Intraluminal Gist, A Rare Cause of Ileo-Ileal Intussusseption in an Elderly Male
Article Information
Muhammad Afzal Randhawa*, Saba Kaynat, Hafsa Niaz, Tehseen Shahzad
Department of Surgery, Bahawal Victoria Hospital, Quaid-E-Azam Medical College, Bahawalpur, Pakistan
*Corresponding Author: Muhammad Afzal Randhawa, Department of Surgery, Bahawal Victoria Hospital, Quaid-E-Azam Medical College, Bahawalpur, Pakistan
Received: 29 March 2018; Accepted: 06 April 2018; Published: 09 April 2018
Citation: Muhammad Afzal Randhawa, Saba Kaynat, Hafsa Niaz, Tehseen Shahzad. Intraluminal Gist, A Rare Cause of Ileo-Ileal Intussusseption in an Elderly Male. Archives of Clinical and Biomedical Research 2 (2018): 068-077.
View / Download Pdf Share at FacebookAbstract
Introduction: Gastrointestinal stromal tumors are mesenchymal tumors found in the stomach, jejunum and ileum and represent 9% of all small bowel tumors. Their intraluminal occurrence in the small bowel is a rare phenomenon as they predominantly grow extra-luminally, so rarely causing small bowel obstruction or intussusception. However, intraluminal presence can provide a lead point for intussusception as does the other benign and malignant diseases such as inflammatory bowel disease, post-op adhesions, crohn’s disease, Meckle’s diverticulum, Lipoma, lymphoma, adenocarcinoma, metastatic neoplasm or even presence of intestinal tubes. In adults only 8-20% cases of intussusceptions are idiopathic while the rest of cases are secondary to an underlying pathology. In elderly population most cases are of Ileo-colic type of intussusception secondary to malignant disease especially adenocarcinoma and lymphomas. However, there is no sufficient data available previously of intraluminal GIST causing ileo-ileal intussusception which makes our case worth presenting to literature.
Presentation: An elderly male patient of 67 years age presented with signs and symptoms of small bowel obstruction, weight loss and mild anemia. These symptoms started 3 months back and were slowly progressive. On examination he had a diffuse lower abdominal mass with signs of obstruction. Systemic examination was unremarkable and the patient had no co-morbid conditions. Exploratory laparotomy was carried out after radiological and baseline investigation and a diagnosis of intraluminal growth causing ileo-ileal intussusception confirmed. Primary anastomosis after resection of the involved segment done Histopathology showed GIST of low malignant potential with resection margins free of tumors and no lymph node involvement.
Discussion: CT-scan abdomen is investigation of choice to d
Keywords
Intussusception; Intraluminal; GIST; Small bowel; Ileo-ileal; Obstruction 1.
Article Details
1. Introduction
Neoplasms of the small bowel are rare lesions that account for less than 5% of all gastrointestinal tumors. Furthermore, Gastrointestinal stromal tumors are mesenchymal tumors and represent 9% of all small bowel tumors. These tumors most frequently occur in the stomach, followed by jejunum and ileum. Occurrence in colon, rectum, esophagus and the appendix is rare. GIST′s predominantly grow extra-luminally. An intraluminal mass is far less common. Obstruction and intussusception are rare because GISTs do not involve the circumferential bowel wall.
Intussusception of the bowel is defined as the telescoping of a proximal segment of the gastrointestinal tract within the lumen of the adjacent segment. This condition is frequent in children and presents with the classic triad of cramping abdominal pain, bloody diarrhea and a palpable tender mass. However, bowel intussusception in adults is considered a rare condition, accounting for 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction [1]. Eight to twenty percent of cases are idiopathic, without a lead point lesion. Secondary intussusception is caused by organic lesions, such as inflammatory bowel disease, postoperative adhesions, Meckel’s diverticulum, benign and malignant lesions, metastatic neoplasms or even iatrogenically, due to the presence of intestinal tubes, jejunostomy feeding tubes or after gastric surgery [2,3].
Intraluminal GIST causing small bowel intussusception is a rare clinical entity and could present as a diagnostic and management challenge for the surgeons. CT-scan is the most sensitive investigation and surgical resection is treatment of choice with proper oncological principals.
2. Presentation of Case
Our patient, an elderly male of 67 years age, who presented with symptoms of intestinal obstruction i.e. vomiting , constipation and abdominal distention. His symptoms first appeared 3 months ago, including colicky abdominal pain, off & on constipation, pain abdomen specially on oral intake, abdominal bloating and mild weight loss. These symptoms became more prominent with the passage of time. There was no history of fever, hematemesis, melena, fresh blood or mucous in stool and no other systemic symptoms.
On examination patient was mildly anemic with regular pulse rate and slightly dehydrated. Abdominal examination revealed moderate distention and a diffuse or ill defined mass in right lower abdomen. Bowel sounds were increased in frequency and tympanatic in character. On Digital rectal examination, rectum was empty. There was no significant lymphadenopathy and rest of systemic examination was unremarkable. Colonoscopy was normal (Figure 1).
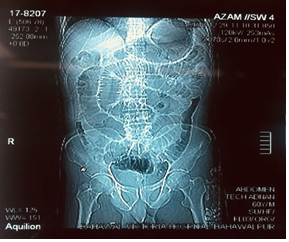
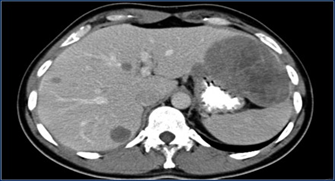
Erect X-ray abdomen showed significantly dilated small bowel loops with an abrupt cut off in distal small bowel. Stool occult blood test was negative. Urgent Abdominal CT-scan with contrast was obtained for definitive pre-op diagnosis which showed the findings of ileo-ileal intussusception secondary to intraluminal pathology (Figure 2).
A provisional diagnosis of intestinal obstruction secondary to small bowel pathology was made. Resuscitation of the patient was already started, nasogastric tube and Foley’s catheter passed, baseline investigation sent. CBC of the patient showed mild microcytic hypochromic anemia.
Exploratory laparotomy was done, which confirmed ileo-ileal intussusception, about one and a half feet segment of proximal ileum was involved. Involved segment was mildly inflamed and serosa thickened with proximal gut dilated (Figure 3).
This segment of gut was resected and an end to end anastomosis made with vicryl 2-0 in an interrupted fashion after emptying the gut on the table. Examination of resected specimen showed intraluminal 4 into 4 cm rounded firm soft tissue mass which was sub mucosal and served as lead point for intussusception. Surrounding mesentery of the lesion was fibrosed and mild serosal inflammation . There were no mesenteric lymph node enlargement and liver / spleen were normal. Also no ascetic fluid was present in the abdominal cavity. Proper closure of the abdomen was done without any drain. Skin sealed with fibrin glue (Figure 4).
The patient had his normal bowel function at 5th post-op day and was discharged. His follow-up is without any complications. Histopathology of the resected specimen showed diagnosis of gastrointestinal stromal tumor of low malignant potential with resected small bowel margins free of any disease and no lymph nodes involved. It was decided to add no further adjuvant treatment in this patient.
3. Discussion
First reported in 1674 by Barbette of Amsterdam [4] and further presented in a detailed report in 1789 by John Hunter [5] as “introssusception”, intussusception represents a rare form of bowel obstruction in the adult. Historically, Sir Jonathan Hutchinson was the first to operate on a child with intussusception in 1871 [6].
In adults, the exact mechanism of bowel intussusception is unknown (primary or idiopathic) in 8%-20% of cases and is more likely to occur in the small intestine [1, 7, 8]. On the other hand, secondary intussusception is believed to initiate from any pathologic lesion of the bowel wall or irritant within the lumen that alters normal peristaltic activity and serves as a lead point, which is able to initiate an invagination of one segment of the bowel into the other [7, 9]. Schematically, intussusception could be described as an “internal prolapse” of the proximal bowel with its mesenteric fold within the lumen of the adjacent distal bowel as a result of overzealous or impaired peristalsis, further obstructing the free passage of intestinal contents and, more severely, compromising the mesenteric vascular flow of the intussuscepted segment. The result is bowel obstruction and inflammatory changes ranging from thickening to ischemia of the bowel wall.
The clinical presentation of adult intussusception varies considerably. The presenting symptoms are nonspecific and the majority of cases in adults have been reported as chronic, consistent with partial obstruction [1, 10].
Variability in clinical presentation and imaging features often make the preoperative diagnosis of intussusception a challenging and difficult task. Reijnen et al [11] reported a preoperative diagnostic rate of 50%, while Eisen et al [12] reported a lower rate of 40.7%.
Plain abdominal films are typically the first diagnostic tool, since in most cases the obstructive symptoms dominate the clinical picture. Such films usually demonstrate signs of intestinal obstruction and may provide information regarding the site of obstruction [12, 13]. Upper gastrointestinal contrast series may show a “stacked coin” or “coil-spring” appearance, while a barium enema examination may be useful in patients with colo-colic or ileo-colic intussusception, during which a “cup-shaped” filling defect or “spiral” or “coil-spring” appearances are characteristically demonstrated [12, 14, 15].
Ultrasonography is considered a useful tool for the diagnosis of intussusception, both in children and in adults [16, 17]. The classical imaging features include the “target” or “doughnut” signs on the transverse view and the “pseudo-kidney” sign or “hay-fork” sign in the longitudinal view [17, 18]. Undoubtedly, this procedure requires handling and interpretation by an experienced radiologist, in order to confirm the diagnosis. However, obesity and the presence of massive air in the distended bowel loops limit the image quality and the subsequent diagnostic accuracy.
Abdominal computed tomography (CT) is currently considered as the most sensitive radiologic method to confirm intussusception, with a reported diagnostic accuracy of 58%-100% [4, 12, 19-23]. The characteristic features of CT scan include an un-homogeneous “target” or “sausage”- shaped soft- tissue mass with a layering effect,mesenteric vessels within the bowel lumen are also typical [7]. A CT scan may define the location, the nature of the mass, its relationship to surrounding tissues and, additionally, it may help staging the patient with suspected malignancy causing the intussusception [12].
Flexible endoscopy of the lower GI tract is considered invaluable in evaluating cases of intussusception presenting with sub-acute or chronic large bowel obstruction [7]. Confirmation of the intussusception, localization of the disease and demonstration of the underlying organic lesion serving as a lead point are the main benefits of endoscopy.
About 20-30% of GIST′s are malignant at presentation. In the small bowel they are more often malignant than in the stomach. Tumors smaller than 2 cm are usually benign, whereas masses larger than 5 cm are often malignant.
Malignant GIST′s predominantly grow extra-luminally and can show necrosis, hemorrhage, calcification (post therapy) and fistula formation. Typically a GIST is a well defined and exophytic mass with heterogeneous enhancement and a clear delineation from the mesentery.
An intraluminal mass is far less common. Obstruction is rare because GISTs do not involve the circumferential bowel wall, in contrast to adenocarcinoma. Unlike carcinoid tumors, the primary lesion in a GIST is large. Both GIST and lymphoma can show aneurysmal dilation of the bowel. Liver metastases are usually hyper-vascular and can be missed on a single portal venous phase CT.
Lymph node metastases are generally not seen. If lymphadenopathy is seen, you should consider another diagnosis. Mesenteric or omental metastases are more common in recurrent disease than at first presentation. This is thought to be due to spill of tumor during surgery. These metastases can be easily missed, as they often have a low-density center.
After chemotherapy (Imatinib or Gleevec), the liver and mesenteric metastases become hypo-vascular or even cystic. Despite radical surgical resection, 40-90% of patients have recurrence of disease in liver or mesentery. Gleevec can be given in case of metastatic disease. Disease recurrence in resected GIST showing hypo-dense liver metastases and a large heterogeneous peritoneal metastasis [24].
Due to the fact that adults present with acute, sub-acute, or chronic nonspecific symptoms [25], the initial diagnosis is missed or delayed and is established only when the patient is on the operating table. Most surgeons accept that adult intussusception requires surgical intervention because of the large proportion of structural anomalies and the high incidence of occurring malignancy. However, the extent of bowel resection and the manipulation of the intussuscepted bowel during reduction remain controversial [7]. In contrast to pediatric patients, where intussusception is primary and benign, preoperative reduction with barium or air is not suggested as a definite treatment for adults [7, 12, 26].
The theoretical risks of preliminary manipulation and reduction of an intussuscepted bowel include: (1) intraluminal seeding and venous tumor dissemination, (2) perforation and seeding of microorganisms and tumor cells to the peritoneal cavity and (3) increased risk of anastomotic complications of the manipulated friable and edematous bowel tissue [1, 7, 11, 12, 27]. Moreover, reduction should not be attempted if there are signs of inflammation or ischemia of the bowel wall [23]. Therefore, in patients with ileo-colic, ileo-cecal, colo-colic and ileo-ileal intussusceptions, especially those more than 60 years of age, due to the high incidence of bowel malignancy as the underlying etiologic factor, formal resections using appropriate oncologic techniques are recommended, with the construction of a primary anastomosis between healthy and viable tissue [7, 11, 12, 28-30]. Finally, several reports have been published regarding the laparoscopic approach of adult intussusception, due to benign and malignant lesions of the small and large bowel [31-35].
4. Conclusion
Surgery i.e. resection and primary end to end anastomosis is treatment of choice in adults in contrast to pediatric group where a trial of air/ barium enema or intra-operative reduction is preferred treatment for intussusception. Involved segment of bowel should not be reduced intra-operatively in such elderly patients to prevent theoretical risk of tumor cells spillage intra-luminally or intra-abdominally. Proper oncological principals must be followed. All abdominal viscera must be thoroughly inspected for metastatic deposits. Complete resection and reconstruction of involved bowel is sufficient treatment. In recurrent or metastatic disease, Imatinib and Gleevac are used as chemotherapeutic agents.
5. Statement of Ethics
The study was performed in accordance with the Helsinki Declaration and Good Clinical Practice.
6. Disclosure Statement
The authors have no conflicts of interest to disclose.
7. Consent of the Patient
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
8. Scare checklest
This work is prepared in guidance with SCARE checklist
References
- Azar T, Berger DL. Adult intussusception. Ann Surg 226 (1997): 134-138.
- Ishii M, Teramoto S, Yakabe M, Yamamato H, Yamaguchi Y, et al. Small intestinal intussusceptions caused by percutaneous endoscopic jejunostomy tube placement. J Am Geriatr Soc 55 (2007): 2093-2094.
- Archimandritis AJ, Hatzopoulos N, Hatzinikolaou P, Sougioultzis S, Kourtesas D, et al. Jejunogastric intussusception presented with hematemesis: a case presentation and review of the literature. BMC Gastroenterol 1: (2001) 1.
- de Moulin D, Paul Barbette. A seventeenth-century Amsterdam author of best-selling textbooks. Bull Hist Med 59 (1985): 506-514.
- Noble I. Master surgeon: John Hunter. J. Messner: New York (1971): 185.
- Hutchinson H, Hutchinson J. Jonathan Hutchinson, life and letters. 1st ed. Wm Heinemann Medical Books: London (1946).
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 173 (1997): 88-94.
- Erkan N, Haciyanli M, Yildirim M, Sayhan H, Vardar E, Polat AF. Intussusception in adults: an unusual and challenging condition for surgeons. Int J Colorectal Dis 20 (2005): 452-456.
- Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, et al. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol 36 (2003): 18-21.
- Martin-Lorenzo JG, Torralba-Martinez A, Liron-Ruiz R, Flores-Pastor B, Miguel-Perello J, et al. Intestinal invagination in adults: preoperative diagnosis and management. Int J Colorectal Dis 19 (2004): 68-72.
- Reijnen HA, Joosten HJ, de Boer HH. Diagnosis and treatment of adult intussusception. Am J Surg 158 (1989): 25-28.
- Eisen LK, Cunningham JD, Aufses AH Jr. Intussusception in adults: institutional review. J Am Coll Surg 188 (1999): 390-395.
- Cerro P, Magrini L, Porcari P, De Angelis O. Sonographic diagnosis of intussusceptions in adults. Abdom Imaging 25 (2000): 45-47.
- Zubaidi A, Al-Saif F, Silverman R. Adult intussusception: a retrospective review. Dis Colon Rectum 49 (2006): 1546-1551.
- Wiot JF, Spitz HB. Small bowel intussusception demonstrated by oral barium. Radiology 97 (1970): 361-366.
- Fujii Y, Taniguchi N, Itoh K. Intussusception induced by villous tumor of the colon: sonographic findings. J Clin Ultrasound 30 (2002): 48-51.
- Boyle MJ, Arkell LJ, Williams JT. Ultrasonic diagnosis of adult intussusception. Am J Gastroenterol 88 (1993): 617-618.
- Weissberg DL, Scheible W, Leopold GR. Ultrasonographic appearance of adult intussusception. Radiology 124 (1977): 791-792.
- Erbil Y, Eminoglu L, Calis A, Berber E. Ileocolic invagination in adult due to caecal carcinoma. Acta Chir Belg 97 (1997): 190-191.
- Farrokh D, Saadaoui H, Hainaux B. Contribution of imaging in intestinal intussusception in the adult. Apropos of a case of ileocolic intussusception secondary to cecal lipoma. Ann Radiol (Paris) 39 (1996): 213-216.
- Gayer G, Apter S, Hofmann C, Nass S, Amitai M, et al. Intussusception in adults: CT diagnosis. Clin Radiol 53 (1998): 53-57.
- Bar-Ziv J, Solomon A. Computed tomography in adult intussusception. Gastrointest Radiol 16 (1991): 264-266.
- Tan KY, Tan SM, Tan AG, Chen CY, Chng HC, et al. Adult intussusception: experience in Singapore. ANZ J Surg 73 (2003): 1044-1047.
- Sandrasegaran K, Rajesh A, Rydberg J, et al. Gastrointestinal stromal tumors: clinical , radiological and pathologic features. AJR 184 (2005): 803-811 .
- Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg 186 (2003): 75-76.
- Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, et al. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis 21 (2006): 834-839.
- Weilbaecher D, Bolin JA, Hearn D, Ogden W 2nd. Intussu-sception in adults. Review of 160 cases. Am J Surg 121 (1971): 531-535.
- Nagorney DM, Sarr MG, McIlrath DC. Surgical management of intussusception in the adult. Ann Surg 193 (1981): 230-236.
- Felix EL, Cohen MH, Bernstein AD, Schwartz JH. Adult intussusception; case report of recurrent intussusception and review of the literature. Am J Surg 131 (1976): 758-761.
- Wolff BC, Boller AM. Large bowel obstruction. In: JL Cameron., editor. Current surgical therapy. Mosby Elsevier: Philadelphia (2008): 189-192.
- Gonzalez AM, Clapp B. Laparoscopic management of small bowel intussusception in a 16-year-old with Peutz-Jeghers syndrome. JSLS 12 (2008): 332?334.
- Lin MW, Chen KH, Lin HF, Chen HA, Wu JM, Huang SH. Laparoscopy-assisted resection of ileoileal intussusception caused by intestinal lipoma. J Laparoendosc Adv Surg Tech A 17 (2007): 789-792.
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Minimal access surgery for adult intussusception with subacute intestinal obstruction: a single center′s decade-long experience. Surg Laparosc Endosc Percutan Tech 17 (2007): 487-491.
- Chuang Ch, Hsieh C, Lin Ch, Yu J. Laparoscopic man-agement of sigmoid colon intussusception caused by a malignant tumor: case report. Rev Esp Enferm Dig 99 (2007): 615-616.
- Ishibashi Y, Yamamoto S, Yamada Y, Fujita S, Akasu T, et al. Laparoscopic resection for malignant lymphoma of the ileum causing ileocecal intussusception. Surg Laparosc Endosc Percutan Tech 17 (2007): 444-446.