conjuction of anterior segment OCT added further accuracy to this procedure [11-12]. Hanfer et al. [15] treated 10 eyes with macular dystrophy in which they performed PTK after epithelial debridement and pannus removal and they found that the BCVA increased from 0.3 ± 0.2 preoperatively to 0.6 ± 0.1 after PTK [15], but they don’t apply mitomycin C to ablated bed as in my case series. Al Arfaj et al. [13] had evaluated transepithelial PTK for patients with various causes of superficial corneal opacities and found that their BCVA increased from about 0.48 to about 0.65 [13], but again they don’t apply mitomycin C to ablated bed as in my case series. Li et al. [18], studied 9 eyes of 8 patients with anterior stromal corneal opacities in which PTK was guided by anterior segment OCT, and they found that the operated eyes gained an average of 4.5-line in uncorrected visual acuity and 2.0-line in best spectacle corrected visual acuity that reached to 20/29 [18] but they also did not apply mitomycin C to ablated bed as in my case series. Mitomycin C is an alkylating agent for DNA, which is derived from Streptomyces caespitosus.It was proven that it decreased corneal haze after excimer laser ablation both in animal [19] and human studies [20] by inhibiting DNA/RNA replication in fibroblasts [21]. In this three case series, I added the use of mitomycin C (0.02%) application to stromal bed for 2 minutes after performing transepithelial subtotal PTK to remove central corneal opacities guided by anterior segment OCT and I reported the improvement in the visual acuity in all cases, where; in case one, the BCVA increases from 0.2 to 0.7 without evidence of residual haze, in case two, the BCVA increased from 0.2 to 0.5 with the addition of -1.50D with minimal residual haze, and in case three the UCVA increased from 0.05 to 0.50 with minimal residual haze.The results of this case series were comparable to previously mentioned studies, in spite of not removing the whole depth of the central corneal opacity as determined by anterior segment OCT; the reason for this subtotal removal was to avoid the possibility of ectasia because of thin cornea in the first 2 cases (central pachymetry below 500 µ) and because of the patient being young (below 18 years) female all of which are known risk factors for ectasia, but I combined the use of mitomycin C (0.02%), which is known to be a powerful inhibitor of haze formation after excimer laser correction for reftactive errors. I recommend to have further studies on more cases of central corneal opacities performed by the same protocol used in this case series to confirm the beneficial effects of mitoycin C 0.2% application after PTK in preventing, post-PTK haze formation and possibly decreasing residual haze in unablated tissue.
4. Conclusion
In the presence of relatively non-superficial corneal opacities of various causes, phototherapeutic keratectomy with mitomycin C application; inspite of not removing the whole opacity, yet it can help the patient with marked improvement of visual acuity without the need for keratoplasty.
Financial Disclosure
The author has no proprietary or commercial interest in any of the materials discussed in this article.
Conflicts of Interest
There are no conflicts of interest.
References
- Rush SW, Rush RB. Optical Coherence Tomography-Guided Transepithelial Phototherapeutic Keratectomy for Central Corneal Opacity in the Pediatric Population. Hindawi Journal of ophthalmology (2018): 1-5.
- Maharana PK, Sharma N, Das S, et al. Salzmann’s nodular degeneration. Ocular Surface 14 (2016): 20-30.
- Steger B, Romano V, Biddolph S, et al. Femtosecond Laser-Assisted Lamellar Keratectomy for Corneal Opacities Secondary to Anterior Corneal Dystrophies; An Interventional Case Series. Cornea 35 (2016): 6-13.
- Wright HR, Turner A, Taylor HR. Trachoma. Lancet 371 (2008): 1945-1954.
- Kalezic T, Mazen M, Kuklinski E, et al. Herpetic eye disease study. Current Opinion in Ophthalmology 29 (2018): 340-346.
- Yamazaki ES, Ferraz CA, Hazarbassanov RM, et al. Phototherapeutic keratectomy for the treatment of corneal opacities after epidemic keratoconjunctivitis. Am J Ophthalmol 151 (2011): 35-43.
- Choi H, Ju L, Kim J, et al. Successful Treatment with Combined PTK/PRK Guided by Intraoperative Skiascopy of Patients with Corneal Haze after Surface Ablation. Korean J Ophthalmol 29 (2015): 74-76.
- Garg P, Krishna PV, Stratis AK, et al. Value of corneal transplantation in reducing blindness. Eye 19 (2005): 1106-1114.
- Mathews PM, Lindsley K, Aldave AJ, et al. Etiology of global corneal blindness and current practices of corneal transplantation. Cornea 37 (2018): 1198-1203.
- Singh N, Said DG, Dua HS. Lamellar keratoplasty techniques.Indian Journal of Ophthalmology 66 (2018): 1239-1250.
- Khurana RN, Li Y, Tang M, et al. High-speed optical coherence tomography of corneal opacities. Ophthalmology 114 (2007): 1278-1285.
- Lim LS, Aung HT, Aung T, et al. Corneal imaging with anterior segment optical coherence tomography for lamellar keratoplasty procedures. Am J Ophthalmol 145 (2008): 81-90.
- Al Arfaj K, Jain V, Hantera M, et al. Phototherapeutic Keratectomy Outcomes in Superficial Corneal Opacities. Ophthalmology and Eye Diseases 3 (2011): 1-6.
- Rapuano CJ. Excimer Laser Phototherapeutic Keratectomy for Corneal Dystrophies. Curr Opin Ophthalmol 12 (2001): 288-293.
- Hanfer A, Langenbueher A, Satz B. Long term results of phototherapeutic keratectomy for macular corneal dystrophy. Am J Ophthalmol 140 (2005): 392-396.
- Seng ET, Scott JA, Janardhanan J, et al. Therapeutic keratoplasty for advanced suppurative keratitis. American Journal of Ophthalmology 143 (2007): 755-762.
- Burk RO, Joussen AM. Corneoscleroplasty with maintenance of the angle in two cases of extensive corneoscleral disease. Eye 14 (2000): 196-200.
- Li Y, El Gendy NMS, Huang D. Optical Coherence Tomography Guided Transepithelial Phototherapeutic Keratectomy for Anterior Corneal Opacities. Investigative Ophthalmology and Visual Science 52 (2011): 3376.
- Netto MV, Mohan RR, Sinha S, et al. Effect of prophylactic and therapeutic mitomycin C on corneal apoptosis, cellular proliferation, haze, and long-term keratocyte density in rabbits. J Refract Surg 22 (2006): 562-574.
- Wallau AD, Campos M. One-year outcomes of a bilateral randomized prospective clinical trial comparing PRK with mitomycin C and LASIK. Br J Ophthalmol 93 (2009): 1634-1638.
- Talamo JH, Gollamudi S, Green WR, et al. Modulation of corneal wound healing after excimer laser keratomileusis using topical mitomycin C and steroids. Arch Ophthalmol 109 (1991): 1141-1146.
- Randleman JB, Woodward M, Lynn MJ, et al. Risk Assessment for Ectasia after Corneal Refractive Surgery. Ophthalmology 115 (2008): 37-50.