Prognostic Indicators in Hepatocellular Carcinoma (HCC) in a Moroccan Population
Article Information
Nada Lahmidani*, Fatime Zahra Hamdoun, Hakima Abid, Maria.Lahlali, Mohammed El Abkari, Sidi Adil Ibrahimi
Department of Gastroenterology, University Hospital Hassan II, School of Medicine and Pharmacy of Fez, Sidi Mohammed Ben Abdallah University, Fez, Morocco
*Corresponding Author: Prof. Nada Lahmidani, Department of Gastroenterology, University Hospital Hassan II, School of Medicine and Pharmacy of Fez, Sidi Mohammed Ben Abdallah University, Fez, Morocco
Received: 02 April 2020; Accepted: 17 April 2020; Published: 27 April 2020
Citation: Nada Lahmidani, Fatime Zahra Hamdoun, Hakima Abid, Maria.Lahlali, Mohammed El Abkari, Sidi Adil Ibrahimi. Prognostic Indicators in Hepatocellular Carcinoma (HCC) in a Moroccan Population. Journal of Cancer Science and Clinical Therapeutics 4 (2020): 115-119.
View / Download Pdf Share at FacebookAbstract
Prognostic Indicators in Hepatocellular Carcinoma (HCC) in a Moroccan Population
Keywords
Hepatocellular carcinoma; Prognostic indicators; Poor prognosis
Hepatocellular carcinoma articles, Prognostic indicators articles, Poor prognosis articles
Hepatocellular carcinoma articles Hepatocellular carcinoma Research articles Hepatocellular carcinoma review articles Hepatocellular carcinoma PubMed articles Hepatocellular carcinoma PubMed Central articles Hepatocellular carcinoma 2023 articles Hepatocellular carcinoma 2024 articles Hepatocellular carcinoma Scopus articles Hepatocellular carcinoma impact factor journals Hepatocellular carcinoma Scopus journals Hepatocellular carcinoma PubMed journals Hepatocellular carcinoma medical journals Hepatocellular carcinoma free journals Hepatocellular carcinoma best journals Hepatocellular carcinoma top journals Hepatocellular carcinoma free medical journals Hepatocellular carcinoma famous journals Hepatocellular carcinoma Google Scholar indexed journals Prognostic indicators articles Prognostic indicators Research articles Prognostic indicators review articles Prognostic indicators PubMed articles Prognostic indicators PubMed Central articles Prognostic indicators 2023 articles Prognostic indicators 2024 articles Prognostic indicators Scopus articles Prognostic indicators impact factor journals Prognostic indicators Scopus journals Prognostic indicators PubMed journals Prognostic indicators medical journals Prognostic indicators free journals Prognostic indicators best journals Prognostic indicators top journals Prognostic indicators free medical journals Prognostic indicators famous journals Prognostic indicators Google Scholar indexed journals Poor prognosis articles Poor prognosis Research articles Poor prognosis review articles Poor prognosis PubMed articles Poor prognosis PubMed Central articles Poor prognosis 2023 articles Poor prognosis 2024 articles Poor prognosis Scopus articles Poor prognosis impact factor journals Poor prognosis Scopus journals Poor prognosis PubMed journals Poor prognosis medical journals Poor prognosis free journals Poor prognosis best journals Poor prognosis top journals Poor prognosis free medical journals Poor prognosis famous journals Poor prognosis Google Scholar indexed journals liver tumor articles liver tumor Research articles liver tumor review articles liver tumor PubMed articles liver tumor PubMed Central articles liver tumor 2023 articles liver tumor 2024 articles liver tumor Scopus articles liver tumor impact factor journals liver tumor Scopus journals liver tumor PubMed journals liver tumor medical journals liver tumor free journals liver tumor best journals liver tumor top journals liver tumor free medical journals liver tumor famous journals liver tumor Google Scholar indexed journals cirrhosis articles cirrhosis Research articles cirrhosis review articles cirrhosis PubMed articles cirrhosis PubMed Central articles cirrhosis 2023 articles cirrhosis 2024 articles cirrhosis Scopus articles cirrhosis impact factor journals cirrhosis Scopus journals cirrhosis PubMed journals cirrhosis medical journals cirrhosis free journals cirrhosis best journals cirrhosis top journals cirrhosis free medical journals cirrhosis famous journals cirrhosis Google Scholar indexed journals cirrhotic patients articles cirrhotic patients Research articles cirrhotic patients review articles cirrhotic patients PubMed articles cirrhotic patients PubMed Central articles cirrhotic patients 2023 articles cirrhotic patients 2024 articles cirrhotic patients Scopus articles cirrhotic patients impact factor journals cirrhotic patients Scopus journals cirrhotic patients PubMed journals cirrhotic patients medical journals cirrhotic patients free journals cirrhotic patients best journals cirrhotic patients top journals cirrhotic patients free medical journals cirrhotic patients famous journals cirrhotic patients Google Scholar indexed journals hepatocellular carcinoma articles hepatocellular carcinoma Research articles hepatocellular carcinoma review articles hepatocellular carcinoma PubMed articles hepatocellular carcinoma PubMed Central articles hepatocellular carcinoma 2023 articles hepatocellular carcinoma 2024 articles hepatocellular carcinoma Scopus articles hepatocellular carcinoma impact factor journals hepatocellular carcinoma Scopus journals hepatocellular carcinoma PubMed journals hepatocellular carcinoma medical journals hepatocellular carcinoma free journals hepatocellular carcinoma best journals hepatocellular carcinoma top journals hepatocellular carcinoma free medical journals hepatocellular carcinoma famous journals hepatocellular carcinoma Google Scholar indexed journals hypervascularized nodule articles hypervascularized nodule Research articles hypervascularized nodule review articles hypervascularized nodule PubMed articles hypervascularized nodule PubMed Central articles hypervascularized nodule 2023 articles hypervascularized nodule 2024 articles hypervascularized nodule Scopus articles hypervascularized nodule impact factor journals hypervascularized nodule Scopus journals hypervascularized nodule PubMed journals hypervascularized nodule medical journals hypervascularized nodule free journals hypervascularized nodule best journals hypervascularized nodule top journals hypervascularized nodule free medical journals hypervascularized nodule famous journals hypervascularized nodule Google Scholar indexed journals hepatic parenchyma articles hepatic parenchyma Research articles hepatic parenchyma review articles hepatic parenchyma PubMed articles hepatic parenchyma PubMed Central articles hepatic parenchyma 2023 articles hepatic parenchyma 2024 articles hepatic parenchyma Scopus articles hepatic parenchyma impact factor journals hepatic parenchyma Scopus journals hepatic parenchyma PubMed journals hepatic parenchyma medical journals hepatic parenchyma free journals hepatic parenchyma best journals hepatic parenchyma top journals hepatic parenchyma free medical journals hepatic parenchyma famous journals hepatic parenchyma Google Scholar indexed journals parenchyma tumor articles parenchyma tumor Research articles parenchyma tumor review articles parenchyma tumor PubMed articles parenchyma tumor PubMed Central articles parenchyma tumor 2023 articles parenchyma tumor 2024 articles parenchyma tumor Scopus articles parenchyma tumor impact factor journals parenchyma tumor Scopus journals parenchyma tumor PubMed journals parenchyma tumor medical journals parenchyma tumor free journals parenchyma tumor best journals parenchyma tumor top journals parenchyma tumor free medical journals parenchyma tumor famous journals parenchyma tumor Google Scholar indexed journals
Article Details
1. Introduction
HCC is the most common primary liver tumor with a high mortality rate. It is an unpredictable cancer with unpredictable progression. Worldwide, it is the fifth most common type of cancer and third most common cause of cancer mortality [1]. Screening ultrasound plays an essential role in cirrhotic patients; it increases the percentage of HCC detection at an early stage and consequently opens up the possibility of curative treatment [2]. The various forms of treatment available for these tumours are effective in improving survival only when the disease is diagnosed at an early stage. For patients with larger tumours and decompensated cirrhosis, no treatment appears to be capable of prolonging survival [3]. The prognosis for HCC on cirrhosis is generally poor and seems to be determined not only by factors linked to the tumor, but also by factors linked to cirrhosis. The main objective of our study is to determine prognostic factors in cirrhotic patients with HCC.
2. Methods
This is a retrospective study of patients with hepatocellular carcinoma on cirrhosis liver diagnosed from January 2009 to July 2019. The diagnosis of HCC was made according to the non-invasive criteria of EASL (existence of a hypervascularized nodule at early arterial time (wash-in) with washing (wash-out: hypodensity or hypointensity compared to the non-tumoral hepatic parenchyma) in the portal phase or in the late phase compared to the non-tumorous parenchyma tumor) with the use of histology for doubtful cases. The degree of hepatocellular insufficiency was defined by the CHILD score. The response to treatment was evaluated at 1 month then 3 months for per cutaneous treatment, 3 months for hepatic resection and Sorafenib and according to the RECIST criteria for transarterial chemoembolization (Complete response if complete disappearance of the enhancement of the treated area, partial response if reduction >50% of the viable part of the target lesion, progression if increase >25% of the viable part of the target lesion or new lesion, stability in other cases).
3. Statistical Analysis
The results were analyzed using the Statistics Package for Social Science software (SPSS version 20) for Windows. Quantitative variables were expressed as average ± standard deviation. Qualitative variables were expressed in number and percentage (%). Multivariate analysis was performed with a binary logistic regression model to identify prognostic factors and we considered significant a p≤0.05. Survival data was analyzed by Kaplan Meier method.
4. Results
We have collected 148 cases of HCC on cirrhosis liver. The average age was 64 [18; 72] years predominance of female. The etiology of cirrhosis was secondary to the hepatitis B and C virus in 79.7%. Child's score was ≥ B7 in 35.8%. Alpha fetoprotein (AFP) exceeded >400 ng/ml in 28.3%. HCC nodules exceeded 3 cm in 66.9%. Invasion of the portal vein was objectified in 15.9% with the presence of metastases in 19%. Only 22.9% patients had curative treatment: 14.86% received per cutaneous treatment and 8.1% had liver resection. Palliative means interested 77% of patients: Transarterial chemoembolization in 39.18%, Sorafenib was used in 22.97% and 13.5% were beyond all therapeutic resources (Table 1). The evolution was marked by progression in 61%. The average overall survival at 1 year and at 5 years was 68.7% and 27% respectively. We noted a significant reduction in survival rate at 1 year: it has decreased from 86, 2% to less than 27% at 5 years which supports the prognosis for CHC (Figure1). The prognostic indicators of death were respectively advanced child (p=0.005), AFP level >400 ng/ml (p=0.02) and presence of metastasis (p <0.001) Table 2.
|
middle age |
64 [18; 72] ans |
|
Sexe ratio (F/H) |
1.24 |
|
Cirrhosis etiology VHC VHB metabolic syndrome |
53.37% (N 79) 26.35% (N 39) 20.27% (N 30) |
|
Screening |
68% (N 101) |
|
Who score 0-1 ≥2 |
85% (N 126) 14.86% (N 22) |
|
AFP score ≤10 ng/ml >10 ng/ml et ≤ 400 ng/ml >400 ng/ml |
34.45% (N 51) 37.16% (N 55) 28.3% (N 42) |
|
CHILD score Child A Child B/C |
64.18% (N 95) 35.8% (N 53) |
|
Characteristic of the tumor: Small CHC (<3 cm) Portal vein thrombosis Metastasis |
33.1% (N 49) 14.8%(N 22) 17% (N 25) |
|
Curative treatment Radiofrequency Alcohol ablation Liver resection |
6.08% (N 9) 8.78% (N 13) 8.10% (N 12) |
|
Other therapeutic means transarterial chemoembolization sorafenib Symptomatic treatment |
39.18% (N 58) 22.97% (N 34) 13.5% (N 20) |
Table 1: Characteristics of the studied population.
|
Prognostic factors |
p |
OR |
Confidence interval |
|
Child avanced |
P=0,005 |
2,87 |
[1,36; 6,05] |
|
AFP level >400 ng / ml |
p=0,02 |
2,30 |
[1,15; 4,77] |
|
Presence of metastasis |
p=0,01 |
3,35 |
[1,13; 4,04] |
|
Portal vein thrombosis |
p=0,03 |
2,7 |
[0,86; 8,83] |
Table 2: Poor prognostic factors in patients with HCC on cirrhosis liver.
Months
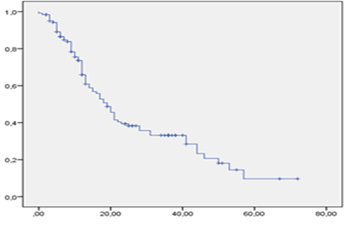
Figure 1: Survival curve for patients with HCC on cirrhosis liver.
5. Discussion
Prognostic studies in HCC are often unsatisfactory because patients included are heterogeneous. Tumor staging at the time of diagnosis is essential to decide which type of therapy is the most appropriate for patients. Several alternative staging systems have been proposed. The CLIP studies identified five independent prognostic variables: Child-Pugh class of cirrhosis, tumour size, number of lesions, presence/absence of portal vein thrombosis, and serum levels of AFP [4]. The Okuda system is a prognostic score introduced in 1985; it includes the tumor volume, the presence of ascites, and the levels of serum albumin and bilirubin [5].
The Barcelona Clinic Liver Cancer (BCLC) staging classification includes four stages: Early stage (A) for patients with asymptomatic early tumors suitable for radical therapies, intermediate stage (B) comprises patients with asymptomatic multinodular HCC. Advanced stage (C) includes patients with symptomatic tumors and/or an invasive tumoral pattern, end-stage disease (D) contains patients with extremely grim prognosis that should merely receive symptomatic treatment [6].
Our finding of the prognostic indicators of death were the advanced child, AFP level >400 ng/ml, presence of metastases and invasion of the portal vein which joins Tandon et al. [7], these have shown in addition to the above described prognostic indicators that the clip score is also predictors of death. Grieco A et al. [8] founded that portal vein thrombosis; alpha fetoprotein, total bilirubin, and tumor size were significant predictors of survival. Okuda, CLIP, and BCLC scores were all able to predict survival (p=0.001). They identified two, four, and six risk groups, respectively, with a median survival ranging from 27 to 19 months for Okuda, 30 to 5 months for CLIP, and 43 to 7 months for BCLC. According to Marrero et al. [9], the independent predictors of survival were performance status (P < .0001), MELD score greater than 10 (P=0.001), portal vein thrombosis (P=0.0001), and tumor diameter greater than 4 cm (P=0.001). The Barcelona Clinic Liver Cancer (BCLC) staging system had the best independent predictive power for survival when compared with the others prognostic systems.
The future in terms of predictor factors of survival in HCC will certainly go towards the study of molecular phenotypes this is what has shown Calderaro J et al. [10] who concluded that HCC phenotype is tightly associated to its molecular alterations and underlying oncogenic pathways. The study evoked a novel subtype of HCC, designated as "macrotrabecular-massive" associated with poor survival (p<0.001), high alpha foeto-protein serum level (P=0.02), vascular invasion (P<0.001), TP53 mutations (P<0.001) and FGE 19 (P=0.02).
6. Conclusion
Hepatocellular carcinoma remains a tumor with a poor prognosis. The prognostic indicators of death, in our study, were respectively the advanced Child, the rate of AFP >400 ng/ml, the presence of metastases and invasion of the portal vein. Our results should be confirmed in a larger multicenter cohort to study the effect of multiple etiologies, ethnicity, and the effect of various treatments on overall survival. A consensus in prognostic staging for HCC is urgently needed to assure progress in the development of biomarkers for early detection and novel therapies.
Conflict of Interests
All authors agree with the content of the manuscript and there are no conflicts of interests between them.
Funding
No financial funding.
References
- Golabi P, et al. Mortality assessment of patients with hepatocellular carcinoma according to underlying disease and treatment modalities. Medicine (Baltimore) 96 (2017): e5904.
- Solmi L, Primerano AM, Gandolfi L. Ultrasound follow-up of patients at risk for hepatocellular carcinoma: results of a prospective study on 360 cases. Am J Gastroenterol 91 (1996): 1189-1194.
- Johnson PJ. Hepatocellular carcinoma: is current therapy really altering outcome? Gut 51 (2002): 459-462.
- The Cancer of Liver Italian Program (CLIP) Investigation. Prospective validation of the CLIP score: a new prognostic system for patients with hepatocellular carcinoma. Hepatology 31 (2000): 840-845.
- Dilou N, et al. Hepatocellular carcinoma survival prediction classifications. Gastroenterol clin biol 28 (2004): 359-366.
- Llovet JM, Bru` C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLCstaging classification. Semin Liver Dis 19 (1999): 329-338.
- Tandon GT, et al. Prognostic indicators in hepatocellular carcinoma: a systematic review of 72 studies. Liver International (2009): 1478-3223.
- Grieco A, et al. Prognostic factors for survival in patients with earlyintermediate hepatocellular carcinoma undergoing nonsurgical therapy: comparison of Okuda, CLIP, and BCLC staging systems in a single Italian centre. Gut 54 (2005): 411-418.
- Marrero et al. Prognosis of Hepatocellular Carcinoma: Comparison of 7 Staging Systems in an American Cohort. Hepatology (2005).
- Calderaro J, et al. Histological Subtypes of Hepatocellular Carcinoma Are Related To Gene Mutations and Molecular Tumour Classification. J Hepatol (2017).
