Regional Variability of Admission Prevalence and Mortality of Pediatric Critical Illness in Latvia
Article Information
Linda Setlere1,2, Ivars Vegeris2,3, Margita Stale4, Reinis Balmaks1,2
1Faculty of Medicine, Riga Stradins University, Latvia
2Intensive Care Unit, Children’s Clinical University Hospital, Riga, Latvia
3Department of Doctoral Studies, Riga Stradins University, Latvia
4The Centre for Disease Prevention and Control of Latvia, Riga
*Corresponding Author: Dr. Reinis Balmaks, Departments of Clinical Skills and Medical Technologies and Pediatrics, Riga Stradins University, 26a Anninmuizas Blvd, Riga, LV-1067, Latvia
Received: 03 May 2019; Accepted: 09 May 2019; Published: 17 May 2019
Citation: Linda Setlere, Ivars Vegeris, Margita Stale, Reinis Balmaks. Regional Variability of Admission Prevalence and Mortality of Pediatric Critical Illness in Latvia. Anesthesia and Critical Care 1 (2019): 15-22.
View / Download Pdf Share at FacebookAbstract
Objectives: There is only one pediatric intensive care unit (PICU) in Latvia, where all critically ill children <18 years are admitted from all regions of Latvia. The aim of this study is to ascertain regional differences in mortality and morbidity of critically ill children over a 5-year period.
Materials and Methods: Descriptive retrospective study of children who were admitted to the PICU in Latvia from January 2012 to December 2016. Data on episodes were obtained from the Children's Clinical University Hospital electronic health records. Pediatric Index of Mortality (PIM2) was used for risk adjustment and calculation of standardized mortality ratio (SMR). The data were compared among the six regions of Latvia - Kurzeme, Latgale, Pieriga, Riga, Vidzeme, and Zemgale.
Results: The analysis included 3651 intensive care episodes. The highest PICU admission prevalence was in Riga and the lowest in Latgale - 2.3 and 1.7 admissions per 1000 children per year, respectively. The highest emergency admission proportion was observed in Riga and Pieriga, while the lowest in Latgale - 52 and 38%, respectively. The average proportion of mechanically ventilated patients ranged from 24 to 29% of all admitted patients across the regions. SMR for the total population was 1.44 (95% CI: 1.17- 1.81). In two regions, Riga (1.51; 95% CI: 1.04- 2.14) and Latgale (2.21; 95% CI: 1.9- 3.76), it was significantly higher than 1.
Conclusions: We noted excess mortality (SMR >1) in the population of critically ill children in Latvia, 2012-2016; in particular, in patients from two regions - Riga and Latgale.
Keywords
Pediatric intensive care units, Critical care outcomes; Child mortality, Hospital mortality, Critical illness, Patient admission
Pediatric intensive care units articles Pediatric intensive care units Research articles Pediatric intensive care units review articles Pediatric intensive care units PubMed articles Pediatric intensive care units PubMed Central articles Pediatric intensive care units 2023 articles Pediatric intensive care units 2024 articles Pediatric intensive care units Scopus articles Pediatric intensive care units impact factor journals Pediatric intensive care units Scopus journals Pediatric intensive care units PubMed journals Pediatric intensive care units medical journals Pediatric intensive care units free journals Pediatric intensive care units best journals Pediatric intensive care units top journals Pediatric intensive care units free medical journals Pediatric intensive care units famous journals Pediatric intensive care units Google Scholar indexed journals Critical care outcomes articles Critical care outcomes Research articles Critical care outcomes review articles Critical care outcomes PubMed articles Critical care outcomes PubMed Central articles Critical care outcomes 2023 articles Critical care outcomes 2024 articles Critical care outcomes Scopus articles Critical care outcomes impact factor journals Critical care outcomes Scopus journals Critical care outcomes PubMed journals Critical care outcomes medical journals Critical care outcomes free journals Critical care outcomes best journals Critical care outcomes top journals Critical care outcomes free medical journals Critical care outcomes famous journals Critical care outcomes Google Scholar indexed journals Child mortality articles Child mortality Research articles Child mortality review articles Child mortality PubMed articles Child mortality PubMed Central articles Child mortality 2023 articles Child mortality 2024 articles Child mortality Scopus articles Child mortality impact factor journals Child mortality Scopus journals Child mortality PubMed journals Child mortality medical journals Child mortality free journals Child mortality best journals Child mortality top journals Child mortality free medical journals Child mortality famous journals Child mortality Google Scholar indexed journals Hospital mortality articles Hospital mortality Research articles Hospital mortality review articles Hospital mortality PubMed articles Hospital mortality PubMed Central articles Hospital mortality 2023 articles Hospital mortality 2024 articles Hospital mortality Scopus articles Hospital mortality impact factor journals Hospital mortality Scopus journals Hospital mortality PubMed journals Hospital mortality medical journals Hospital mortality free journals Hospital mortality best journals Hospital mortality top journals Hospital mortality free medical journals Hospital mortality famous journals Hospital mortality Google Scholar indexed journals Critical illness articles Critical illness Research articles Critical illness review articles Critical illness PubMed articles Critical illness PubMed Central articles Critical illness 2023 articles Critical illness 2024 articles Critical illness Scopus articles Critical illness impact factor journals Critical illness Scopus journals Critical illness PubMed journals Critical illness medical journals Critical illness free journals Critical illness best journals Critical illness top journals Critical illness free medical journals Critical illness famous journals Critical illness Google Scholar indexed journals Patient admission articles Patient admission Research articles Patient admission review articles Patient admission PubMed articles Patient admission PubMed Central articles Patient admission 2023 articles Patient admission 2024 articles Patient admission Scopus articles Patient admission impact factor journals Patient admission Scopus journals Patient admission PubMed journals Patient admission medical journals Patient admission free journals Patient admission best journals Patient admission top journals Patient admission free medical journals Patient admission famous journals Patient admission Google Scholar indexed journals Pediatric Index of Mortality articles Pediatric Index of Mortality Research articles Pediatric Index of Mortality review articles Pediatric Index of Mortality PubMed articles Pediatric Index of Mortality PubMed Central articles Pediatric Index of Mortality 2023 articles Pediatric Index of Mortality 2024 articles Pediatric Index of Mortality Scopus articles Pediatric Index of Mortality impact factor journals Pediatric Index of Mortality Scopus journals Pediatric Index of Mortality PubMed journals Pediatric Index of Mortality medical journals Pediatric Index of Mortality free journals Pediatric Index of Mortality best journals Pediatric Index of Mortality top journals Pediatric Index of Mortality free medical journals Pediatric Index of Mortality famous journals Pediatric Index of Mortality Google Scholar indexed journals standardized mortality ratio articles standardized mortality ratio Research articles standardized mortality ratio review articles standardized mortality ratio PubMed articles standardized mortality ratio PubMed Central articles standardized mortality ratio 2023 articles standardized mortality ratio 2024 articles standardized mortality ratio Scopus articles standardized mortality ratio impact factor journals standardized mortality ratio Scopus journals standardized mortality ratio PubMed journals standardized mortality ratio medical journals standardized mortality ratio free journals standardized mortality ratio best journals standardized mortality ratio top journals standardized mortality ratio free medical journals standardized mortality ratio famous journals standardized mortality ratio Google Scholar indexed journals
Article Details
1. Introduction
Latvia is a Northern European country with a population size of 1.97 million, of which about 354,000 are children less than 18 [1]. Over the last 25 years, the under-five mortality rate in Latvia has decreased from 21 to 4.8 per 1,000 live births; however, it still remains one of the highest in the European Union [2, 3]. Latvia’s National Health Service healthcare system has a hospital network consisting of three tertiary university hospitals, seven regional hospitals where multidisciplinary subspecialty care is available, twelve local hospitals and ten specialized hospitals providing only single subspecialty care (e.g. orthopedics, obstetrics, psychiatry etc.) [4]. Of the three university hospitals, one is a dedicated children’s hospital where all children needing pediatric subspecialist care are transferred, including critical care. The only national PICU admits all critically ill children that are older than 1 month and younger than 18 years from all regions of Latvia (>700 children a year) [5]. In Latvia any child who requires continuous cardiopulmonary monitoring is considered a candidate for PICU admission.
The territory of Latvia is divided into 6 regions, consisting of counties and cities. Following the completion of administrative territorial reform in 2009, Latvia has Riga (the capital city), Pieriga (central Latvia surrounding the capital), Vidzeme (North-East), Latgale (South-East), Zemgale (South), and Kurzeme (West) regions (Figure 1A). The aim of this study was to investigate regional differences in the admission prevalence, mortality and interventions for pediatric critical illness in Latvia over a five-year period.
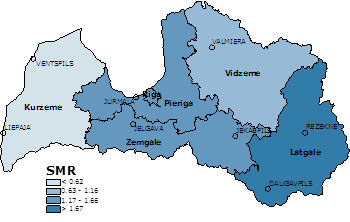
Figure 1A: Calculated SMR and the geographic location of the regions of Latvia.
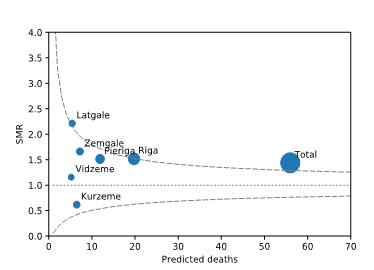
Figure 1B: SMR according to predicted number of deaths in the regions of Latvia. Dashed lines represent 95% CI for SMR of 1.0. SMR - standardized mortality ratio; CI - confidence interval.
2. Materials and Methods
2.1 Patients
This was a descriptive retrospective study. The study protocol was approved by Riga Stradins University Ethics Committee (No 24 / 27.04.2017.) and Children’s Clinical University Hospital (BKUS-3/2017). All children between the ages of 1 month and 18 years who were admitted to Children’s Clinical University Hospital Intensive Care Unit between January 2012 and December 2016 were included in this study. In Latvia children younger than 1 month regardless of diagnosis are admitted to the neonatal intensive care unit and were excluded.
2.2 Clinical data
Data on episodes of intensive care were obtained from the Children's Clinical University Hospital electronic health records system Andromeda (Children's Clinical University Hospital, Riga, Latvia). Clinical data were obtained from the IntelliVue Clinical Information Portfolio (ICIP) D.03.02 (Koninklijke Phillips Electronics N.V., The Netherlands) electronic medical record software.
2.3 Population data
The population data were obtained from The Centre for Disease Prevention and Control of Latvia. Population data at the beginning of 2016 were used as denominator (Table 1).
Table 1: Demographics and characteristics of pediatric critical illness among the regions of Latvia.
2.4 Risk adjustment
Pediatric Index of Mortality (PIM2) score was used for risk adjustment and standardized mortality ratio calculation [6]. PIM2 is a mortality risk prediction tool which considers data on the type of admission (elective or emergency), low-risk or high-risk diagnosis, mechanical ventilation, blood pressure, blood gas, and pupillary examination data within the first hour of admission to the PICU. SMR is a recognized indicator of critical care quality. SMR was calculated as a ratio of the observed PICU mortality and mortality predicted by PIM2. An SMR >1 means that observed mortality is higher than expected [7]. 95% confidence intervals (CI) were calculated by using Mid-P test in SMR Analysis v4.11.19 on-line tool [8].
2.5 Data visualization
ArcGIS 10.5.1 (Esri, US) software was used for data visualization on maps.
3. Results
Hospital electronic health records returned 3709 admissions to intensive care, 40 (1%) were excluded because of missing, incomplete or conflicting clinical data, 18 (0.5%) patients could not be assigned to a region, i.e. missing address or not residents of Latvia. The final analysis included 3651 intensive care episodes of 2903 individual patients, a mean of 730 episodes per year.
3.1 PICU admission prevalence
During the study period the average PICU admission prevalence was 206 per 100,000 children per year (95% CI: 198-211). Table 1 demonstrates regional differences in the admission prevalence. The highest admission prevalence of critical pediatric illness was observed in Riga, while the lowest was in Latgale, with 231 and 173 admissions per 100,000 children per year, respectively. Latgale also had the lowest emergency admission proportion-37.8% of all admitted patients. The highest proportion of emergency admissions was observed in Riga and Pieriga-52%(Table 1).
3.2 Diagnostic groups
Figure 2 demonstrates the most common diagnostic groups. The five most common reasons for admission were cardiovascular, gastrointestinal, neurological, musculoskeletal diagnosis and trauma. The main reason for admission to PICU in Riga, Pieriga, Vidzeme, Zemgale and Latgale regions was cardiovascular diagnosis. In Kurzeme the most common reason for admission was trauma (16%). Trauma had similar prevalence across all regions of Latvia (11 to 15%).
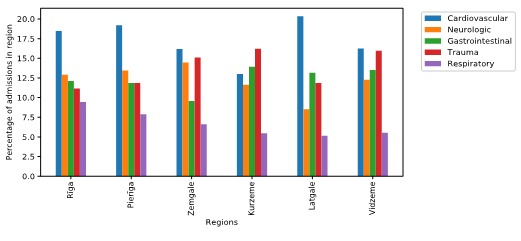
Figure 2: Five most frequent types of diagnosis in the regions of Latvia (2012- 2016).
3.3 Mechanical ventilation
A total of 958 (26.2%) patients were ventilated during study period. No significant differences were observed in the proportion of mechanically ventilated patients in regions of Latvia. The average proportion of mechanically ventilated patients ranged from 24 to 29% of all admitted patients with median ventilation period of 2 (IQR: 1- 4) days.
3.4 Mortality
A total of 829 children aged 1 month to <18 years died in Latvia during the study period. Of all deaths during the study period 82 (9.9%) were PICU deaths. The proportion PICU deaths varied from 3.2 in Kurzeme to 14.3% in Riga. Table 2 shows observed PICU mortality rate, predicted PICU mortality, mean PIM2 score and SMR across all regions. SMRs in the whole PICU population (1.47; 95% CI: 1.17- 1.81) and in Riga (1.51; 95% CI: 1.04- 2.14) and Latgale (2.21; 95% CI: 1.9- 3.76) regions were significantly higher than 1 (Figure 1B).
|
Parameter |
Regions |
Total |
|||||
|
Riga |
Pieriga |
Kurzeme |
Vidzeme |
Zemgale |
Latgale |
||
|
Observed mortality rate |
0.0235 |
0.024 |
0.0091 |
0.0183 |
0.0256 |
0.031 |
0.022 |
|
Prediction by mean PIM2a score |
0.0155 |
0.0158 |
0.0148 |
0.0159 |
0.0154 |
0.0139 |
0.0153 |
|
SMRb (95% CI) |
1.52 (1.04-2.14) |
1.51 (0.92-2.34) |
0.62 (0.2-1.49) |
1.16 (0.47-2.4) |
1.66 (0.9-2.82) |
2.21 (1.2-3.76) |
1.47 (1.17-1.81) |
a - Pediatric Index of Mortality 2; b - Standardized mortality ratio
Table 2: Regional standardized mortality ratios of critically ill children in Latvia (2012–2016).
4. Discussion
Pediatric intensive care is a low-volume, high cost specialty with a primary goal of lowering mortality of children with reversible critical illness whilst optimizing functional outcomes [9]. Description of the epidemiology of critical illness allows for planning of bed numbers and staffing, thus meeting the demand for this expensive resource cost-effectively and safely. Furthermore, regional factors are crucial in planning specialized transfer of these children in a timely manner. This is the first study that assessed differences in incidence and mortality of pediatric critical illness across the regions of Latvia.
Average admission prevalence of pediatric critical illness in Latvia during January 2012 to December 2016 was 206 per 100,000 children (<18 years) per year. The rate of PICU admissions in the United Kingdom (UK) and Ireland was similar with 150 per 100,000 children <16 per year [10]. Our observed crude PICU mortality was low (average mortality rate 2.2%) and was lower than reported elsewhere - 3.4% in the PICANet registry in the UK and Ireland [10], 5.8% in a Europe-wide study [11], 6.4- 10.3% in the PICUs in Egypt [12]. A five-year retrospective cohort study by McCrory and colleagues showed a very similar crude PICU mortality in the United States of 2.3% [13]. However, mortality in the intensive care unit depends on the severity of illness and the patient population analyzed. Risk adjustment scores allow for inter- and intra- unit mortality comparison over time [14]. For this reason, we used the PIM2 score and standardized mortality ratio (SMR). There was excess mortality in the whole population and in two regions in particular - Riga and Latgale.
Another important finding of this study is that only a small proportion of children died in the PICU in Latvia (9.9%). This proportion is lower than in the UK, where about 15% children die in the PICU [10]. Moreover, in 2016 of all pediatric deaths (28 days to 14 years) in Latvia, 56% were out-of-hospital, with most out-of-hospital deaths caused by accidents (The Centre for Disease Prevention and Control of Latvia; data given upon request); in comparison in the UK in the same age group only 20% deaths were out-of-hospital [15]. The delay in reaching hospital care may be a significant factor why we observed excess mortality in this study. Mechanical ventilation is one of the most common procedures performed in PICU. According to Khemani and colleagues in the United States 30% to 64% of admitted patients require ventilatory support [16], in the UK and Ireland about 65% [10], while in a study in India about 16% of patients received mechanical ventilation [17]. In our study the proportion of mechanically ventilated patients was only from 24% to 29%. This can be explained by the fact that in Children’s Clinical University Hospital there are no high-dependency or step-down units, hence most patients requiring telemetry are admitted to the PICU.
5. Limitations
This was a retrospective study. The main limitation of this fact is that we could not retrieve all information necessary for calculation of PIM2 in all patients. Missing variables in this risk prediction model are assumed to be normal and lead to lower estimated mortality risk. This study led to the establishment of prospective PICU registry in Latvia [5], which will allow prospective validation of these findings. Some children >1 month died in the NICU, which leads to lower proportion of PICU deaths, even though these children were receiving intensive care. We were unable to adjust for this; however, we know that this number is small.
6. Conclusions
While the childhood mortality in Latvia is declining, still it remains one of the highest in the European Union. We evaluated the main indicators of the PICU epidemiology and compared them among different regions of Latvia. We found higher than predicted PICU mortality in Latvia. This study raises the question and need to investigate why regional differences in pediatric critical care in Latvia exist.
Acknowledgments
The authors would like to thank medical student Viktoria Schaeff and Drs. Anete Paula Perova, Valdis Skotelis and Janis Kolbergs for help with the data collection and Dr. Roger Parslow for statistical advice and critical reading of the manuscript.
Conflicts of Interest and Source of Funding
None declared.
References
- Central Statistical Bureau of Latvia. Children in Latvia 2016, collection of statistics, Riga (2017).
- Under-5 Mortality Rate - Total. UN Inter-agency Group for Child Mortality Estimation (2019).
- Wang H, Liddell CA, Coates MM, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384 (2014): 957-979.
- The National Health Service. Hospitalization Plan (2019).
- Vegeris I, Daukste I, Barzdina A, et al. Abstract P-372: Establishment of pediatric intensive care registry in Latvia. Pediatric Critical Care Medicine 19 (2018): 161.
- Slater A, Shann F, Pearson G. Paediatric Index of Mortality (PIM) Study Group. PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Medicine 29 (2003): 278-285.
- Siegel T, Adamski J, Nowakowski P, et al. Prospective assessment of the standardized mortality ratio (SMR) as a measure of quality of care in an intensive care unit - a single-centre study. Anesthesiology Intensive Therapy 47 (2015): 328-332.
- Sullivan KM. Standardized Mortality Ratio (SMR) (2019).
- Goh AY, Mok Q. Centralization of paediatric intensive care: are critically ill children appropriately referred to a regional centre? Intensive Care Medicine 27 (2001): 730-735.
- Paediatric Intensive Care Audit Network Annual Report 2017. Universities of Leeds and Leicester (2017).
- Devictor DJ, Nguyen DT. Forgoing life-sustaining treatments in children: a comparison between Northern and Southern European pediatric intensive care units. Pediatric Critical Care Medicine 5 (2004): 211-215.
- Rady HI, Mohamed SA, Mohssen NA, et al. Application of different scoring systems and their value in pediatric intensive care unit. Egyptian Pediatric Association Gazette 62 (2014):59-64.
- McCrory MC, Spaeder MC, Gower EW, et al. Time of Admission to the PICU and Mortality. Pediatric Critical Care Medicine 18 (2017): 915-923.
- Sankar J, Singh A, Sankar MJ, et al. Pediatric Index of Mortality and PIM2 scores have good calibration in a large cohort of children from a developing country. Biomed Research International (2014): 907871.
- Office for National Statistics. Statistical bulletin. Deaths registered in England and Wales: 2016. Newport, (2017).
- Khemani RG, Markovitz BP, Curley MAQ. Characteristics of children intubated and mechanically ventilated in 16 PICUs. Chest 136 (2009): 765-771.
- Bhori NS, Ghate SV, Chhajed PS. A study of mechanical ventilation in children. International Journal Contemporary Pediatrics 4 (2017): 2088-2092.
