Modified Z-Plasty for Cervical Spine Myelopathy: A Not-So-Obsolete Method of Laminoplasty
Article Information
Truc Tam Vu*, Hanh The Nguyen, Riet Ngoc Do, Thanh Dang Le, Vien Chi Tieu, Tram Thi Bao Nguyen, Khai Dang Tran, Lan Hoang Bui, Tuan Duc Ha, Long Thanh Ngo, Phuc Nghia Diep, Tin Trong Nguyen
Department of Spinal Surgery B, Hospital for Traumatology and Orthopedics, Ho Chi Minh, Vietnam
*Corresponding Author: Truc Tam Vu, Department of Spinal Surgery B, Hospital for Traumatology and Orthopedics, Ho Chi Minh, Vietnam
Received: 14 May 2020; Accepted: 26 May 2020; Published: 01 June 2020
Citation:
Truc Tam Vu, Hanh The Nguyen, Riet Ngoc Do, Thanh Dang Le, Vien Chi Tieu, Tram Thi Bao Nguyen, Khai Dang Tran, Lan Hoang Bui, Tuan Duc Ha, Long Thanh Ngo, Phuc Nghia Diep, Tin Trong Nguyen. Modified Z-Plasty for Cervical Spine Myelopathy: A Not-So-Obsolete Method of Laminoplasty. Journal of Spine Research and Surgery 2 (2020): 058-066.
View / Download Pdf Share at FacebookAbstract
Introduction: It is generally accepted that laminoplasty is a safe and reliable surgical treatment for cervical spine myelopathy (CSM) due to spinal canal stenosis. There are multiple techniques of laminoplasty for spinal cord decompression and most of them require expensive instruments to stabilize the laminae. From 2005 to 2015, we applied the modified Z-plasty (Sakou's technique) for CSM patients in an attempt to reduce the cost of treatment.
Materials and methods: This is a retrospective study. CSM patients treated by modified Z-plasty technique were selected. We applied the Sakou’s technique, according to which the laminae will be opened in different directions alternatively. We use the JOA score and recovery rate of Hirabayashi to assess the neurological recovery and the Neck Disability Index (NDI) for the cervical functional outcome.
Results: There were 42 patients with the mean follow-up duration of 10 years (5-15 years), male: female ratio of 3:1 and mean age of 61. The mean operating time and blood loss per lamina were 40 minutes and 45ml, respectively. The canal expanding index was 4.2mm (3-5 mm). The mean pre- and postoperative JOA score were 11.1 and 14.7, respectively (p<0.05). For the axial pain, the mean NDI was 18 point with 88% of cases having as good and very good cervical function. For complications, there were 3 cases of C5 palsy with full recovery after one year.
Conclusion: Being considered as an old-fashioned surgery, the modified Z-plasty can still provide good clinical and radiological outcomes to cervical myelopathic patients. The absence of hardware such as titanium plates or hydroxyapatite spacers reduces the risk of infection and the cost of treatment. Considering the risk-benefit and cost-benefit ratio, this operation is suitable for low-income patients in developing countries.
Keywords
Cervical Spine Myelopathy, Modified Z-Plasty, Open Door Laminoplasty, French Door Laminoplasty
Cervical Spine Myelopathy articles Cervical Spine Myelopathy Research articles Cervical Spine Myelopathy review articles Cervical Spine Myelopathy PubMed articles Cervical Spine Myelopathy PubMed Central articles Cervical Spine Myelopathy 2023 articles Cervical Spine Myelopathy 2024 articles Cervical Spine Myelopathy Scopus articles Cervical Spine Myelopathy impact factor journals Cervical Spine Myelopathy Scopus journals Cervical Spine Myelopathy PubMed journals Cervical Spine Myelopathy medical journals Cervical Spine Myelopathy free journals Cervical Spine Myelopathy best journals Cervical Spine Myelopathy top journals Cervical Spine Myelopathy free medical journals Cervical Spine Myelopathy famous journals Cervical Spine Myelopathy Google Scholar indexed journals Modified Z-Plasty articles Modified Z-Plasty Research articles Modified Z-Plasty review articles Modified Z-Plasty PubMed articles Modified Z-Plasty PubMed Central articles Modified Z-Plasty 2023 articles Modified Z-Plasty 2024 articles Modified Z-Plasty Scopus articles Modified Z-Plasty impact factor journals Modified Z-Plasty Scopus journals Modified Z-Plasty PubMed journals Modified Z-Plasty medical journals Modified Z-Plasty free journals Modified Z-Plasty best journals Modified Z-Plasty top journals Modified Z-Plasty free medical journals Modified Z-Plasty famous journals Modified Z-Plasty Google Scholar indexed journals Open Door Laminoplasty articles Open Door Laminoplasty Research articles Open Door Laminoplasty review articles Open Door Laminoplasty PubMed articles Open Door Laminoplasty PubMed Central articles Open Door Laminoplasty 2023 articles Open Door Laminoplasty 2024 articles Open Door Laminoplasty Scopus articles Open Door Laminoplasty impact factor journals Open Door Laminoplasty Scopus journals Open Door Laminoplasty PubMed journals Open Door Laminoplasty medical journals Open Door Laminoplasty free journals Open Door Laminoplasty best journals Open Door Laminoplasty top journals Open Door Laminoplasty free medical journals Open Door Laminoplasty famous journals Open Door Laminoplasty Google Scholar indexed journals French Door Laminoplasty articles French Door Laminoplasty Research articles French Door Laminoplasty review articles French Door Laminoplasty PubMed articles French Door Laminoplasty PubMed Central articles French Door Laminoplasty 2023 articles French Door Laminoplasty 2024 articles French Door Laminoplasty Scopus articles French Door Laminoplasty impact factor journals French Door Laminoplasty Scopus journals French Door Laminoplasty PubMed journals French Door Laminoplasty medical journals French Door Laminoplasty free journals French Door Laminoplasty best journals French Door Laminoplasty top journals French Door Laminoplasty free medical journals French Door Laminoplasty famous journals French Door Laminoplasty Google Scholar indexed journals multilevel stenosis articles multilevel stenosis Research articles multilevel stenosis review articles multilevel stenosis PubMed articles multilevel stenosis PubMed Central articles multilevel stenosis 2023 articles multilevel stenosis 2024 articles multilevel stenosis Scopus articles multilevel stenosis impact factor journals multilevel stenosis Scopus journals multilevel stenosis PubMed journals multilevel stenosis medical journals multilevel stenosis free journals multilevel stenosis best journals multilevel stenosis top journals multilevel stenosis free medical journals multilevel stenosis famous journals multilevel stenosis Google Scholar indexed journals cervical lordosis articles cervical lordosis Research articles cervical lordosis review articles cervical lordosis PubMed articles cervical lordosis PubMed Central articles cervical lordosis 2023 articles cervical lordosis 2024 articles cervical lordosis Scopus articles cervical lordosis impact factor journals cervical lordosis Scopus journals cervical lordosis PubMed journals cervical lordosis medical journals cervical lordosis free journals cervical lordosis best journals cervical lordosis top journals cervical lordosis free medical journals cervical lordosis famous journals cervical lordosis Google Scholar indexed journals laminoplasty articles laminoplasty Research articles laminoplasty review articles laminoplasty PubMed articles laminoplasty PubMed Central articles laminoplasty 2023 articles laminoplasty 2024 articles laminoplasty Scopus articles laminoplasty impact factor journals laminoplasty Scopus journals laminoplasty PubMed journals laminoplasty medical journals laminoplasty free journals laminoplasty best journals laminoplasty top journals laminoplasty free medical journals laminoplasty famous journals laminoplasty Google Scholar indexed journals spinal surgery articles spinal surgery Research articles spinal surgery review articles spinal surgery PubMed articles spinal surgery PubMed Central articles spinal surgery 2023 articles spinal surgery 2024 articles spinal surgery Scopus articles spinal surgery impact factor journals spinal surgery Scopus journals spinal surgery PubMed journals spinal surgery medical journals spinal surgery free journals spinal surgery best journals spinal surgery top journals spinal surgery free medical journals spinal surgery famous journals spinal surgery Google Scholar indexed journals Orthopedics articles Orthopedics Research articles Orthopedics review articles Orthopedics PubMed articles Orthopedics PubMed Central articles Orthopedics 2023 articles Orthopedics 2024 articles Orthopedics Scopus articles Orthopedics impact factor journals Orthopedics Scopus journals Orthopedics PubMed journals Orthopedics medical journals Orthopedics free journals Orthopedics best journals Orthopedics top journals Orthopedics free medical journals Orthopedics famous journals Orthopedics Google Scholar indexed journals
Article Details
1. Introduction
Cervical spine myelopathy is a medical condition characterized by a chronic compression of the spinal cord by spondylotic osteophytes, disc herniation, ossification of the longitudinal ligament (OPLL), hypertrophy or ossification of the ligamentum flavum etc. Surgery is indicated when conservative treatments fail, with the goal of enlarging the stenotic canal. It is generally accepted that for multilevel stenosis (from 3 levels and above) with preserved cervical lordosis, laminoplasty is a reasonable choice as it can provide sufficient decompression as well as relatively avoid possible complications of laminectomy (eg restenosis, kyphotic deformity etc). Oyama and Hattori in 1973 have presented their original Z-plasty technique (Figure 1A) [1], to which two modifications including Sakou's (Figure 1B) [2] and Chiba university techniques were later proposed (Figure 1C) [3]. The concept of enlarging the spinal canal by just opening the laminae without excising it became popular in Japan when Hirabayashi developed the open-door [4, 5] and Kurukawa the French-door technique [6].
Naito et al in 1994 have conducted a research comparing the three main methods of laminoplasty and concluded that all of them can provide similar decompressive effect and clinical outcome, but the Z-plasty was the most technical demanding and time consuming of the three [9]. After this study, Z-plasty became gradually obsolete as most of spinal surgeons worldwide prefered either open-door or French-door methods. Despite that trend, from 2005 to 2015, the Z-laminoplasty was the technique of choice of our department of spinal surgery for multilevel cervical stenosis as it did not require any expensive devices to secure the laminae and provided good outcome.
2. Material and Method
This is a retrospective study. From 2005 to 2015, 97 CSM patients were operated with the Z-plasty technique in the department of Spinal Surgery B, Hospital for Traumatology and Orthopedics at Ho Chi Minh city, Vietnam. We invited them for final evaluation at our hospital by mail or phone call. There were 42 patients accepting to participate in this study with sufficient pre- and postoperative images. Informed consents were obtained from all patients.
2.1 Indication of surgery
Patients with cervical myelopathic symptoms secondary to multilevel spinal stenosis (from three levels and above) with preserved cervical lordosis, K line positive and no gross instablity or severe axial pain.
2.2 Operative technique
Patient was placed in a prone position on the surgical frame. The head is firmly held in the neutral position by the Mayfield tong. The midline skin incision from C2 to C7 spinous processes was used on a systematic basis. We then exposed through the avascular plane between two layers of the nuchal ligament down to the tips of spinous process from C3 to C6. Care was taken during exposure in order to preserve the attachment of the subcapital muscle at C2 and that of the nuchal ligament at C7 vertebra. The laminae from C3 to C6 were exposed with cautery bilaterally until the facet joint then blunt dissection continued the work in an attempt to protect the capsules. Yellow ligaments between C2 and C7 levels were removed in order to facilitate the opening of the laminae to both sides. The laminae were then opened in the zigzag fashion (for example the C3 lamina was opened to the left side, the C4 lamina to the right side and C5 to the left side and C6 to the right side). Two-milimeter burr was used to make a hole at the cutting edge of each lamina. The laminae were held against each other in the open position by non-absorbable suture through the aforementioned drill holes (Figure 1B). The incision was then drained and closed in layers. The patient was instructed to wear hard collar continously in the next six weeks and on intermitten basis during six weeks after, alternatively with rehabilitation excersices to restore the cervical range of motion.
2.3 Neurological evaluation
Pre- and postoperative neurological status of each
patient was evaluated using the Japanese Orthopaedic Association (JOA) system. To assess the neurological recovery, the recovery rate proposed by Hirabayashi and colleagues was calculated by the following formula: recovery rate (%) = ([postoperative score - preoperative score] ÷ [17 [full]- [preoperative score]) x 100. Neurological outcome was classified by the Hirabayashi's classification, according to which 75% to 100% was designated as very good, 50 to 74% as good, 25 to 49% as fair, and 0 to 24% as poor.
2.4 Clinical evaluation
The neck pain or discomfort was evaluated by using the Neck Disability Index (NDI) system. The Neck Disability Index (NDI) is designed to measure neck-specific disability. The questionnaire has 10 items concerning pain and activities of daily living including personal care, lifting, reading, headaches, concentration, work status, driving, sleeping and recreation.
2.5 Radiological evaluation
The enlarging of the spinal canal was assessed with lateral Xray. The pre- and postoperative AP distance of the spinal canal at each disc level from C3 to C6 was measured in all cases. The canal expanding index was defined as the difference between the final and preoperative AP diameter (in milimeter) of the spinal canal at each disc level. Magnetic resonance imaging was also performed as routine to evaluate the expansion of the thecal sac at each disc level after decompression. C2-7 lordotic angle was also measured on pre- and postoperative lateral Xray.
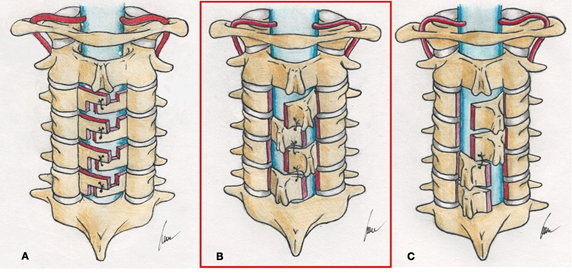
Figure 1: Original Z-laminoplasty (Hattori's method) (A) and modified techniques including: Sakou's method (B), Chiba university method (C). Note that the technique of our department is Sakou's Z-plasty (in the red box). Source: drawn by the corresponding author).
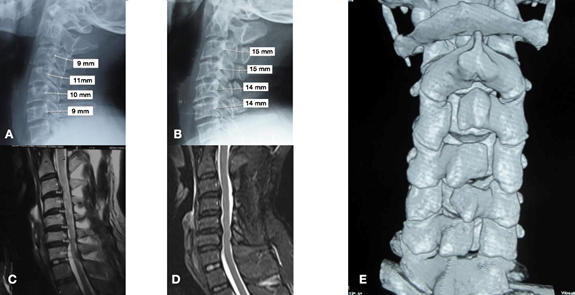
Figure 2: Illustration case: 60 year-old female patient underwent Z-plasty from C3 to C6 for multilevel cervical stenosis. Preoperative Xray (A) and MRI (C) showed acquired and congenital stenosis from C3 to C6 with well-preserved cervical lordosis. Final Xray (B) and MRI (D) after 15 years depicted wider spinal canal after Z plasty with mild residual stenosis at C5/6 and C6/7. The JOA score of this patient increased from 11 point preop to 16 at final follow up. CT scan reconstruction at final follow up showed the zigzag layout of the Z-plasty with good bone fusion of the hinges.
|
Preoperative |
Final follow up |
p |
|
|
Clinical outcome |
|||
|
mean JOA |
11.1 |
14.7 |
<0.05 |
|
mean Hirabayashi ratio |
68% |
||
|
mean NDI |
23 |
18 |
>0.05 |
|
Radiological outcome |
|||
|
mean canal diameter |
12.3mm |
16.8mm |
<0.05 |
|
mean expansion index |
4.2mm |
||
|
mean thecal sac diameter |
6.6mm |
11.2mm |
<0.05 |
|
mean C2-7 lordotic angle |
21.10 |
19.3 0 |
>0.05 |
Table 1: Clinical and radiological outcomes of 42 patients after undergoing decompression by Z-plasty.
|
Gender |
Age |
Preoperative canal diameter (mm) |
Postoperative canal diameter (mm) |
Final follow up canal diameter (mm) |
|
|
Patient 1 |
Male |
52 |
8 |
14 |
11 |
|
Patient 2 |
Male |
59 |
9 |
15 |
12 |
|
Patient 3 |
Female |
62 |
8 |
15 |
11 |
Table 2: Patients with spring-back closure as complication.
|
Surgical time per lamina (minute) |
Blood loss per lamina (milliliter) |
|
|
Open door (Naito) |
29 ±6,2 |
93 ±13 |
|
French door (Naito) |
32 ±6,4 |
90 ±11 |
|
Z-plasty (Naito) |
48 ± 7,1 |
121± 21 |
|
Z-plasty (Our study) |
40 ± 13 |
45 ± 21 |
Table 3: Comparing our surgical parameters with those of Naito's study.
3. Results
There were 42 patients recruited in this study with the mean follow up duration of 10 years (5- 15 years), the male: female ratio of 3:1 and the mean age of the population of 65 (46- 82). The average operative time in total was approximately 140 minutes (120–180 minutes) and 40 minute per lamina (30-45 minutes). The average total blood loss was was 130 ml (90–300 ml) and 45ml per lamina (25-75ml). The radiological and clinical outcomes are displayed in Table 1. The mean recovery rate of Hirabayashi was 68% with 75% of patients having from good to very good outcome. The NDI at final follow up was 18 with 88% of patients having from good to very good cervical function with minimal to mild pain during daily activities. For complications, there were 3 case (7.2 %) having C5 palsy after the surgery. After checking with postoperative CT scans revealing no residual foraminal stenosis, the protocol was to wait and see and all three patients had full recovery one year after. In other three patients (7.2 %), lamina closure has been detected by comparing the immediate postoperative xray and the final xray (Table 2). However, this complication did not have any negative effect on the neurological recovery, therefore the protocol was also observing. There was one case of superficial infection well controlled with oral antibiotic. No dural tears or deep infections have been recorded.
4. Discussion
The Z-plasty technique has been described and reported by Oyama and Hattori in 1974. The original method was time consuming and technical demanding when the Z-shaped cut line must be done at each lamina (Figure 1A) [7]. In 1984 Tomimura and Sakou have modified this surgery by open each lamina as a whole in different directions in an attempt to simplify the procedure and reduce the time of surgery (Figure 1B) [8]. This is the technique our department of spinal surgery has been using from 2005 to 2015 before we switched to open door technique when titanium plates became available. Last but not least, in 1987 Watanabe proposed the Chiba university modification according to which the C3 and C4 laminae will be opened to one side and the other two to the other side (Fig 1C). Despite those modifications, the Z-plasty became gradually obsolete when Hirabayashi’s [1] and Kurukawa’s techniques [5] have been presented in 1983 and 1984, consecutively. However, those two latter techniques are not without drawbacks. For the open-door laminoplasty, the asymmetry of the two masses of paraspinal muscle could lead to suboptimal clinical and neurological outcome. On the one hand, the canal is opened to one side and hinged on the other and this can create an asymmetric expansion of the canal [11, 12, 13]. When bilateral foraminal stenosis exists, open door laminoplasty may increase the possibility of C5 nerve palsy due inadequate foraminal decompression or asymmetrical decompression [14]. One the other hand, unilateral open-door laminoplasty results in skeletal asymmetry and causes asymmetrical muscular approximation [12, 15]. Studies have demonstrated that patients treated with open door techique reported more axial pain than those with French door method [16]. For the French-door technique, the main issue is how to keep the laminar halves open bilaterally. The conventional technique requires expensive hydroxyapatite spacers that could be a problem for low-income patients, especially when the device is not covered by the insurance. One feasible solution is using iliac bone block, which in turn can lead to donor site complications [17]. Another alternative is harvesting strut graft from C3-C6 spinous processes [18]. This technique appeared to be beneficial in the setting of cost-effectiveness and donor site complications. However, it was time consuming and not very suitable for Vietnamese patients with relatively small size spinous processes.
In a nutshell, the symmetry of the paraspinal muscles might have an important role in postoperative outcome and beside French-door laminoplasty, only Z-plasty can meet that requirement. When systematically searching in the literature, we noticed that the concept of opening the laminae in the zigzag pattern is not entirely out of date. Iencean et al in 2007 have reported a case serie of 23 patients treated by altenating open-door laminoplasty with satisfactory results [19]. The authors also open the laminae in different directions with a zigzag configuration. The only difference from our technique is the way they secure the open laminae by suturing the spinous processe to the capsule on the hinge side, similar to Hirabayashi's technique. Arantes et al in 2014 [29] reported a case serie treated by a technique similar to Chiba university technique [3], according to which two first laminae (C3 and C4) will be open to one side and the other two (C5 and C6) to the other side. Despite the new name "two-open-door laminoplasty", this is the modification of the original Z-plasty. In 2016, the team of Lee has proposed a novel en-bloc laminoplasty technique using translaminar screw as fixation [20]. They also preferred to open the laminae with a zigzag pattern in order to maintain the symmetry of the neck and preserve the nuchal ligament. We have been using the Z-plasty method for most of our patients with the aim of reducing the cost of treatment, avoiding donor site morbidity and preserving the symmetry of the neck. Naito in 1994 have compared three different methods including open-door, French-door and Z-plasty. The conclusion was no differences in regards to neurological outcome and axial pain have been found, however the Z-plasty was the least favorable choice because of largest blood loss and longest surgical duration. Table 3 displays the surgical parameters of Naito's and those of our study. It is noticeable that our surgical time per lamina is significantly shorter than that of the Z-plasty group of Naito. This difference can be explained by the fact that we used modified Z-plasty (Sakou's technique) whereas Naito et al have used the original one (Hattori method) with more complexity. Our surgical time per lamina was longer than that of the open-door and French-door groups but this difference has no clinical significance and can be compensated by the lower blood loss per lamina when compared with Naito's data.
The mean neurological recovery rate of our study (68%) was in line with that of laminoplasty studies in general [1-10]. Our mean canal expansion index of 4.2mm was sufficient for optimal neurological decompression as recommended by Gu et al [21]. Excessive opening of the lamina may cause the cord to migrate and extend posteriorly. In such cases, traction and tethering of the nerve root secondary to posterior shift of the spinal cord may occur, which has been considered as a main factor in postoperative C5 nerve root palsy [22-24]. The decompression effect has been confirmed by final MRI scans showing the enlargement of the AP diameter of the thecal sac from 6.6 preoperative to 11.2mm at final follow up. For all operated patients, we never tried to enlarge the canal too widely and that might help to minimize the C5 palsy rate (3 case, 7.2 %). To our understanding, our complication rate stayed within the acceptable range [22-24]. One potential and worrysome complication of Z-plasty is spring-back closure when the laminae were secured only by non-absorbable suture. Wang et al in their study have shown that spring-back closure with Hirabayashi technique could be as high as 10% [25]. In our study this undesirable event occured in 7.2% and fortunately it did not require any revision surgery. Last but not least, our patients reported mild to moderate axial pain at final follow up and for most of them, the neck discomfort did not aggravate with time. In agreement with other authors [26-28], we tried our best to protect the soft tissue attachment at C2 and C7 spinous processes during exposure and took great care when closing the incision. Finally, the cervical lordosis of our patients has been well preserved, even in those with a follow up duration longer than ten years.
5. Conclusion
Being considered as an old-fashioned surgery, the Z-plasty is a safe and reliable technique that can provide good clinical and radiological outcomes to cervical myelopathic patients. The absence of hardware such as titanium plates or hydroxyapatite spacers reduces the risk of infection as well as the cost of treatment. Considering the risk-benefit and cost-benefit ratio, this operation is highly suitable for low-income patients in developing countries.
References
- Oyama M, Hattori S, Moriwaki N, et al. A new method of cervical laminectomy. Chubu Nippon Seikeigeka Gakkai Zasshi 16 (1973): 792-794.
- Tomimura K, Morizonno Y. Osteoplastic enlargement of the cervical canal for cervical spondylosis. Rinsho Seikeigeka 19 (1984): 491-497.
- Watanabe T, Inoue S. Expansive laminoplasty (Chiba modification) for cervical myelopathy. Shujutsu 41 (1987): 519- 527.
- Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open door laminoplasty for cervical spinal stenoticmyelopathy. Spine 8 (1983): 693-699.
- Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty formyelopathy in ossifiation of the posterior longitudinal ligament. Clin Orthop 359 (1999): 35-48.
- Kurokawa T, Tsuyama N, Tanaka H. Enlargement of spinal canal by the sagittal splitting of spinal processes for cervicalspondylotic myelopathy. Rinsho Seikeigeka 19 (1984): 483-490.
- Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine 10 (1985): 729-736.
- Kawai S, Sunago K, Doi K, et al. Cervical laminoplasty (Hattori’s method). Procedure and follow-up results. Spine 13 (1998): 1245-1250.
- Naito M, Ogata K, Kurose S, et al. Canal-expansive laminoplasty in 83 patients withcervical myelopathy: A comparative study of three different procedures. International Orthopaedics 18 (1994): 347-351.
- Wang LN, Wang L, Song YM, et al. Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. Int Orthop 40 (2016): 1267-1274.
- Maeda T, Arizono T, Saito T, et al. Cervical alignment, range of motion, an instability after cervical laminoplasty. Clin Orthop Relat Res 9 (2002): 132-138.
- Azuma Y, Kato Y, Taguchi T. Etiology of cervical myelopathy induced by ossification of the posterior longitudinal ligament: determining the responsible level of OPLL myelopathy by correlating static compression and dynamic factors. J Spinal Disord Tech 23 (2010): 166-169.
- Shaffrey CI, Wiggins GC, Piccirilli CB, et al. Modified open-door laminoplasty for treatment of neurological deficits in younger patients with congenital spinal stenosis: analysis of clinical and radiographic data. J Neurosurg 90 (1999): 170-177.
- Komagata M, Nishiyama M, Endo K, et al. Prophylaxis of C5 palsy after cervical expansive laminoplasty by bilateral partial foraminotomy. Spine J 4 (2004): 650-655.
- Chiba K, Toyama Y, Matsumoto M, et al. Segmental motor paralysis after expansive open-door laminoplasty. Spine (Phila Pa 1976) 27 (2002): 2108-2115.
- Okada M, Minamide A, Endo T, et al. A Prospective Randomized Study of Clinical Outcomes in Patients With Cervical Compressive Myelopathy Treated With Open-Door or French-Door Laminoplasty. Spine 34 (2009): 1119-1126.
- Dimitriou R, Mataliotakis G I, Angoules A G, et al. Complications following autologous bone graft harvesting from the iliac crest and using the RIA: A systematic review. Injury 42 (2011): S3-S15.
- Nakashima H, Imagama S, Ito Z, et al. Essential Surgical Technique for French-Door (Double-Door) Laminoplasty. JBJS Essential Surgical Techniques 5 (2015): e2.
- Iencean S M. Alternating cervical laminoplasty for cervical spondylotic myelopathy. The Journal of Bone and Joint Surgery. British 89-B (2007): 639-641.
- Lee S E, Jahng T-A, Kim H-J. En Bloc Cervical Laminoplasty Using Translaminar Screws (T-laminoplasty). Clinical Spine Surgery 29 (2016): E296-E302.
- Gu Z, Zhang A, Shen Y, et al. Relationship between the laminoplasty opening size and the laminoplasty opening angle, increased sagittal canal diameter and the prediction of spinal canal expansion following open-door cervical laminoplasty. European Spine Journal 24 (2015): 1613-1620.
- Imagama S, Matsuyama Y, Yukawa Y, et al. C5 palsy after cervical laminoplasty: a multicentre study. J Bone Joint Surg Br, 92 (2010): 393-400.
- Tsuzuki N, Abe R, Saiki K, et al. Extradural tethering effect as one mechanism of radiculopathy complicating posterior decompression of the cervical spinal cord. Spine 21 (1996): 203-211.
- Uematsu Y, Tokuhashi Y, Matsuzaki H. Radiculopathy after laminoplasty of the cervical spine. Spine 23 (1998): 2057-2062.
- Wang HQ, Mak KC, Samartzis D, et al. “Spring-back” closure associated with open-door cervical laminoplasty. The Spine Journal 11 (2011): 832-838.
- Cho CB, Chung KC, Oh JY, et al. Axial Neck Pain after Cervical Laminoplasty. J Korean Neurosurg Soc 47 (2010): 107-111.
- Sakaura H, Hosono N, Mukai Y, et al. Preservation of the Nuchal Ligament Plays an Important Role in Preventing Unfavorable Radiologic Changes After Laminoplasty. Journal of Spinal Disorders & Techniques 21 (2008): 338-343.
- Takeuchi T, Shono Y. Importance of preserving the C7 spinous process and attached nuchal ligament in French-door laminoplasty to reduce postoperative axial symptoms. European Spine Journal 16 (2007): 1417-1422.
- Arantes Júnior AA, Silva Junior GA, Malheiros JA, et al. A new expansive two-open-doors laminoplasty for multilevel cervical spondylotic myelopathy: technical report and follow-up results. Arq Neuropsiquiatr 72 (2014): 49-54.
