Posterior Capsular Rupture with Vitreous Loss in Assisted Surgeons-Towards a Better Understanding
Article Information
Tamer Adel Refai*
Research Institute of Ophthalmology, Giza, Egypt
*Corresponding Author: Tamer Adel Refai, Research Institute of Ophthalmology, Giza, Egypt
Received: 09 September 2019; Accepted: 25 September 2019; Published: 30 September 2019
Citation:
Tamer Adel Refai. Posterior Capsular Rupture with Vitreous Loss in Assisted Surgeons-Towards a Better Understanding. Journal of Ophthalmology and Research 2 (2019): 040-049.
View / Download Pdf Share at FacebookAbstract
Aim: To evaluate cases with posterior capsular rupture with vitreous loss among phacoemulsification patients performed by assisted surgeons in research Institute of ophthalmology.
Methods: Fourteen (14) eyes of fourteen patients in which posterior capsular rupture with vitreous loss had happened during phacoemulsification surgery performed by assisted ophthalmic surgeons at one sector of research institute of ophthalmology Giza-Egypt between February 2018 and August 2019. Patient age was recorded, the machine used in phacoemulsification, the operative step in which the capsular rupture and vitreous loss occurred, the nucleus grade (an indicator of the difficulty of the procedure) in addition to any added difficulties in the procedure as reported by questionnaire of the surgeon. Collected data were subjected to statistical analysis mainly by Chi-Squared test to compare the relative frequency of existence of the possible risk factors related to posterior capsular rupture and vitreous loss.
Results: In this study, according to the cataract nuclear grade, the highest percentage of posterior capsular rupture and vitreous loss for nuclear grade III nuclear cataracts (42.86%), although the Chi-squared test denotes a non significant difference (X2=2.55, P>0.05). For the phacoemulsification step, the highest percentage of vitreous loss occurred with the phacoemulsification (phaco II) step (42.86%) followed by the hydromaneuvers step and the phaco-division (i.e., phaco I) step (I14.29% each), followed by other steps, although the Chi-squared test showed a nonsignificant difference (X2=10.8, P>0.05). For the phacomachine used; a higher percentage of posterior capsular rupture and vitreous loss occurred with the Alcon Infiniti with OZil Torsional Handpiece (42.86% of cases), followed by the Oe
Keywords
Vitreous loss in assisted surgeons, Phacomachine, Phacoemulsification step-nuclear grade
Vitreous loss in assisted surgeons articles, Phacomachine articles, Phacoemulsification step-nuclear grade articles
Article Details
1. Introduction
In most developed countries, phacoemulsification surgery is one of the most commonly performed surgeries; owing to the simplicity of the procedures in the hands of trained ophthalmologists, the use of minimal-sized incisions, by the use of ultrasound energy and implantation of foldable intraocular lenses with early visual stability and minimal rehabilitation time [1] and with less need for full ocular akinesia [2, 3]. However phacoemulsification had a long learning curve for an ophthalmologist to reach a qualified proficient level [4]. Posterior capsular rupture with or without vitreous loss is considered the most undesirable complication intra-operatively [5-11] because it is associated with serious complications like retinal detachment, Cystoid macular oedema, glaucoma, recurrent uveitis as well as instability and dislocation of intraocular lenses (IOLs) [12]. Some studies had reported highest incidence of posterior capsular rupture and vitreous loss occurring during cortical removal as well as during emulsification of the last nuclear fragment where the posterior capsule can be aspirated into the phacotip [13].
Other researchers found that the main risk indicators identified were increasing age, brunescent or white cataract, pseudoexfoliation/phacodonesis, small pupil size, axial length >26 mm, and trainee status. It is inevitable that there are further factors that may be important, such as shallow anterior chamber depth (ACD) [14]. Multiple phacomachines had been used in phacoemulsification each has its specifications and phacoprobe dimentions, amongst them are the Alcon Infiniti with OZil Torsional Handpiece that shears the lens material, providing decreased repulsion (no jack hammer effect) while improving the thermal safety profile over traditional ultrasound, the Oertli Os3, with Venturi and peristaltic double pump switchable (from pedal, remote control or panel) during surgery with the dual function cassette that supports both pump and an air free fluidics system that is claimed to provide an immediate response to pressure changes, instant build up of suction power and stable anterior chamber and also the AMO Whitestar Signature where the Fusion Fluidics surge-prevention technology allows the use of high vacuum and flow settings to reduce phaco time and increase efficiency while improving chamber stability by anticipating occlusions and presumptively adjusting vacuum before occlusion breaks [15].
1.1 Purpose
Purpose of this study is to evaluate cases of phacoemulsification done by ophthalmologists needing assistance from senior staff in which posterior capsular rupture with vitreous loss had occurred to try to highlight the variable risk factors associated with vitreous loss and improve the phacoemulsification performance among assisted ophthalmologists to reach best patient’s welfare and satisfaction.
2. Materials and Methods
Fourteen cases which suffered from a posterior capsular rupture with vitreous loss during phacoemulsification surgery performed at one sector of the research institute of ophthalmology Giza-Egypt by assisted ophthalmologists between February 2018 and August 2019 were included in the study. Assisted surgeons included underskilled specialists, residents of the Research Institute in addition to, fellows and trainees at the research institute of ophthalmology. Patient age was recorded, the machine used in phacoemulsification (including; Alcon Infiniti with OZil Torsional Handpiece, Oertli Os3 and AMO Whitestar Signature) the operative step in which the capsular rupture and vitreous loss occurred, the nucleus grade (Graded from I to IV as an indicator of the difficulty of the procedure) in addition to any added difficulties in the procedure as reported by questionnaire of the surgeon.
2.1 The phacoemulsification procedure
- Topical anesthesia done by benoxite hydrochloride 0.4% eye drops instilled into the conjunctival sac.
- A 5-7 ml of local anesthetic mixture of equal amounts of (2% lidocaine with added hyaluronidase 15 IU) and 0.5. % bupivacaine) was injected at the medial canthus between the eyeball and the semilunaris fold by a 22-Gauge sharp-tipped needle with needle length 25 mm followed by an ocular massage for about 5 minutes to ensure adequate ocular analgesia and akinesia.
- A clear corneal incision was done by the keratome.
- Viscoelastic was used to fill and deepen the anterior chamber.
- Continuous curvilinear capsulorrhexis was initiated by bent-tipped cystitome and compelled by a capsulorrhexis forceps.
- BSS with a blunt tipped canula was used to perform hydrodissection and hydrodelineation of the nucleus followed by rotation of the nucleus.
- The phacoprobe was introduced through the clear corneal incision with irrigation on and the epinucleus anterior to the nucleus removed in the area of the capsulorrhexis.
- An initial groove was created in the nucleus and rotated 180 degrees to complete from the other side to separate the nucleus into 2 pieces using high phacopower, low vacuum level and low aspiration rate.
- The nucleus is again rotated 90 degrees and the same maneuver repeated to have the nucleus divided into 3 or 4 quadrants.
- Using moderate phacopower, high vacuum level and high aspiration rate, each nuclear quadrant was emulsified while reducing all parameters when dealing with the last quadrant.
- The epinucleus was emulsified with negligible phacopower, moderate vacuum level and moderate aspiration rate.
- The residual cortex was aspirated by the bi-manual irrigation aspiration canulae.
- The capsular bag was filled Viscoelastic material and IOL implanted.
- Hydration of the wound.
- In the event of posterior capsular rupture and vitreous loss, a good automated vitrectomy was performed (assisted by kenacort as possible), followed by removal of residual nuclear fragments assisted by viscoexpression after enlarging the incision as needed, followed by good anterior vitrectomy removing vitreous strands from anterior chamber and wound edges and removing residual lens matter by the Aspiration/aspriration and cutting function of the vitrectomy machine, followed by evaluation of the anterior capsular rim to implant whether a posterior chamber IOL or anterior chamber IOL, followed by closure of the wound with 10/0 nylon sutures as necessary.
Collected data were subjected to statistical analysis mainly by Chi-Squared test to compare the relative frequency of existence the possible risk factors related to posterior capsular rupture and vitreous loss.
3. Results
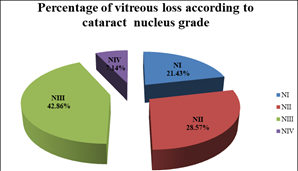
Patient's age ranged from 55 to 72 years with mean age (63.93 ± 5.27) years, the phaconucleus grade ranged from Grade I to Grade IV), the three phacomachines which were used in the operation included; Alcon Infiniti with OZil Torsional Handpiece, Oertli Os3 and AMO Whitestar Signature). Regarding the cataract nuclear grade, 21.43% of posterior capsular rupture and vitreous loss occurred with nuclear grade I, 28.57% with nuclear grade II, 42.86% with nuclear grade III and 7.14% with nuclear grade IV, where the comparison with the Chi-squared test denotes a non significant difference (X2=2.55, P>0.05) (Table 1), but there is a higher percentage among grade III nuclear cataracts (Figure 1).
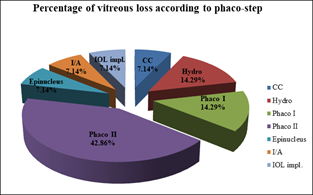
Regarding the phacoemulsification step, 7.14% of cases of posterior capsular rupture with vitreous loss occurred with the capsulorrhexis step, 14.29% with the hydromaneuvers step, 14.29% with the phaco-division (i.e., phaco I) step, 42.86% with the phacoemulsification (phaco II) step, 7.14% with epinucleus emoval, 7.14% with irrigation/Aspiration step 7.14% with intra-ocular lens implantation with the Chi-squared test denotes a non significant difference (X2=10.8, P>0.05) (Table 2), but there is a higher percentage among phacoemulsification step (i.e., phaco II step) (Figure 2).
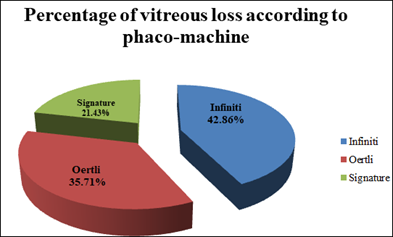
Regarding phacomachine used; 42.86% of posterior capsular rupture and vitreous loss occurred with the Alcon Infiniti with OZil Torsional Handpiece, 35.71% of cases occurred with the Oertli Os3 and 21.43% occurred with the AMO Whitestar Signature machine, where comparison with the Chi-squared test denotes a non significant difference (X2=1.0, P>0.05) (Table 3), but there is a higher percentage among Infiniti and Oertli phacomachines (Figure 3).
Regarding the presence of additional operative difficulties, 14.29% of cases with posterior capsular rupture occurred with the presence of small pupil intraoperatively, 14.29% with poor red reflex, 0% with positive vitreous pressure and 71.43% without any additional operative difficulty with the Chi-squared test denotes a non significant difference (X2=6.33, P>0.05) (Table 4), but there is a relatively higher percentage among cases with intraoperative small pupil and poor red reflex (Figure 4).
|
Cataract Grade |
NI |
NII |
NIII |
NIV |
Chi2 |
P-value |
Significance |
|
No.of eyes |
3 |
4 |
6 |
1 |
2.55 |
>0.05 |
nonsignificant |
|
Percentage of eyes |
21.43% |
28.57% |
42.86% |
7.1% |
Table 1: showing the relative frequency of posterior capsular rupture and vitreous loss among assisted surgeons, according to cataract nuclear grade and their comparison by Chi-squared test and significance among study.
Table 2: showing the relative frequency of posterior capsular rupture and vitreous loss among assisted surgeons, according to phacoemulsification step and their comparison by Chi-squared test and significance among study.
|
Phaco Machine |
Infiniti |
Oertli |
Signature |
Chi2 |
P-value |
Significance |
|
No.of eyes |
6 |
5 |
3 |
1.0 |
>0.05 |
Non significant |
|
Percentage of eyes |
42.86% |
35.71% |
21.43% |
Table 3: showing the relative frequency and percentage of posterior capsular rupture and vitreous loss among assisted surgeons according to phacomachine used and their comparison by Chi-squared test and significance among study.
|
Additional difficulty |
Small pupil |
Poor red reflex |
Positive vitreous pressure |
None |
Chi2 |
P-value |
Significance |
|
No.of eyes |
2 |
2 |
0 |
10 |
6.33 |
>0.05 |
Non significant |
|
Percentage of eyes |
14.29% |
14.29% |
0% |
71.43% |
Table 4: Showing the relative frequency of posterior capsular rupture and vitreous loss among assisted surgeons according to additional difficulties during phacoemulsification surgery and their comparison by Chi-squared test and significance among study.
Figure 4: Showing The Percentage Of Posterior Capsular Rupture And Vitreous Loss Among Assisted Surgeons According To Additional Difficulties During Phacoemulsification Surgery Among Study.
4. Discussion
Phacoemulsification; inspite of being one of the most commonly performed operations owing to its simplicity in the hands of experienced surgeons [1], yet one of the most serious operative complications is rupture of the posterior capsule with vitreous loss as it can result in multiple sequelae like chronic intraocular inflammation, intraocular infection, cystoid macular oedema and retinal detachment that may have bad effects on the patient’s visual acuity [16]. Several local factors had been recognized as risk factors for vitreous loss; including narrow palpebral fissures, deep set eyes, glaucoma and history of vitreous loss in the fellow eye [17]. Similarly, there are systemic features which had been found to be risk factors of vitreous loss including; obesity, marfan syndrome, systemic hypertension and diabetes mellitus [17]. Surgical training is another important risk factor for posterior capsular rupture with vitreous loss, the incidence of which usually ranges from PC tear with vitreous loss between 2.8% and 10% among training surgeons [18-21]. Lockwood et al. found that the main risk indicators identified were increasing age, brunescent or white cataract, pseudoexfoliation/phacodonesis, small pupil size, axial length>26 mm, and trainee status. It is inevitable that there are further factors that may be important, such as shallow anterior chamber depth (ACD) [14]. Temel et al. had reported highest incidence of posterior capsular rupture and vitreous loss occurring during cortical removal as well as during emulsification of the last nuclear fragment where the posterior capsule can be aspirated into the phacotip [13]. Zare et al., studied vitreous loss among ophthalmic residents and fellows and they found that the highest rate of vitreous loss occurred in patients with dense nuclear cataracts. Older age, female sex, small pupil, small capsulorrhexis, presence of pseudoexfoliation, and high myopia were significantly associated with vitreous loss. The rate of vitreous loss was five folds higher in residents compared to fellows which emphasized the positive effect of training [22].
In this study, Regarding the cataract nuclear grade, the highest percentage of vitreous loss occurred in grade III nuclear cataracts (42.86%) followed by grade III (28.57%) followed by grade II (21.43%) and lastly grade IV (7.14%) with nuclear grade IV (which is usually done only by highly skilled surgeons), and in spite of Chi-squared test showing a non significant difference, yet there is a higher percentage among grade III nuclear cataracts which agrees with previous studies. Regarding the phacoemulsification step, the highest percentage of vitreous loss occurred with the phacoemulsification (phaco II) step (42.86%) followed by the hydromaneuvers step and the phaco-division (i.e., phaco I) step (I14.29%) followd by the capsulorrhexis step (7.14%), epinucleus emoval (7.14%), irrigation/Aspiration step and the intra-ocular lens implantation step (7.14%) and inspite that the Chi-squared test showed a non significant difference (X2=10.8, P >0.05), but there is a higher percentage among phacoemulsification step (i.e., phaco II step) which agreed partially with the results found by Temel et al. 2003. Regarding phacomachine used; the highest percentage of posterior capsular rupture and vitreous loss (42.86%) occurred with the Alcon Infiniti with OZil Torsional Handpiece, followed by the Oertli Os3 (35.71%) and then the AMO Whitestar Signature machine (21.43%), and again the Chi-squared test denotes a non significant difference, but there is a higher percentage among Infiniti and Oertli phacomachines and this comparison between different phacomachines regarding vitreous loss where not included in the previously mentioned studies.It was expected to a have a high percentage of vitreous loss related to the Alcon Infiniti with OZil Torsional Handpiece being the most preferable phacomachine by ophthalmologists; owing its small handpiece diameter demanding a small incision size, thus providing good stability of the anterior chamber throughout the phaco-procedure, but the the high percentage of posterior capsular rupture and vitreous loss related to the Oertli Os3 phacomachine (which is not preferable to ophthalmologists owing to its large diameter handpiece) was not expected which denotes a higher risk of this complication with this phacomachine at least for underskilled assisted surgeons. Regarding the presence of additional operative difficulties, a relatively higher percentage of posterior capsular rupture and vitreous loss (14.29%) occurred in the presence of small pupil intraoperatively and poor red reflex, which agreed with previous studies.
5. Conclusion
During performing phacoemulsification by assisted surgeons, in order to decrease the incidence of posterior capsular rupture with vitreous loss, special care should be taken while performing phacoemulsifiaction of the nucleus (i.e., phaco II), and it is better to avoid working on grade III nuclear density and on the Oertli-phaomachime.Also it is recommended to have good pupillary dilatation with good red reflex.
Financial Disclosure
The author has no proprietary or commercial interest in any of the materials discussed in this article.
Conflicts of Interest
There are no conflicts of interest.
Acknowledgements
Special acknowledgement is presented to Research Institute of Ophthalmology, Giza, Egypt, providing valuable funding and training for ophthalmologists while providing high operative standards to the patients thus deserving acknowledgement.
References
- Dick HB. Bladeless custom femtosecond laser-assisted refractive cataract surgery? Let’s give our latest breakthrough surgical technique a name that fits. J Refract Surg 31 (2015): 346.
- Zhao LQ, Zhu H, Zhao PQ, et al. Topical anesthesia versus regional anesthesia for cataract surgery: a meta-analysis of randomized controlled trials. Ophthalmology 119 (2012): 659-667.
- Ezra DG, Allan BD. Topical anaesthesia alone versus topical anaesthesia with intracameral lidocaine for phacoemulsification. Cochrane Database Syst Rev 3 (2007): 005276.
- Tzamalis A, Lamprogiannis L, Chalvatzis N, et al. Training of Resident Ophthalmologists in Cataract Surgery: A Comparative Study of Two Approaches (2015): 1-7.
- Prasad S. Phacoemulsification learning curve: experience of two junior trainee ophthalmologists. Journal of Cataract & Refractive Surgery 24 (1998): 73-77.
- Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. Journal of Cataract and Refractive Surgery 24 (1998): 66-72.
- Hennig A, Schroeder B, and Kumar J. Learning phacoemulsification.Results of different teaching methods. Indian Journal of Ophthalmology 52 (2004): 233-234.
- Albanis CV, Dwyer MA, Ernest JT, Outcomes of extracapsular cataract extraction and phacoemulsification performed in a university training program. Ophthalmic Surgery and Lasers 29 (1998): 643-648.
- Badoza DA, Jure T, Zunino LA, et al. State-of the-art phacoemulsification performed by residents in Buenos Aires, Argentina. Journal of Cataract and Refractive Surgery 25 (1999): 1651-1655.
- Blomquist PH, Rugwani RM. Visual outcomes after vitreous loss during cataract surgery performed by residents. Journal of Cataract and Refractive Surgery 28 (2002): 847-852.
- Smith JH. Teaching phacoemulsification in US ophthalmology residencies: can the quality be maintained? Current Opinion in Ophthalmology 16 (2005): 27-32.
- Johansson B, Lundström M, Montan P, et al. Capsule complication during cataract surgery: Long-term outcomes: Swedish Capsule Rupture Study Group report 3. J Cataract Refract Surg, 35 (2009): 1694-1698.
- Temel M, Osher RH. Posterior capsule tear resulting from faulty instrumentation. J Cataract Refract Surg 29 (2003): 619-620.
- Lockwood A, Kirwan JF. Risk stratification for posterior capsule rupture and vitreous loss during cataract surgery Eye 24 (2010): 389-390.
- Jacob AT. High-End Phaco Systems: A Comparison. Kerala Journal of Ophthalmology 4 (2008): 382-384.
- Jaffe NS, Jaffe MS, Jaffe GF. Cataract surgery and its complications. (6th) St Louis 4 (2009): 208-212.
- Gimbel HV. Posterior capsule tears using phacoemulsification-causes, prevention and management. Eur J Implant Refract Surg 2 (1990): 63-69.
- Albanis CV, Dwyer MA, Ernest JT. Outcomes of extracapsular cataract extraction and phacoemulsification performed in a university training program. Ophthalmic Surgery and Lasers 29 (1998): 643-648.
- Badoza DA, Jure T, Zunino LA, et al. State-ofthe-art phacoemulsification performed by residents in Buenos Aires, Argentina. Journal of Cataract and Refractive Surgery 25 (1999): 1651-1655.
- Blomquist PH, Rugwani RM.Visual outcomes after vitreous loss during cataract surgery performed by residents. Journal of Cataract and Refractive Surgery 28 (2002): 847- 852.
- Smith GH. Teaching phacoemulsification in US ophthalmology residencies: can the quality be maintained?. Current Opinion in Ophthalmology 16 (2005): 27-32.
- Zare M, javadi MA, Einollani B, et al. Risk Factors for Posterior Capsule Rupture and Vitreous Loss during Phacoemulsification. J Ophthalmic Vis Res 4 (2009): 208-212.