Spectrum of Resting 12-Lead Electrocardiographic Findings in Peri- Partum Cardiomyopathy: Report of 100 Consecutive Patients
Article Information
Hayatu Umar1*, Adamu Jibril Bamaiyi2
1Department of Internal Medicine, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
2Department of Physiology, Usmanu Danfodiyo University, Sokoto, Nigeria
*Corresponding Author: Hayatu Umar, Department of Internal Medicine, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
Received: 28 June 2020; Accepted: 10 July 2020; Published: 15 July 2020
Citation: Hayatu Umar, Adamu Jibril Bamaiyi. Spectrum of Resting 12-Lead Electrocardiographic Findings in Peri-Partum Cardiomyopathy: Report of 100 Consecutive Patients. Cardiology and Cardiovascular Medicine 4 (2020): 310-323.
View / Download Pdf Share at FacebookAbstract
Electrocardiography (ECG) is an investigative procedure in PPCM screening and monitoring. Although ECG features among PPCM patients have been shown to vary among different ethnicities, this has not been fully described among the Hausa/Fulani ethnicity. In the present study therefore, we described the ECG features of PPCM among Hausa/Fulani ethnic group of Nigeria and we relate same with left ventricular (LV) functions and dimensions. One hundred women who fulfilled the diagnostic criteria for PPCM were evaluated. A standard resting 12-lead ECG and echocardiographic examination were performed on the patients. Data analysis was done using IBM SPSS statistical software (version 22). Mean age of the patients was 27.11 ± 7.83 years and were 98% of the Hausa/Fulani ethnicity. The heart rate (HR) was fast (117.54 ±15.02). Most patients had abnormal ST and T-waves (70% and 83%, respectively). The mean QTc index was 460.97 ±40.69, with 47% of them having prolonged QTc. However, the mean QRS interval was within normal (89.89 ±20.00ms). Although, ejection fraction (EF) showed a significant inverse relationship with the left ventricular internal diameter in diastole (LVIDd) (r = - 0.234, p = 0.021, β-coefficient =-0.013, R2 =0.027), neither of the EF nor the LVIDd showed significant relations with the indices of QRS voltage amplitudes, even though about 82% of the patients had LV dilatation. We conclude that ECG abnormalities are rife among PPCM patients of Hausa/Fulani extraction of Nigeria and may be used alongside other standard protocols to screen and monitor treatment of the patients in this region.
Keywords
Electrocardiography; Hausa/Fulani; Left ventricular function; Left ventricular internal diameter
Article Details
Introduction
Peripartum cardiomyopathy (PPCM) is an important cause of cardiovascular morbidity and mortality in women [1-3]. Although, the disease has been described since early 1800s, and was first described to be associated with heart failure in puerperium by the Rudolf Virchow and Charles Porack [4], its aetiologies and characteristics is still not very clear [5,6]. Furthermore, PPCM profile seems to vary among different races and societies where it is been described [4,7]. North-western Nigeria is probably the “hottest spot” for PPCM, and arguably with the worst outcome, globally [2,8]. Although echocardiography may be the investigative modality of choice for PPCM, this is not as easily accessible, less costly and user friendly as electrocardiographic (ECG) investigation. In this regard, the use of ECG in screening and monitoring of PPCM patients have been suggested in some recent studies [5,6]. Nevertheless, the electrocardiographic (ECG) features of PPCM patients has not been described, as yet among the main ethnicity of the region with the highest burden of the disease. Indeed, majority of PPCM patients have been reported to have ECG abnormalities [1,5,6]. To this extent, a good knowledge of the ECG picture of the patients is important to guide health practitioners in the diagnosis and on appropriate drug use in pregnancy and during breastfeeding among PPCM patients. Moreover, healthcare assessment of PPCM patients is unlikely to be optimum if less expensive modalities are not used, as the health financing system of Nigeria is poorly structured and most patients have to pay out-of-pocket to access cares [9]. Furthermore, PPCM patients may have multiple and diverse presentations on ECG [4,6], therefore early detection of ECG abnormalities in PPCM may help in the holistic management of PPCM and forestall electromechanical complications as well as bad outcome.
We aimed in the present study, to demonstrate the spectrum of electrocardiographic findings in PPCM among the most affected ethnic group (Hausa/Fulani) in the world [1,5,6] and possibly explore the relationship between the ECG findings and left ventricular (LV) systolic function and dimension.
Methods
We consecutively enrolled a total of one hundred and six (106) women of childbearing age, who fulfilled the European Society of Cardiology (ESC) diagnostic criteria for Peri-partum Cardiomyopathy [10,11], aged 15 years and older, in three health facilities. One hundred (94.3%) participants eventually qualified for the study. The study was approved by each of the ethics review committees of the Usmanu Danfodiyo University Teaching Hospital (UDUTH), Sokoto, Specialist Hospital, Sokoto and Medistop Clinical Diagnostic Center, Sokoto. All the enrolled patients gave their informed written consents. The regulations concerning human research, as stated in the Helsinki declaration (World Medical, 2013) were followed. The patients enrolled include female patients seen at the above three health centres, between January, 2018 to June, 2019. Patients demographic and other clinical information were retrieved from completed structured questionnaires. Relevant perinatal related cultural practices such as traditional hot bath and ingestion of pap made with millet and rich in dry lake salt (‘’Kununkanwa’’ in Hausa) were also noted in the questionnaire. Each patient was specifically asked about symptoms suggestive of left-sided and right-sided heart failure.
General physical and systemic examination
- New York Heart Association (NYHA) heart failure functional classes were determined on admission
- Anthropometric measurements e.g. weight, height, body mass index (BMI), were determined using standard procedures
- A special attention was given to pulse (rate, rhythm, volume and character)
- Standard procedures were followed in measuring brachial blood pressure, using Accuson mercury sphygmomanometer
- Presence of raised jugular venous pressure (JVP), apex beat location, character, thrills, third heart sound (S3) gallop, variability of first heart sound (S1), loud second heart sound pulmonary component (P2), murmurs, respiratory rate, oxygen saturation, bi-basal fine or coarse crepitations, signs of pleural effusion were assessed
- Pitting pedal edema, congestive hepatomegaly and ascites were also assessed
Inclusion criteria
The study included childbearing women aged 15 years and above, who were diagnosed of heart failure in the last month of pregnancy or within 5 month of child birth, who met ESC diagnostic criteria for Peri-partum cardiomyopathy [11] and underwent resting 12-lead ECG.
Exclusion criteria
Excluded in the present study are, patients below 15 years of age, those who passed away shortly after enrollment before complete clinical, ECG and echocardiography evaluation were carried out. Patients with poor echo window and participants with known clinical e.g. diabetes mellitus, hypertension, thyrotoxicosis, sickle cell anemia, rheumatic heart disease and social history alcoholism, were excluded in the present study.
Electrocardiography
Standard resting 12 lead Electrocardiography (ECG) was performed with lead II recorded for long rhythm strip. The recommendation of the American Heart Association (AHA) [12], concerning standardization of the leads and specification for instrument was followed and relevant abnormal findings were noted for each patient. Atrial and ventricular rate, rhythm, P-R interval, QRS duration/abnormality and axis in frontal plane directed to the region between 0° to -90° was taken as left axis deviation and normal QRS axis was -30° to +115°. QTc interval were measured and noted. Right atrial enlargement (RAE) indicated as the presence of peaked P wave with amplitude of 2.5mm or more in lead II, III and avF. Left atrial enlargement (LAE) indicated as the presence of notched P with duration of 0.12 sec or more or defined as P terminal force in V1 equal or more negative than -0.04 mm sec. Bi-atrial enlargement was expressed as presence of the existence of criteria for both RAE and LAE or demonstration of huge diphasic P wave in lead V1 where the initial positive component measured above 1.5mm and the terminal negative component measured 1mm in depth and 0.04 sec in duration. Left ventricular hypertrophy (LVH) was defined by Sokolow-Lyon criteria [13] as S-wave in V1 + R-wave in V5 or V6 > 35mm or as defined by Araoye criteria S-wave in V2 + R-wave in V5 or V6 ≥35mm in female or ≥40mm in male [14]. Right ventricular hypertrophy (RVH) was defined as (a) R wave in V1 ≥7mm (b) R/S ratio V1 > 1 or alternatively R/S ratio in V5 or V6 <1 (c) R wave in V1+S wave in V5 or V6 > 10.5mm (d) qR complex in V1. Bi-ventricular hypertrophy defined as meeting the criteria for both LVH and RVH. The ratio of R-wave in V6 and maximum R-wave in lead I, II, III were determined and the ratio of RV6/Rmax was calculated to find out the correlation of this ratio with ejection fraction and ventricular dilatation [15]. ST segment and T wave abnormalities were noted as well as supraventricular tachy-arrythmias (SVT), brady-arrythmias, ventricular arrhythmias, heart blocks, atrial, junctional, ventricular premature contractions were noted, and other uncommon ECG abnormalities were also taken note of.
Echocardiography
Echocardiographic examination was performed with the patient in the partial left lateral decubitus position using Sonascape SSI-5000 ultrasound imaging system with a 1-6 MHz transducer. Two-dimensional (2-D) guided motion mode (M-mode) were obtained as recommended by the American Society of Echocardiography (ASE) [16]. Doppler studies were also obtained with transthoracic echocardiography (TTE). Measurements were obtained in accordance with the recommendation of the leading edge to leading edge procedures. Calculations were made using the in-built analysis software of the echocardiographic machine. The 2-D views were used for real time morphological characteristics and also as a reference for selection of the M–mode beam. The echo views utilized for the study included parasternal long axis view, short axis view, apical 4-chamber view, and 5 chamber view. These views and measurements were used to examine pericardial and cardiac cavity, wall dimensions, aortic dimension, wall motion abnormalities, valve morphology, motion and dimension, chamber dimensions and appearance as well as systolic function; intramural thrombus, septal defect, valvular vegetations were all looked for. Recording of the mitral inflow were obtained from apical 4-chamber view in order to assess left ventricular (LV) filling dynamics and grade the LV diastolic dysfunction accordingly. The presence and magnitude of regurgitation across heart valve was assessed by color Doppler echocardiography, color Doppler regurgitant jet area of atrium area or wall impending jet of any size, swirling in the atrium method was used to determine a grade of mild (<20%), moderate (20-40%) or severe (>40%) [17], and pulmonary arterial pressure was also determined.
Other Relevant Investigations
Hemogram (Hb), Fasting blood sugar (FBS), Fasting lipid profile (FLP), and serum urea, electrolyte and creatinine, chest X-ray (PA view) were also determined.
Statistical Analysis
Data storage and analysis was completed with IBM SPSS software (version 22 for windows Inc., Chicago, IL, USA). Mean and standard deviations were computed for quantitative variables. Baseline characteristics were described using summary statistics, as appropriate. Where values are expressed as qualitative, proportions or percentages are used and also presented as either tables or graphs of frequencies. Where relationship between quantitative variables are required person correlation coefficient were applied. A two-sided P-value of<0.05 was considered as level statistical significance.
Results
Social demographic information of the patients
The population of patients studied are predominantly of Hausa/Fulani Muslims, and it is typical of north - western Nigerian region (Table 1). The average age of the patients was 27.11 ± 7.83 years, with the average weight/BMI was within normal limits (Table 1). The average height of the patients was similarly within normal limits (>150cm).
Although most of the patients were married, the level of formal education was abysmally poor, and most of them are unemployed, therefore most of the patients are of the low social economic group (Table 1).
Most of the patients were delivered of singleton pregnancies and most of them have less than five children, with 21% of the patients having more than four children (tTable 1). Most of them had blood pressure in the normal range (<140mmHg), with the sample population average of 108.6 ±14.7 mmHg (70 – 160mmHg). See Table 1.
|
Variable |
Frequencies (%) |
|
Age ± SD (years) |
27.11 ± 7.83 |
|
Weight ± SD (kg) |
56.77 ± 11.42 |
|
Height ± SD (cm) |
159.04 ± 17.86 |
|
BMI ± SD (Kg/M2) |
21.51 ± 4.01 |
|
SBP ± SD (mmHg) |
108.6 ± 14.7 |
|
SBP categories: <140 |
86 (86.0%) |
|
≥140 |
14 (14.0%) |
|
EF ± SD (%) |
36.94 ± 7.44 |
|
Occupation: Unemployed |
99 (99.0) |
|
Farmer |
1 (1.0) |
|
Marital status: Married |
97 (97.0) |
|
Divorced on admission |
1 (1.0) |
|
Divorced after admission |
2 (2.0) |
|
Education status: Quranic |
71 (71.0) |
|
Primary |
12 (12.0) |
|
Secondary |
13 (13.0) |
|
Tertiary |
4 (4.0) |
|
Tribe: Hausa/Fulani |
98 (98.0) |
|
Others |
2 (2.0) |
|
Religion: Islam |
97 (97.0) |
|
Christianity |
3 (3.0) |
|
Twin gestation: Yes |
7 (7.0) |
|
No |
93 (93.0) |
|
Parity: Para 1 |
37 (37.0) |
|
Para 2 |
17 (17.0) |
|
Para 3 |
13 (13.0) |
|
Para 4 |
12 (12.0) |
|
Para 5 |
5(5.0) |
|
Para ≥ 6 |
16(16.0) |
|
NYHA functional class at presentation: Class I |
- |
|
Class II |
8(8.0) |
|
Class III |
24(24.0) |
|
Class IV |
68(68.0) |
|
Outcome: Alive |
95(95.0) |
|
Dead (in-hospital) |
5(5.0) |
Table 1: Demographic and relevant clinical characteristics of the patients (n=100)
Abbreviation: SBP = Systolic blood pressure, EF = Ejection fraction, BMI = Body mass index
PR interval and QRS complex duration
PR interval and QRS complex duration were within normal limit of normal (120ms -200ms and 60 -100ms, respectively) (Table 2).
QTc and HR of the patients:
Both the HR and the QT interval corrected for HR (QTc) were higher than the normal range.
QRS amplitudes and axis of the patients:
About 35% of the patients had various form of low QRS voltage amplitudes, but about 65% of them had normal amplitude (Table 2).
Heart block characteristics of the patients:
Only 3% of the patients had LBBB. Similarly, left anterior hemi-block and first-degree heart block were each recorded in two patients (Table 2).
ST changes and T-wave profiles of the patients:
Most of the patients (66.0%) had ST depression, with only 30.0% of the patients having normal pattern. Similarly, T wave was inverted in 54.0% of the patients, and 29.0% of them showed T wave flattening, with only 17.0% showing normal T wave (Table 2).
Special and rare ECG findings in some of the patients
One patient showed ventricular premature complex (VPC), of the bigeminy type. Atrioventricular nodal re-entrant tachycardia (ANRT) was seen in a patient, Sinus node re-entrant tachycardia (SNRT) was observed in one patient, and Wolf-Parkinson-White syndrome was seen in a patient.
|
Parameters |
Frequencies (%) |
|
PR interval ± SD (ms) |
139.52 ± 25.97 |
|
QRS duration ± SD (ms) |
89.89 ±20.00 |
|
QTc ± SD |
460.97 ± 40.69 |
|
Prolonged QTc |
47(47.0) |
|
HR ± SD (bpm) |
117.54 ± 15.02 |
|
QRS axis: Normal |
72 (72.0) |
|
LAD |
27 (27.0) |
|
RAD |
1 (1.0) |
|
Sinus tachycardia: |
92(92.0) |
|
Atrial flutter: |
1(1.0) |
|
Atrial fibrillation: |
2(2.0) |
|
Ventricular premature complex (interpolated VPC): |
5 (5.0) |
|
Ventricular bigeminy |
1(1.0) |
|
Wolf-Parkinson-White syndrome |
1(1.0) |
|
AV nodal re-entrant tachycardia |
1(1.0) |
|
Sinus node re-entrant tachycardia |
1(1.0) |
|
First degree heart block |
2(2.0) |
|
LBBB: Yes |
3 (3.0) |
|
Left anterior hemi-block |
2 (2.0) |
|
ST changes: Normal |
30 (30.0) |
|
ST elevation |
4 (4.0) |
|
ST depression |
66 (66.0) |
|
T-wave changes: Normal |
17 (17.0) |
|
Flattening |
29 (29.0) |
|
Inversion |
54 (54.0) |
Table 2: ECG features in PPCM patients (n =100)
Abbreviations: HR = Heart rate, LBBB =Left bundle branch block
Ventricular remodeling
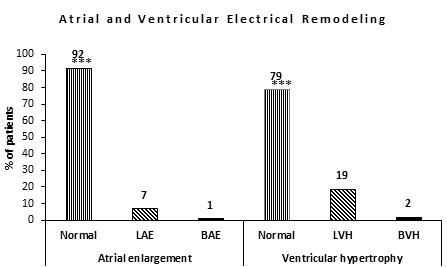
Seventy-nine percent of the patients had no ventricular hypertrophy by ECG criteria, while 21.0% of them showed electrical remodeling. Of the 21.0%, 19.0% are of LVH category, while the remaining 2.0% presented with both right and left ventricular hypertrophies. See Figure 1.
Atrial remodeling
Ninety-two percent of the patients had no atrial enlargement based on ECG criteria. But 7.0% of them had left atrial enlargement (LAE) and just 1.0% of the patient had bi-atrial enlargement. See Figure 1.
Heart rhythms
Majority of the patients (84%) had sinus tachycardia (average HR of 117.54 ± 15.02 bpm) Table 1, while just 7 (7.0%) had sinus rhythm.
Abbreviations: LAE =Left atrial enlargement, BAE = Bi-atrial enlargement, LVH = Left ventricular hypertrophy, BVH = Bi-ventricular hypertrophy NB: *** =p<0.0005, ** p=<0.005, * =p<0.05
|
LV functions |
QRS voltage indices |
r |
p |
Standardized β-coefficient |
R2 |
|
EF: v |
RV6 |
0.072 |
0.485 |
-0.075 |
0.004 |
|
v |
Rmax |
0.081 |
0.438 |
-0.235 |
0.009 |
|
v |
RV6/Rmax |
-0.053 |
0.615 |
0.242 |
0.001 |
|
v |
LVIDd |
-0.234 |
0.021 |
-0.013 |
0.027 |
|
LVIDd: v |
RV6 |
-0.013 |
0.904 |
-2.718 |
0.027 |
|
v |
Rmax |
-0.049 |
0.641 |
-2.856 |
0.008 |
|
v |
RV6/Rmax |
0.039 |
0.706 |
-11.696 |
0.001 |
Table 3: LV functions and QRS voltage amplitude indices
Abbreviations: LV =Left ventricle, EF =Ejection fraction, LVIDd = LV = internal diameter in diastole, r = Pearson’s correlation coefficient, R2 = Coefficient of determination, Rmax = Tallest R in leads I, II and III
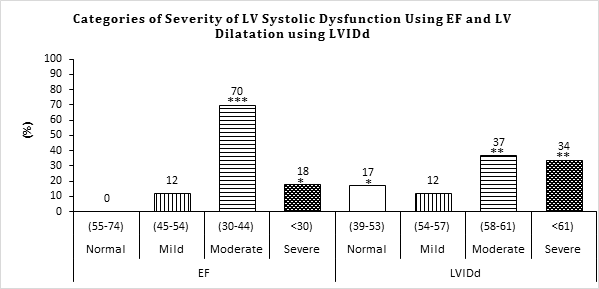
Abbreviations: EF =Ejection fraction, LVIDd = LV = internal diameter in diastole
NB: *** =p<0.0005, ** p=<0.005, * p=<0.05
Although LV chamber dilatation (LVIDd) showed a significant, but opposite relationship with the EF (r = -0.234, p =0.021) among the PPCM patients, EF did not show any significant relationships with RV6, Rmax or RV6/Rmax (see Table 3). Similarly, LVIDd showed opposite variations with RV6 and Rmax, but these were not significant. LVIDd also showed a non-significant relationship with RV6/Rmax, but in same direction (see Table 3). The findings above were well corroborated by the standardized β-coefficients and their corresponding coefficient of determinations among the LV functions (EF and LVIDd) and QRS voltage indices (see Table 3).
In Figure 2/Table 4, most of the patients (83%) have LV dilatation. But none of the patients are of normal category of EF.
Discussions
Our main findings in the present study are; most of the patients had sinus tachycardia, abnormal ST patterns and T-wave abnormalities. In the majority of the patients however, there were normal QRS complex, PR interval, amplitude of QRS voltage, QRS axis and QTc index. Although, a study in Nigeria [6], asserted the use of the trio of HR, ST-T abnormalities and prolonged QRS complex duration to screen for PPCM, we report in the present study, normal QRS complex duration in 90% of the patients. Beside the fact that the above study is suggested to screen PPCM, not confirmatory, our findings may not be unconnected that majority of the patients had no LVH by ECG criteria. In this regard, prolonged QRS complex duration (>110ms) is associated with LVH [6,18].
The present study also reported some of the demographic characteristics of the patients to be within the normal ranges, including weight, height, BMI and systolic BP. However, the patients tend to present with PPCM at a younger age compared with values reported in earlier studies. Furthermore, almost all the patients were not gainfully employed, most did not receive formal educations and are in the majority of cases married, but among other co-wives.
Although PPCM has been described about 200 years ago [4], the disease is still a major cause of morbidity and mortality, with aetiologies that are not properly understood [5,6]. In this regard, the present study presented some ECG findings and other demographic parameters that negate the submissions of earlier studies [1,5,6]. Indeed, age, gender, race and geographic differences, all tend to modify the electrocardiographic picture among PPCM patients [4,19].
QRS duration
Even though the patients had normal QRS duration in the majority, they satisfied the definition for PPCM. QRS duration may be prolonged in PPCM [6] and it may be associated with LVH [19,20], and may be due to tachycardia, heart blocks or Wolff-Parkinson-White (WPW) syndrome [20]. In this regard, although the average HR of our patients was faster than normal, heart block and WPW syndrome were rare findings in the present study. Furthermore, our patients being younger and mostly of the normal systolic BP range, may further explain why the QRS duration was not prolonged.
HR and QTc
The patients demonstrated sinus tachycardia. Similarly, about 47% of the patients had prolonged QTc index. Although, both fast HR (>100 bpm), and prolonged QTc (>460 ms) [14,21] are both said to be associated with poor cardiovascular outcome [22-24], only 5% of mortality was recorded in-hospital in the present study. However, this mortality figure may be a “tip-of- the-iceberg”, as the patients were not followed up after discharged from the hospital, to monitor post-discharge complications or mortalities.
QRS axis and QRS amplitude
Majority of the patients had normal QRS axis and just above a quarter of them having LAD. The normal axis in the majority of the patients may be explained by the fact that most of them had no ventricular hypertrophy (Figure 1). And the LAD may be due to pregnancy induced increase in intra-abdominal pressure. Indeed, mechanical effects of pregnancy may be associated with LAD [25].
About a quarter of the patients had low QRS voltage amplitude in both the precordial and limb leads. Overall, however, majority of them presented with normal QRS amplitude. Though, the absence of low voltage QRS amplitude doesn’t rule out PPCM, low QRS voltage has been described as a feature of dilated cardiomyopathy [25].
LV functions and QRS voltage amplitudes
Although EF showed a significant inverse relationship with LVIDd, this was a weak one (r = -0.234, p = 0.021, β-coefficient =-0.013, R2 =0.027). There was no significant relationship between the EF and RV6, Rmax or RV6/Rmax. Indeed, the mean RV6, 13.78 ±5.80 (3.00-32.00) was low, compared to the ≥15mm reported by Momiyama, Mitamura [26] in dilated cardiomyopathy (DCM) and it may explain the lower RV6 and Rmax ratio obtained, 2.30 ± 0.97 (0.30-6.00), when compared with the 3.40 reported by Momiyama, Mitamura [15] among patients with DCM. Similarly, LVIDd showed no significant relationship RV6, Rmax or RV6/Rmax among the patients.
In the present study, the design was a cross-sectional descriptive type, making it impossible to carry out serial records for comparison. The findings in the present study may also be explained by the fact that only about 20% of the patients had ventricular hypertrophies (left ventricular or bi-ventricular hypertrophies). Further, the study being compared with the present study was on DCM in the non-pregnant patient, not PPCM. However, about 82% of the patients had LV dilatation, with mean of 58.10 ±11.87mm, which is within moderate range of LV dilatation [27]. This is an important finding in PPCM, as systolic dysfunction (of the LV) is an important component of PPCM. Indeed, EF is inversely proportional to LVIDd [15,26,28,29]. Moreover, while QRS voltage amplitude is directly proportional to the degree of LV dilatation in DCM patients [26,29], the EF is inversely proportional to the extent of LV dilatation [15,26].
ST-T, and T wave changes
The present study showed ST segment depression in a substantial proportion of the patients and few numbers of elevations. Overall, the ST segments were mainly abnormal. Indeed, ST segment abnormalities are features of PPCM [5,6].
We report T wave abnormalities, including inversion and flattening in majority of the patients. Only a few of the patients had normal T wave pattern, which still does not rule out PPCM in them1. In this regard, earlier reports [5,10,19] have described abnormal T wave in PPCM patients.
Social demographic characteristics of the patients
Poor literacy level and low economic powers among the patients were reported as independent risk factors for PPCM in a recent study on PPCM by the PEACE registry group [30]. The present study is in tandem with that findings, as most of our patients had no formal education, not gainfully employed and are mostly married, but as a wife among other co-wives, this together translates to poor economic disposition.
Conclusion
We conclude in the present study, that ECG abnormalities are common among PPCM patients of Hausa/Fulani extraction, Northwestern Nigeria, where the burden of the disease is probably the highest. The ECG parameters in this group showed some variations compared to results obtained elsewhere. Indeed, even though they showed LV dilatations and characterized by low EF, these does not bear significant relationship with the QRS voltage amplitudes in the patients. Nevertheless, ECG may be used alongside other standard protocols to screen and monitor treatment of the patients in this region.
Study limitations
The present study is limited by the fact that we did not follow-up the patients to be able to correlate our ECG findings with patients’ survival, post management. We also regret that the study time is not long enough, so we couldn’t expand the sample size beyond the present figure. Further studies will be required to address the above limitations.
Acknowledgement
We sincerely thank our patients for consenting to participate in the study. We also appreciate Mr. Jonathan Isiah for technical assistance with the ECG.
References
- Honigberg MC, Elkayam U, Rajagopalan N, et al. Electrocardiographic findings in peripartum cardiomyopathy. Clinical cardiology 42 (2019): 524-9.
- Danbauchi S, Oyati A, Isa M, Alhassan M. Peripartum cardiomyopathy. Nigerian Journal of Cardiology 11 (2014): 66-73.
- Soma-Pillay P, Seabe J, Sliwa K. The importance of cardiovascular pathology contributing to maternal death: Confidential Enquiry into Maternal Deaths in South Africa, 2011-2013. Cardiovascular journal of Africa 27 (2016): 60-5.
- Arany Z, Elkayam U. Peripartum Cardiomyopathy. Circulation 133 (2016): 1397-409.
- Tibazarwa K, Lee G, Mayosi B, Carrington M, Stewart S, Sliwa K. The 12-lead ECG in peripartum cardiomyopathy. Cardiovascular journal of Africa 23 (2012): 322-9.
- Karaye KM, Lindmark K, Henein MY. Electrocardiographic predictors of peripartum cardiomyopathy. Cardiovascular journal of Africa 27 (2016): 66-70.
- Lee YZJ, Judge DP. The Role of Genetics in Peripartum Cardiomyopathy. J Cardiovasc Transl Res 10 (2017): 437-45.
- Isezuo SA, Abubakar SA. Epidemiologic profile of peripartum cardiomyopathy in a tertiary care hospital. Ethnicity & disease 17 (2007): 228-33.
- Ogah OS, Stewart S, Onwujekwe OE, et al. Economic burden of heart failure: investigating outpatient and inpatient costs in Abeokuta, Southwest Nigeria. PloS one 9 (2014): e113032-e.
- Bauersachs J, König T, van der Meer P, et al. Pathophysiology, diagnosis and management of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Study Group on peripartum cardiomyopathy. European journal of heart failure 21 (2019): 827-43.
- Sliwa K, Hilfiker-Kleiner D, Petrie MC, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. European journal of heart failure 12 (2010): 767-78.
- KOSSMANN CE, BRODY DA, BURCH GE, et al. Recommendations for Standardization of Leads and of Specifications for Instruments in Electrocardiography and Vectorcardiography. Circulation 35 (1967): 583-602.
- Sokolow M, Lyon TP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. 1949. Ann Noninvasive Electrocardiol 6 (2001): 343-68.
- Ogunlade O, Akintomide AO. Assessment of voltage criteria for left ventricular hypertrophy in adult hypertensives in south-western Nigeria. J Cardiovasc Dis Res 4 (2013): 44-6.
- Momiyama Y, Mitamura H, Kimura M. ECG characteristics of dilated cardiomyopathy. Journal of Electrocardiology 27 (1994): 323-8.
- Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation 58 (1978): 1072-83.
- Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and doppler echocardiography. Journal of the American Society of Echocardiography 16 (2003): 777-802.
- Surawicz B, Childers R, Deal BJ, Gettes LS. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram. Circulation 119 (2009): e235-e40.
- Surawicz B, Childers R, Deal BJ, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 119 (2009): e235-e40.
- Ogunlade O. Causes of broad QRS complex. ECG nuggets. OAU, Ile-Ife, Osun State, Nigeria: DO Foundation; 2018: 34-5.
- Viskin S. The QT interval: too long, too short or just right. Heart rhythm 6 (2009): 711-5.
- Brendorp B, Elming H, Jun L, et al. Qtc interval as a guide to select those patients with congestive heart failure and reduced left ventricular systolic function who will benefit from antiarrhythmic treatment with dofetilide. Circulation 103 (2001): 1422-7.
- Chen X-j, Barywani SB, Hansson P-O, et al. Impact of changes in heart rate with age on all-cause death and cardiovascular events in 50-year-old men from the general population. Open heart 6 (2019): e000856.
- Böhm M, Schumacher H, Teo KK, et al. Resting heart rate and cardiovascular outcomes in diabetic and non-diabetic individuals at high cardiovascular risk analysis from the ONTARGET/TRANSCEND trials. European heart journal 41 (2020): 231-8.
- Ogunlade O. Causes of alteration in QRS axis. ECG nuggerts. Revised first edition ed. OAU, Ile-Ife, Osun state, Nigeria: DO foundation 2018: 48-9.
- Momiyama Y, Mitamura H, Kimura M. ECG differentiation of idiopathic dilated cardiomyopathy from coronary artery disease with left ventricular dysfunction. Journal of Electrocardiology 28 (1995): 231-6.
- Narayanan K, Reinier K, Teodorescu C, et al. Left ventricular diameter and risk stratification for sudden cardiac death. Journal of the American Heart Association 3 (2014): e001193-e.
- Feldman T, Borow KM, Neumann A, Lang RM, Childers RW. Relation of electrocardiographic R-wave amplitude to changes in left ventricular chamber size and position in normal subjects. The American journal of cardiology 55 (1985): 1168-74.
- Feldman T, Childers RW, Borow KM, Lang RM, Neumann A. Change in ventricular cavity size: differential effects on QRS and T wave amplitude. Circulation 72 (1985): 495-501.
- Karaye KM, Ishaq NA, Sa'idu H, et al. Incidence, clinical characteristics, and risk factors of peripartum cardiomyopathy in Nigeria: results from the PEACE Registry. ESC Heart Failure 7 (2020):235-43.