Incident of Post ERCP Complications: Meta-analysis and Systematic Review
Article Information
Mohamed Dahir Aden*, Tao Deng, Liao Yuting
Department of Gastroenterology, Renmin Hospital of Wuhan University, Hubei, Wuhan, China
*Corresponding Authors: Mohamed Dahir Aden, Department of Gastroenterology, Renmin Hospital of Wuhan University, Hubei, Wuhan, China
Received: 29 June 2020; Accepted: 10 July 2020; Published: 17 July 2020
Citation:
Mohamed Dahir Aden, Tao Deng, Liao Yuting. Incident of Post ERCP Complications: Meta-analysis and Systematic Review. Archives of Internal Medicine Research 3 (2020): 168-177.
View / Download Pdf Share at FacebookAbstract
Background: Post-endoscopic retrograde cholangio-pancreatography (ERCP) primarily exhaust certain complications in the diagnostic assessment of therapeutics of pancreatitis in a multi-variant incidence. And in identifying the rate of fatalities and severity, we determine PEP mortality based on placebo randomized controlled trials to subsequently evaluate precise diagnostic ways.
Method: The database of systematic reviews was searched from EMBASE, MEDLINE, Springer and Cochrane database performing >15 reviewing clinical studies in the measures of 10 years, probably selecting the survey of prospective cited literature with relevant references independently extract the sensitivity following association of perforations, infection, bleeding and miscellaneous outcome of pancreatitis. The discrepancies of cohort studies across geographical regions identified 450 articles expressing the dichotomous outcome of the odds ratio (OR) comparing with the Randomized controlled trial (RCT) conducted previously since 2009 reporting the cases of PEP 10% and mortality rate 1.0% respectively.
Conclusion: The limitation of study always remains on PEP included risk factors in matches of gender differences at overall procedures of Oddi sphincter dysfunctions inducing sphincterotomy and pancreatic duct stenting in non-prophylactic ways relative to the consistency of morbidity carrier which triggers the events of severity leading to death cause.
Keywords
Pancreatitis, Sphincterotomy, Stenting
Pancreatitis articles, Sphincterotomy articles, Stenting articles
Article Details
1. Introduction
ERCP always has chosen to treat pancreatitis over various diagnostic procedures evolving post-operative conditions from invasive development of MRCP in the therapeutic intervention of biliary disorders. The main direction is to review the screening of 13 studies trials in females clinically at more frequent ways, essentially to see the thermal effect and certain blockages leading to tissue sensitivity causing PEP. Moreover, the estimated incidence of approximately 100,000 in the US annually assumed the impact of risk factors over >36,000 cases, preferring MRCP a better diagnostic way as compared with ERCP in a prolonged helpless hospitalized scenario roughly to treat iatrogenic reports. However, the question always arises from retrospective studies based on intervening results specificity that the potency of ERCP promptly of higher levels resolve the magnitude of life-threatening complications pursuing to minimize the fatalities cases [1-3]. The expanded post-operative risk factors include the frequent bleeding, infection, hemorrhage, and perforation that may remain a concern of controversy in protective measures of preventive consenting the patient’s accuracy of diagnostics. As mentioned in the several literature reviews about the suffered incidence based on severity and mortality rate include the involvement of certain post ERCP risk factors to some extend comprehensively summarize through collected data based on RCTs [2-4]. The evaluation of incidence adopts a similar result of 0.5% carrying out the earlier noted ERCP survey estimating RCTs follow-up. Furthermore, the attributed criteria of comorbidities systematically trigger the autoimmune and neoplastic conditions elucidating the correlated factors interacting with the synergies of PEP complications greatly vary the values depending on effectiveness and particular geographic regions [5]. The main aim of the study based on prospective studies is to truly determine the number of targeted cases indicating the calculated techniques for the efficacy of safety prevention in the guidelines of post ERCP stratifying
risk factors excluding the stenting therapy outcome.
2. Methods
2.1 Data strategy
Literature search clinically carried out between 2009-2019 in MEDLINE and Cochrane to outline the guidelines of research quality and methods in accordance with combined searched on Embase and PubMed in terms of keywords identifying the efficacy of treatment in RCTs to prevent pancreatitis. The relevant search of bibliographies from systematic reviews of Annals of Internal Medicine, Gastrointestinal endoscopy, Gout, Endoscopy, and New England Journal of Medicine publications during 2012-2019 was also observed in the collection of additional data for inclusion criteria.
2.2 Eligibility
The evidence-based results conducting stents can be possibly prevented to reduce the formation of PEP.
2.3 Data extraction
The basic approach in the diagnostic analysis of treatment for mention the importance of ERCP needs to exclude prophylaxis. The full review content reveals the comments of independent 2 reviewers defining the staging of consensus factors that remain eligible for resolving the ability to subtract dates. And the quality of generated randomized sequence allocates the investigations on using pilot-tested data, adding on variable sheets about its characteristic outcomes.
2.4 Identified criteria
Inclusion: The primary analysis of multivariate data past 10 years in the observed study shows the complexity of pancreatitis on the least of 3-fold higher amylase concentration in the period of first 24hrs during post ERCP accompanying fewer milder symptoms obtaining the reliability of explanation.
2.5 Exclusion
The case study reports and reviews were the types of articles clarifying the size of the study used on 150 cases for an OR value of 95% Confidence Interval. And the studies with less known facts and etiology retrospective data were also to elaborate the result and conclusion on not duplicating results.
2.6 Analysis
The pool incidence obtaining the proportions of inverse-weighted variance brings out the negative effect on post ERCP use indicating ERCP non-risky stratify in some continents on measuring n value. The consideration of PEP assessment suspecting SOD reports the balanced compared result in a sufficient amount of study that increases the absolute risk at the developmental staging. However, the performance of meta-analysis in the minimized capabilities allowed to estimate bias by stata 11.1 software to notice the inherent of secondary results at the recognition of statistics specifying the portion of the random errors portion through each RCTs. The expressed data in an analytical way define the dichotomous calculation with deemed statistical differences of P-value <0.05 on using the RevMan version. 4.3 in a collaborated review manager.
3. Result
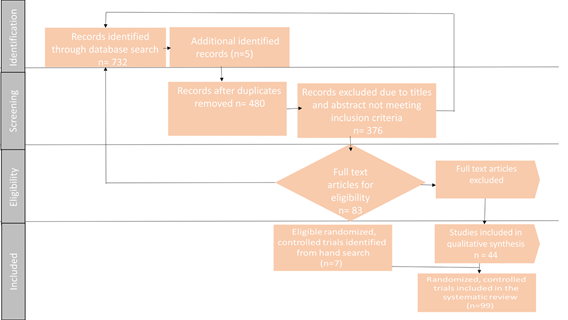
The involved Post ERCP 19 cases in the review with 55 (0.03%) fatalities, 282 (1.677%) severe complications and 173 (1.33%) total PEP suffering incidence of 1.13-1.53 we extracted the relative risk on age group, gender, miscellaneous, and all death 0.02-0.12 CI using references to analyze the significance of P<0.01. On using adopted the Figure 1 in a search of PUBMED database 8 Cochrane library following 732 studies criteria relevant to 5 included ERCP on Endnote results checking the duplicating studies 480. The 376 total studies were found and removed through the search. The 83 studies in the eligibility screening measured the abstract and title with regards to criteria format. At this stage, the author added RCTs and exclude other types of publications adding case study, retrospective analysis, protocols, and editorial letters. The excluded 44 studies were not meeting the required inclusion submission. Therefore, the 99 studies were thoroughly reviewed, and out of 7 studies remained irrelevant. Thus the remaining 99 studies were assessed in the literature review. It mainly focusses on a different ways of procedures used in pancreatitis is known factors at certain peak points crucially in the probability of treatment and prevention therapy emphasizing the significance of analyzing through prospective studies. The quality of methodologies accordingly varies by 4 known severity conditions which quantitatively trigger towards the stone formation and sphincter of Oddi dysfunctions. The interchangeable results addressing the modifications in the distal parts fail to describe the ERCP procedure on justifying the confirmed best strategy in terms of switching the procedural actions in a feasible presence of complications i.e. pancreatic head tumor finding the papillary cause in OR 3.3 respectively. The primary identified findings in the assessment of pancreatic imaging and magnetic resonance cholangiopancreatography, history of the disease, and multiple dysfunctions [24-27].
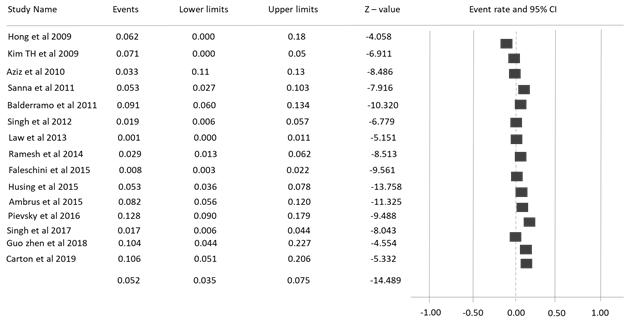
On studying further 6 reporting cases in the control study of PEP at on increased incidence of interval statistically 2 fold with P-value <0.01 deriving the endoscopic sphincterotomy result, 5.52% between 9 other studies evaluating RCTs measures shown in Figure 2 [25]. However, the adverse events in pancreatitis show fewer alterations during mechanical etiology explaining the funnel plot on observing 80% heterogeneity assumed by random effect with deriving complications of dilatation reaching the goal of predictive prophylaxis [28-32].
Table 1: Number of selective incidence in the surveys of post ERCP risk factors define prospective studies through different diagnostic techniques in brief review papers.
Table 2: Details of understanding subgroups concerning severity in Post ERCP.
The conventional outcomes maximize the anchoring devices in its performances of 5 trials effectively convince the use of cannulation modulates in edema and regressed tissue conditions to exhibit and proliferate ductal injection diagnostic way in prosthetic techniques observing retrograde efflux. Additionally, bleeding appears impaired requiring amylase noted levels for treating pancreatic pain. And the less spontaneous frequency based on a few symptoms contrasts retroperitoneal spacing, perforation, and luminous imaging influencing the pathology and prominence of the structure. Statistically, the 2-step forward approach in the parameters of stenosis sampling and diameter of biliary duct introduce an ERCP methodology to achieve the optimal not exceeding the moderate adverse events to severe pre-cut procedures in a clinical logistics.
4. Discussion
The innovation of endoscopy motivates various technologies to gather PEP investigating approaches to understand advance and conflict of interests in reviewing the literature and data on updated supported evidence. The smaller studies in the probability of cannulation localizing the main ductal system assure the reduced risk ratio of calcification and may facilitate the inhibitory action on a cascade of spasmodic secretion as a pharmaco prevention therapy [33, 34]. Whereas, the larger multicenter trials based on the hypothesis of standardized performances in the consensus of sphincterotomy incorporate the stone removal theory towards arsenal management tracking the limitations appeared and explored the interpretation for future concerning trials. According to the abstract based format in the importance of 3 published papers accepting the burden of sphincterotomy support the absolute results of pancreatitis events, analyzing the isolated sphincterotomy judging mechanical physiology exposing an infection in post-operative conditions [28-32]. The cautious attitude towards controlling the complexity events may monitor the interval time and occurrence of hemorrhage as a rare condition with perforation efficiently resolve the complementation exposed to ductal injury, trauma, and inflammation potentially noting the time required and its management. However, the episodic complaints of abdominal pain and fever functionally may variate the abnormalities in the incidence of drainage and stent placement showing the cohort studies largely confirm the continuum with biopsy, manometry, and needle diagnostic was simply to show the endoscopists experts the main purpose by consent from patients and an appropriate conclusion for future direction [35-37].
The multicenter EPISODIC predicts the dysfunction of Oddi sphincter in a beneficial way to rename the facet of SOD in separated sample size, subgroup, weighted events, and inheritance of missing data, confounding the adjustments in observing the partial and complete sphincterotomy transverse to the discrepancy of etiological circumstances. And, the selected 25 trials in its consistency of risk factors of coagulopathy and insufficient guidelines may exceptionally configure the rigorous tendency of the homogenized conceptual pathway [33]. Therefore, the remarkable review landmark the interest to the attempts of balloon dilatation in a disproportion of giant bile duct stones affecting 80% inversely suggesting the risk factors of choledocholithiasis prioritized in the aforementioned study resulting traumatic cases over sphincterotomy techniques. Thus, the absence of variance in substantial findings of analyzing bias expressed the quality of the study, case characteristics, and diversifying techniques but lack the changes in potency accordance with post ERCP complications for suitable proficiency training during pre-operative and intra-operative practices of analogs to minimize the post-operative harming conditions [38-40].
5. Conclusion
Despite, the known implications in the measures of pancreatitis at the trial of ERCP versus sphincterotomy its pharmacological study in its frequency include hydration, cannulation, spasmodic relief, inhibitory trypsinogen activating prophylaxis to average the multifactorial consolidate cases imprecision the pooling effect in terms of disputed PEP pathophysiological phases encountering the wire-guided technology as a final preventive measure.
Conflict of Interest
No competing interests.
References
- Hori Y, Naitoh I, Nakazawa T, Hayashi K, Miyabe K, et al. Feasibility of endoscopic retrograde cholangiopancreatography-related procedures in hemodialysis patients. J Gastroenterol Hepatol 29 (2014): 648-652.
- Colton JB, Curran CC. Quality indicators, including complications, of ERCP in a community setting: a prospective study. Gastrointest Endosc 70 (2009): 457-467.
- Cotton PB, Garrow DA, Gallagher J, Romagnuolo J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest Endosc 70 (2009): 80-88.
- Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, et al. Complications of ERCP. Gastrointest Endosc 75 (2012): 467-473.
- Cooper ST, Slivka A. Incidence, risk factors and prevention of post ERCP pancreatitis. Gastroenterol Clin North Am 36 (2007): 259-276.
- Hiroyuki Matsubayashi, Akira Fukutomi, Hideyuki Kanemoto, Atsuyuki Maeda, Kazuya Matsunaga, et al. Risk of pancreatitis after endoscopic retrograde cholangiopancreatography and endoscopic biliary drainage 11 (2009): 222-228.
- Peter B Cotton, Donald A Garrow, Joseph Gallagher, Joseph Romagnuolo. Risk Factors for Complications After ERCP: A Multivariate Analysis of 11,497 Procedures Over 12 Years. Gastrointest Endosc 70 (2009): 80-88.
- Pier Alberto Testoni. Risk Factors for post-ERCP Pancreatitis in High- And Low-Volume Centers and Among Expert and Non-Expert Operators: A Prospective Multicenter Study. Am J Gastroenterol 105 (2010): 1753-1761.
- Pancreatitis: Medical and Surgical Management (2010).
- Wence Zhou, Yumin Li, Quanbao Zhang, Xun Li, Wenbo Meng, et al. Risk Factors for Postendoscopic Retrograde Cholangiopancreatography Pancreatitis: A Retrospective Analysis of 7,168 Cases. Pancreatology 11 (2011): 399-405.
- Anderson MA. Complications in ERCP. Gastrointestinal Endoscopy 75 (2012): 467-473.
- Iorgulescu A, Sandu I, Turcu F, Iordache N. Post-ERCP Acute Pancreatitis and Its Risk Factors. J Med Life 6 (2013): 109-113.
- Xiang Ding, FuCheng Zhang, YaoJun Wang. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surgeon 13 (2015): 218-229.
- Kei Ito, Jun Horaguchi, Naotaka Fujita, Yutaka Noda, Go Kobayashi, et al. Clinical usefulness of double-guidewire technique for difficult biliary cannulation in endoscopic retrograde cholangiopancreatography. Digestive Endoscopy 26 (2014): 442-449.
- Kazunari Nakahara, Chiaki Okuse, Keigo Suetani, Yosuke Michikawa, Shinjiro Kobayashi, et al. Need for pancreatic stenting after sphincterotomy in patients with difficult cannulation. World J Gastroenterol 20 (2014): 8617-8623.
- Deshpande Aparna, Velhal Rishikesh, Thanky Harsh, Soman Sundeep, Shah Ritesh. Lessons Learnt in Management of Acute Pancreatitis. Journal of pancreas 16 (2015): 432-437.
- Mohammad Yaghoobi, Qi Pauls, Valerie Durkalski, Joseph Romagnuolo, Evan L Fogel, et al. Incidence and Predictors of post-ERCP Pancreatitis in Patients With Suspected Sphincter of Oddi Dysfunction Undergoing Biliary or Dual Sphincterotomy: Results From the EPISOD Prospective Multicenter Randomized Sham-Controlled Study. Endoscopy 47 (2015): 884-890.
- David Zagalsky, Martín Guidi, Cecilia Curvale, Juan Lasa, Julio de María, et al. Early Precut Is as Efficient as Pancreatic Stent in Preventing post-ERCP Pancreatitis in High-Risk Subjects-A Randomized Study. Rev Esp Enferm Dig 108 (2016): 258-562.
- Parth J Parekh, Raj Majithia, Sanjay K Sikka, Todd H Baron. The “Scope” of Post-ERCP Pancreatitis. Mayo Clin Proc 92 (2017): 434-448.
- Hiroyuki Miyatani, Hirosato Mashima, Masanari Sekine, Satohiro Matsumoto. Post-ERCP biliary complications in patients with biliary type sphincter of Oddi dysfunction. Sci Rep 8 (2018).
- Milan S Bassan, Praka Sundaralingam, Scott B Fanning, James Lau, Jayaram Menon, et al. The Impact of Wire Caliber on ERCP Outcomes: A Multicenter Randomized Controlled Trial of 0.025-inch and 0.035-inch Guidewires. Gastrointest Endosc 87 (2018): 1454-1460.
- Qiang Huang, Feng Shao, Chen Wang, Wei Qi, Lu Jun Qiu, et al. Nasobiliary drainage can reduce the incidence of post-ERCP pancreatitis after papillary large balloon dilation plus endoscopic biliary sphincterotomy: a randomized controlled trial. Scandinavian Journal of Gastroenterology 53 (2018): 114-119.
- Murat Pekgöz. Post-endoscopic retrograde cholangiopancreatography pancreatitis: A systematic review for prevention and treatment. World J Gastroenterol 25 (2019): 4019-4042.
- Wang P, Li ZS, Liu F, Ren X, Lu NH, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol 104 (2009): 31-40.
- DiMagno MJ, Spaete JP, Ballard DD, Wamsteker EJ, Saini SD. Risk models for post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP): smoking and chronic liver disease are predictors of protection against PEP. Pancreas 42 (2013): 996-1003.
- Lin Y, Liu X, Cao DQ, Tang JH, Wen JJ, et al. Analysis of risk factors and prevention strategies of post-ERCP pancreatitis. Eur Rev Med Pharmacol Sci 21 (2017): 5185-5190.
- Omar M, Ahmed A, Said O, El-Amin H. Risk factors for post-ERCP pancreatitis: a prospective multicenter study in upper Egypt. Egypt J Surg 34 (2015): 1-10.
- Cotton PB. ERCP: Risks, Prevention, and Management. In: Cotton PB, Leung J, editors. Advances Digestive Endoscopy: ERCP. Massachusetts: Blackwell Publishing (2005): 339-403.
- Karsenti D, Coron E, Vanbiervliet G, Privat J, Kull E, et al. Complete endoscopic sphincterotomy with vs. without large-balloon dilation for the removal of large bile duct stones: randomized multicenter study. Endoscopy 49 (2017): 968-976.
- Guo Y, Lei S, Gong W, Gu H, Li M, et al. A Preliminary Comparison of Endoscopic Sphincterotomy, Endoscopic Papillary Large Balloon Dilation, and Combination of the Two in Endoscopic Choledocholithiasis Treatment. Med Sci Monit 21 (2015): 2607-2612.
- Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, et al. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology 144 (2013): 341-345.
- Jun Bo Q, Li Hua X, Tian Min C, Liu Gen G, Yan Mei Y, et al. Small Endoscopic Sphincterotomy plus Large-Balloon Dilation for Removal of Large Common Bile Duct Stones during ERCP. Pak J Med Sci 29 (2013): 907-912.
- Elmunzer BJ. Reducing the risk of post-endoscopic retrograde cholangiopan-creatography pancreatitis. Dig Endosc 29 (2017): 749-757.
- Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc 54 (2001): 425-434.
- Wilcox CM, Phadnis M, Varadarajulu S. Biliary stent placement is associated with post-ERCP pancreatitis. Gastrointest Endosc 72 (2010): 546-550.
- Zhou W, Li Y, Zhang Q, Li X, Meng W, et al. Risk factors for postendoscopic retrograde cholangiopancreatography pancreatitis: a retrospective analysis of 7,168 cases. Pancreatology 11 (2011): 399-405.
- Akashi R, Kiyozumi T, Tanaka T, Sakurai K, Oda Y, et al. Mechanism of pancreatitis caused by ERCP. Gastrointest Endosc 55 (2002): 50-54.
- Choudhary A, Bechtold ML, Arif M, Szary NM, Puli SR, et al. Pancreatic stents for prophylaxis against post-ERCP pancreatitis: a meta-analysis and systematic review. Gastrointest Endosc 73 (2011): 275-282.
- Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol 102 (2007): 1781-1788.
- Masci E, Mariani A, Curioni S, Testoni PA. Risk factors for pancreatitis following endoscopic retrograde cholangiopancreatography: a meta-analysis. Endoscopy 35 (2003): 830-834.