Risk Factors Associated With Malaria Mortality in Tshwane District, South Africa: A Retrospective Cohort Study, 2011-2014
Article Information
Mphaka MR1, 2, 3*, Moshime M3, Tsilo LC2, Reddy C1
1South African Field Epidemiology Training Programme, National Institute of Communicable Diseases, South Africa
2School of Health Systems and Public Health, University of Pretoria, South Africa
3Tshwane district: Expanded Programme on Immunization/Communicable Disease Control and Outbreak Response Directorate, Department of Health, South Africa
*Corresponding Author: Mphaka MR, South African Field Epidemiology Training Programme, National Institute of Communicable Diseases, South Africa
Received: 23 November 2018; Accepted: 28 May 2019; Published: 01 July 2019
Citation: Mphaka MR, Moshime M, Tsilo LC, Reddy C. Risk Factors Associated With Malaria Mortality in Tshwane District, South Africa: A Retrospective Cohort Study, 2011-2014. Journal of Environmental Science and Public Health 3 (2019): 289-297.
View / Download Pdf Share at FacebookAbstract
Background: Tshwane District in Gauteng Province identifies malaria cases from endemic provinces and neighbouring countries as well as Odyssean malaria cases.
Objectives: To assess changes in malaria morbidity and mortality and to determine risk factors associated with malaria mortality in Tshwane District during 2011-2014.
Methods: A retrospective cohort study was conducted using malaria surveillance data collected by the Communicable Disease Control Directorate in Tshwane district over a period of four years. Only laboratory confirmed cases were enrolled in the study. Secondary death audits were reviewed. Logistic regression determined risk factors associated with malaria mortality.
Results: During 2011-2014, 964 cases were identified. Of these, the median age was 28 years (range: 4 months to 79 years), 71.7% (n=691) were males. The majority of cases, 96.6% (n=931), had travelled to malaria endemic areas within South Africa and neighbouring countries. Of those who travelled to endemic malaria provinces in South Africa, 62.5% (40/64) went to Limpopo. Malaria cases decreased from 333 in 2011 to 229 in 2014. There were 20 deaths (2.1%) and 19 (2.0%) Odyssean malaria cases. Age, gender and malaria season were not associated with mortality. History of travel to a malaria endemic area was a protective factor for mortality (aOR 0.2, 95%CI: 0.36 to 0.78, p=0.021).
Conclusion: In this non-endemic district, a number of malaria cases have been reported. Public awareness regarding uptake of antimalarial prophylaxis before and during travel to endemic areas cou
Keywords
Malaria, Tshwane district, Mortality, Risk factors, Endemic, Surveillance
Malaria articles Malaria Research articles Malaria review articles Malaria PubMed articles Malaria PubMed Central articles Malaria 2023 articles Malaria 2024 articles Malaria Scopus articles Malaria impact factor journals Malaria Scopus journals Malaria PubMed journals Malaria medical journals Malaria free journals Malaria best journals Malaria top journals Malaria free medical journals Malaria famous journals Malaria Google Scholar indexed journals Mortality articles Mortality Research articles Mortality review articles Mortality PubMed articles Mortality PubMed Central articles Mortality 2023 articles Mortality 2024 articles Mortality Scopus articles Mortality impact factor journals Mortality Scopus journals Mortality PubMed journals Mortality medical journals Mortality free journals Mortality best journals Mortality top journals Mortality free medical journals Mortality famous journals Mortality Google Scholar indexed journals Risk factors articles Risk factors Research articles Risk factors review articles Risk factors PubMed articles Risk factors PubMed Central articles Risk factors 2023 articles Risk factors 2024 articles Risk factors Scopus articles Risk factors impact factor journals Risk factors Scopus journals Risk factors PubMed journals Risk factors medical journals Risk factors free journals Risk factors best journals Risk factors top journals Risk factors free medical journals Risk factors famous journals Risk factors Google Scholar indexed journals Endemic articles Endemic Research articles Endemic review articles Endemic PubMed articles Endemic PubMed Central articles Endemic 2023 articles Endemic 2024 articles Endemic Scopus articles Endemic impact factor journals Endemic Scopus journals Endemic PubMed journals Endemic medical journals Endemic free journals Endemic best journals Endemic top journals Endemic free medical journals Endemic famous journals Endemic Google Scholar indexed journals Surveillance articles Surveillance Research articles Surveillance review articles Surveillance PubMed articles Surveillance PubMed Central articles Surveillance 2023 articles Surveillance 2024 articles Surveillance Scopus articles Surveillance impact factor journals Surveillance Scopus journals Surveillance PubMed journals Surveillance medical journals Surveillance free journals Surveillance best journals Surveillance top journals Surveillance free medical journals Surveillance famous journals Surveillance Google Scholar indexed journals Communicable Diseases Control articles Communicable Diseases Control Research articles Communicable Diseases Control review articles Communicable Diseases Control PubMed articles Communicable Diseases Control PubMed Central articles Communicable Diseases Control 2023 articles Communicable Diseases Control 2024 articles Communicable Diseases Control Scopus articles Communicable Diseases Control impact factor journals Communicable Diseases Control Scopus journals Communicable Diseases Control PubMed journals Communicable Diseases Control medical journals Communicable Diseases Control free journals Communicable Diseases Control best journals Communicable Diseases Control top journals Communicable Diseases Control free medical journals Communicable Diseases Control famous journals Communicable Diseases Control Google Scholar indexed journals malaria endemic countries articles malaria endemic countries Research articles malaria endemic countries review articles malaria endemic countries PubMed articles malaria endemic countries PubMed Central articles malaria endemic countries 2023 articles malaria endemic countries 2024 articles malaria endemic countries Scopus articles malaria endemic countries impact factor journals malaria endemic countries Scopus journals malaria endemic countries PubMed journals malaria endemic countries medical journals malaria endemic countries free journals malaria endemic countries best journals malaria endemic countries top journals malaria endemic countries free medical journals malaria endemic countries famous journals malaria endemic countries Google Scholar indexed journals Economic Community articles Economic Community Research articles Economic Community review articles Economic Community PubMed articles Economic Community PubMed Central articles Economic Community 2023 articles Economic Community 2024 articles Economic Community Scopus articles Economic Community impact factor journals Economic Community Scopus journals Economic Community PubMed journals Economic Community medical journals Economic Community free journals Economic Community best journals Economic Community top journals Economic Community free medical journals Economic Community famous journals Economic Community Google Scholar indexed journals healthcare facilities articles healthcare facilities Research articles healthcare facilities review articles healthcare facilities PubMed articles healthcare facilities PubMed Central articles healthcare facilities 2023 articles healthcare facilities 2024 articles healthcare facilities Scopus articles healthcare facilities impact factor journals healthcare facilities Scopus journals healthcare facilities PubMed journals healthcare facilities medical journals healthcare facilities free journals healthcare facilities best journals healthcare facilities top journals healthcare facilities free medical journals healthcare facilities famous journals healthcare facilities Google Scholar indexed journals
Article Details
1. Introduction
Malaria is a life threatening parasitic disease which is transmitted to humans by the bite of an infected female anopheles mosquito [1]. It is one of the leading causes of morbidity and mortality in endemic countries [2]. There has been a global decline of malaria incidence by 17% and malaria mortality by 26% since 2000 [3]. There was an estimated 214 million cases of malaria and 438 000 deaths in 2015 and a global decrease of 37% in malaria incidence and 60% in malaria deaths between 2000 and 2015 [1]. There are potential risk factors which may have a significant impact on malaria transmission such as the level of mosquito control measures, population immunity, social and economic status (housing conditions), and environmental factors including rainfall and temperatures. Resistance to antimalarial drugs has been attributed to an increase in mortality [4]. In Africa, malaria is mostly caused by Plasmodium falciparum (P. falciparum) as opposed to P. ovale, P. vivax, P. malariae, and P. knowlesi [3, 5]. 90% of malaria infections in South Africa are caused by P. falciparum, which is more virulent [6, 7]. Previous studies have shown that people who are at high risk of dying from malaria are pregnant women whose immunity is decreased by pregnancy, children <5 years of age with immature immune systems, immunocompromised people and travellers from non-endemic areas into malaria endemic areas [8]. Malaria is under surveillance and is a notifiable condition in South Africa [9]. The number of reported malaria cases and deaths is used to guide public health interventions to inform policy decision making and to track progress of malaria control programmes. There are three malaria endemic provinces: Limpopo, KwaZulu-Natal and Mpumalanga [9].
2. Methods
2.1 Study design
Ethical approval was obtained from University of Pretoria Ethics Committee. Permission to use the surveillance data was obtained from Tshwane research committee and Communicable Diseases Control (CDC) programme manager. A retrospective cohort study was conducted using malaria surveillance data collected by the Communicable Disease Control Directorate in Tshwane district during 2011-2014. The surveillance data was received from both private and public health facilities. The reporting sites included eight public hospitals, 35 private hospitals, 22 municipal clinics and 49 public clinics. Only laboratory confirmed malaria cases were enrolled in the study. For each malaria death in Tshwane district, an audit is conducted using a special tool to assess risk factors associated with malaria mortality, therefore, secondary death audits were reviewed. The secondary death audit data were used to describe the risk factors associated with malaria mortality in Tshwane district.
2.2 Study site and population
The study was conducted in Tshwane district, which is one of five districts in Gauteng province. Tshwane is the second largest municipality in Gauteng with a population of approximately 2.9 million [12]. The study included individuals who resided in urban and rural settlements within the seven sub-districts of Tshwane, both males and females and all age groups who consulted in health facilities and were laboratory confirmed malaria cases.
2.3 Data management
Data was cleaned and validated including identification of duplicates using Microsoft Excel 2013. Information collected during research was kept confidential. The names of participants involved in the study were not mentioned during report writing. Data was stored on a password protected computer.
2.4 Data analysis
Time series plots were constructed to analyze changes in malaria cases over the period of four years (2011-2014). Univariate and multivariate logistic regression analysis was used to determine risk factors for malaria mortality. The potential risk factors including age, gender, travel history and malaria season were considered. Risk factors with p-values less than 0.2 in the univariate logistic regression models were introduced into the multivariate model. Statistically non-significant risk factors were removed using the manual forward stepwise procedure, starting with those that were highly significant. In all statistical tests, a p value less than 0.05 was considered to be statistically significant. Data was analysed using STATA version 13 and Microsoft Excel 2013.
3. Results
Between 2011 and 2014, a total of 964 cases were diagnosed with malaria and were notified by public and private hospitals to the Tshwane district Communicable Disease Control (CDC) Directorate. Of these, 19 cases, including one death were Odyssean malaria cases. The median age was 28 years (range: 4 months to 79 years). The age group 25-34 years was more affected compared to other age groups. Males were more affected than females in all the years of study (2011-2014) (Table 1). Almost all cases (99.8%) were caused by P. falciparum. The majority of cases, 96.6% (n=931) had travelled to malaria endemic areas within South Africa and neighbouring countries predominantly Mozambique (52.6%) (Figure 1). Of all cases, 19 did not have travel history. None of the cases had taken chemoprophylaxis before they travelled as indicated on the notification forms received by the CDC directorate.
|
Age (years) |
2011 |
2012 |
2013 |
2014 |
N |
% |
|
0-5 |
21 |
32 |
30 |
32 |
115 |
12% |
|
6-14 |
25 |
12 |
14 |
14 |
65 |
7% |
|
15-24 |
67 |
23 |
31 |
35 |
156 |
16% |
|
25-34 |
117 |
58 |
60 |
58 |
293 |
30% |
|
35-44 |
52 |
41 |
33 |
32 |
158 |
16% |
|
45-54 |
30 |
18 |
19 |
29 |
96 |
10% |
|
55-64 |
8 |
8 |
6 |
15 |
37 |
4% |
|
65+ |
8 |
0 |
3 |
9 |
20 |
2% |
|
Unknown |
5 |
4 |
10 |
5 |
24 |
2% |
|
Gender |
||||||
|
Males |
253 |
139 |
135 |
164 |
691 |
72% |
|
Female |
80 |
57 |
71 |
65 |
273 |
28% |
|
Travel history |
||||||
|
To endemic areas and provinces |
320 |
186 |
199 |
225 |
930 |
96.47% |
|
No travel history |
9 |
7 |
3 |
1 |
20 |
2.07% |
|
Unknown travel history |
4 |
3 |
4 |
3 |
14 |
1.45% |
|
Total |
333 |
196 |
206 |
229 |
964 |
100% |
Table 1: Demographic characteristics of reported cases, Tshwane District: 2011-2014.
There were 20 deaths (2.1%) out of 964 cases. Of these, 17 secondary death audits were reviewed, 94.1% (n=16) of deaths had travelled to malaria endemic countries and provinces. Over a third of the deceased patients had comorbidities, including HIV infection (n=2), pre-eclampsia (n=1), hypertension (n=2), diabetes mellitus (n=1), asthma (n=1) and 5.9% (n=1) was pregnant. They all died in a health facility. The majority of the deceased patients (n=11) were diagnosed within a day, (range: 10 minutes to 4 days). Of all deaths, 35.3% (n=6) had co-morbidities and 4.8% (n=1) were pregnant. The length of stay in the hospital before death varied from one to 25 days (median: 4 days). The majority of the cases 47.1% (8/17) presented at a facility between three days and one week after onset of symptoms. The total number of malaria cases decreased from 333 in 2011, to 196 in 2012 and then increase slightly to 206 in 2013 to 229 in 2014 (Figure 2). A total of 19 Odyssean malaria cases have been reported. The majority (90.0%, n=18) of cases that died had travelled to malaria endemic areas. There was a decrease in the total number of deaths during the study period with the highest case fatality rate in 2012 (Figure 2). The number of malaria cases peaked in January each year for the period of study (2011-2014) (Figure 3).
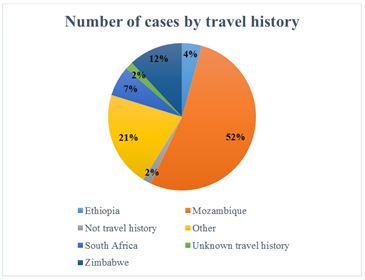
Figure 1: Number of cases by travel history, Tshwane District: 2011-2014 (n=964).
*Other refers to countries with fewer cases
In univariate analysis, cases aged 45-64 years (OR 2.9, 95%CI: 1.10 to 8.09, p=0.046) were more likely to die from malaria relative to cases of younger age groups of 0-5 years (Table 2). Gender (OR 0.6, 95%CI: 0.24 to 1.45, p=0.257) and malaria season (OR=0.7, 95% CI: 0.21 to 2.49, p=0.613) were not statistically significant (Table 2). Age, gender and malaria season were not statistically significant in multivariable analysis. History of travel to a malaria endemic area was found to be protective (OR 0.2, 95%CI: 0.36 to 0.78, p=0.02) (Table 2).
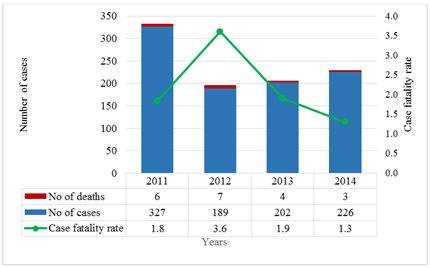
Figure 2: Changes in the occurrence of malaria cases and deaths reported in Tshwane District by year (2011-2014).
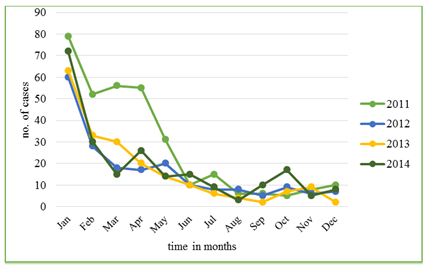
Figure 3: Trends in malaria cases reported in the Tshwane District month by month (2011-2014).
|
Variables |
Univariate analysis |
Multivariable analysis |
||||||
|
Odds ratio |
95% Confidence interval |
p-value |
Odds ratio |
95% Confidence interval |
p-value |
|||
|
Lower |
Upper |
Lower |
Upper |
|||||
|
Gender: Males |
(reference) |
|||||||
|
Females |
0.6 |
0.24 |
1.45 |
0.257 |
0.9 |
0.32 |
2.73 |
0.898 |
|
Age groups 0-5 |
(reference) |
|||||||
|
6-24 |
0.9 |
0.35 |
2.78 |
0.973 |
2.0 |
0.38 |
10.66 |
0.407 |
|
25-44 |
0.7 |
0.22 |
2.03 |
0.454 |
1.3 |
0.21 |
7.60 |
0.809 |
|
45-64 |
2.9 |
1.10 |
8.09 |
0.046 |
4.9 |
0.96 |
24.97 |
0.055 |
|
65+ |
2.7 |
0.34 |
21.19 |
0.411 |
6.3 |
0.54 |
73.38 |
0.143 |
|
Travel history: No |
(reference) |
|||||||
|
Yes |
0.2 |
0.04 |
0.78 |
0.036 |
0.1 |
0.03 |
0.75 |
0.021 |
|
Malaria season: Low |
(reference) |
|||||||
|
High |
0.7 |
0.21 |
2.49 |
0.207 |
0.9 |
0.17 |
3.64 |
0.766 |
Table 2: Logistic regression predicting the likelihood of malaria mortality in Tshwane District (2011-2014).
4. Discussion
The surveillance data indicates that malaria incidence has been decreasing from 2011 to 2014 with a decrease in the total number of deaths. Age was found to be a risk factor for mortality. Mortality was higher in older people (45-65 years). Most deaths were not in the <5 age group. This is in contrast with other studies where majority of deaths occur in children under five years of age [13]. The incidence of malaria was high in the age group 24-34 as compared to other age groups. This supports findings of other studies [11]. This is an economically productive age group. They are more likely to migrate to Tshwane district in Gauteng province for employment opportunities. Majority of cases occurred in rainy season with a highest peak in January. This may be due to people who are travelling during December holidays to locations that are malaria endemic resulting in an increased number of cases when they return from those areas. There was an increased number of cases in 2014 between August and November which may be due to high temperatures as a result of global warming. Previous studies have shown that there has been a steady decline in the number of cases in South Africa which resulted in decreased morbidity and mortality [9, 14]. Males were more affected than females. This is similar to previous studies conducted in Mpumalanga and Limpopo provinces, South Africa and United Kingdom [8, 15, 16]. All the patients did not take chemoprophylaxis as indicated on the notification forms. However, the reasons for low prophylaxis uptake were not investigated in this study. The findings of a study conducted in the United Kingdom found that low prophylaxis uptake was associated with cost and fear of side effects [17]. Research shows that pregnancy and co-morbidities may lead to severe malaria and are significant causes of malaria mortality [18-20]. However, in this study, statistical significance could not be established due to insufficient risk factor data among those who did not die. These results are similar to the results of the study conducted in Tamale hospital, Northern Ghana [21].
Travel history to a malaria endemic area was found to be protective. The study indicated that those who did not travel to malaria endemic provinces were more at risk of dying as compared to those who travelled. The reason for this might be that malaria is unlikely to be suspected in those without a travel history and diagnosis might be missed. The study showed that the odds of dying from malaria increases with age. This is similar to the results of the study conducted in United Kingdom in 2012 [22]. This study had some limitations. Our study focused on cases which were reported to the Communicable Disease Control office in Tshwane District. Those who were not reported would have caused underrepresentation of the total number of cases in Tshwane District. The results are not generalizable because the surveillance system looked at was only that from Tshwane. A risk factor audit was done only for the patients who died, hence there was insufficient risk factor data for those patients who did not die. The outcome of this study was malaria mortality and the sample size of the deceased was small hence the statistical significance of other variables could not be established. The other limitation of this study is that we were not able to analyse some potential risk factors such as occupation, pregnancy, chemoprophylaxis during travel, time interval between illness and presentation at the health facility, comorbidity, length of stay in hospital, doctors training about malaria, availability of malaria guidelines due to insufficient risk factor information for those patients who did not die.
5. Conclusion
In Tshwane district, malaria cases were reported throughout the year during the study period with seasonal peaks. Majority of cases were imported. Therefore, public awareness regarding uptake of antimalarial prophylaxis before and during travel to endemic areas could lead to a reduction in mortality and morbidity in South Africa. There is a need to investigate any case of fever for malaria infection to avoid complications and to reduce morbidity and mortality. Malaria surveillance should be strengthened in non-endemic provinces for early detection of malaria cases, including Odyssean cases to reduce morbidity and mortality associated with malaria.
6. Acknowledgements
We would like to thank Tshwane District Communicable Disease Control Directorate for providing and allowing access to the surveillance data Thanks to South African Field Epidemiology Program for their continued support. We are grateful to Dorothy L. Southern for her input and guidance on scientific writing and for the critical review of this manuscript.
References
- World malaria report 2013, World Health Organization (2014).
- Dube S, Ismail N, Hoosen A. A retrospective review of malaria cases seen in a non-endemic area of South Africa. Travel medicine and infectious disease 6 (2008): 296-300.
- World Health Organization. World malaria report (2012).
- Morris N, Frean J, Baker L, et al. Re-defining the extent of malaria transmission in South Africa: Implications for chemoprophylaxis. SAMJ: South African Medical Journal 103 (2013): 858-860.
- Salvadó E, Pinazo MJ, Munoz J, et al. Clinical presentation and complications of Plasmodium falciparum malaria in two populations: travelers and immigrants. Enfermedades infecciosas y microbiologia clinica 26 (2008): 282-284.
- Maharaj R, Raman J, Morris N, et al. Epidemiology of malaria in South Africa: From control to elimination. SAMJ: South African Medical Journal 103 (2013): 779-783.
- Tilley L, Dixon MW, Kirk K. The Plasmodium falciparum-infected red blood cell. The international journal of biochemistry & cell biology 43 (2011): 839-842.
- Phillips A, Bassett P, Szeki S, Newman S, Pasvol G. Risk factors for severe disease in adults with falciparum malaria. Clinical Infectious Diseases 48 (2009): 871-878.
- Moonasar D, Nuthulaganti T, Kruger PS, et al. Malaria control in South Africa 2000-2010: beyond MDG6. Malar J 11 (2012): 1475-2875.
- Frean J, Brooke B, Thomas J, et al. Odyssean malaria outbreaks in Gauteng province, South Africa, 2007-2013. South African Medical Journal 104 (2014).
- Khosa E, Kuonza LR, Kruger P, et al. Towards the elimination of malaria in South Africa: a review of surveillance data in Mutale Municipality, Limpopo Province, 2005 to 2010. Malar J 12 (2013).
- Metropolitan Municipality. Statistics South Africa (2015).
- Coulibaly D, Rebaudet S, Travassos M, et al. Spatio-temporal analysis of malaria within a transmission season in Bandiagara, Mali. Malaria journal 12 (2013): 82.
- Baker L. A practical guide to the management of malaria in South Africa-2010: review. SA Pharmaceutical Journal 77 (2010): 28-32.
- Ngomane L, De Jager C. Changes in malaria morbidity and mortality in Mpumalanga Province, South Africa (2001-2009): a retrospective study. Malar J 11 (2012): 19.
- Gerritsen A, Kruger P, van der Loeff M, Grobusch MP. Malaria incidence in Limpopo Province, South Africa, 1998-2007. Malar J 7 (2008): 162.
- Smith AD, Bradley DJ, Smith V, et al. Imported malaria and high risk groups: observational study using UK surveillance data 1987-2006. Bmj (2008): 337.
- Desai M, ter Kuile FO, Nosten F, et al. Epidemiology and burden of malaria in pregnancy. The Lancet infectious diseases 7 (2007): 93-104.
- Rogerson SJ, Hviid L, Duffy PE, et al. Malaria in pregnancy: pathogenesis and immunity. The Lancet infectious diseases 7 (2007): 105-117.
- Bejon P, Berkley JA, Mwangi T, et al. Defining childhood severe falciparum malaria for intervention studies. PLoS medicine 4 (2007): 251.
- Abdul-Aziz A, Harris E, Munyakazi L. Risk Factors In Malaria Mortality Among Children In Northern Ghana: A Case Study At The Tamale Teaching Hospital. International Journal of Business and Social Research 2 (2012): 35-45.
- Checkley AM, Smith A, Smith V, et al. Risk factors for mortality from imported falciparum malaria in the United Kingdom over 20 years: an observational study. Bmj (2012): 344.
|
Citation: Mphaka MR, Moshime M, Tsilo LC, Reddy C. Risk Factors Associated With Malaria Mortality in Tshwane District, South Africa: A Retrospective Cohort Study, 2011-2014. Journal of Environmental Science and Public Health 3 (2019): 289-297. |
