Fertility Outcomes After Varicocele Repair: Are There Any Benefits? A Traditional Review
Article Information
Iana Malasevskaia1*, Ahmed Ali Al-Awadhi2, Fatima Ali Raza3
1Clinic of Obstetrics and Gynecology, Yemen-German Hospital, Sana'a, Republic of Yemen
2Yemen-German Hospital, Sana’a, Republic of Yemen
3MBBS Student, Karachi Medical and Dental College, Karachi, Pakistan
*Corresponding Author: Iana Malasevskaia, Clinic of Obstetrics and Gynecology, Yemen-German Hospital, Sana'a, Republic of Yemen
Received: 20 March 2021; Accepted: 03 April 2021; Published: 06 April 2021
Citation: Iana Malasevskaia, Ahmed Ali Al-Awadhi, Fatima Ali Raza. Fertility Outcomes After Varicocele Repair: Are There Any Benefits? A Traditional Review. Fortune Journal of Health Sciences 4 (2021): 284-298.
View / Download Pdf Share at FacebookAbstract
Backgrounds: A varicocele is identified in 15% of healthy men and around 40% of men with primary infertility suffer from some degree of varicocele. The presence of spermatic varicose veins creates a hostile environment for spermatogenesis. It results in reduced quality and quantity of sperm production and, in some cases, can conduce to a total absence of sperm. This is due to an increase in circulating reactive oxygen species (ROS) resulting in sperm DNA fragmentation, even if the conventional semen parameters are within the normal reference ranges. It has been proposed that treating the varicocele may result in improvements in the semen parameters, fertilization, and pregnancy rates. Additionally, treating the varicocele could improve the results of both spontaneous pregnancies as well as following in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and Assisted Reproduction Treatment (ART) in the presence of suboptimal semen parameters.
Aim: We are performing a review of the literature with the aim to evaluate the evidence of the indications and advantages of treatment of varicocele in infertile men. And additionally, we are analyzing the results achieved after the varicocele repair.
Methods: A literature search in PMC, PubMed, Google, and Google Scholar was carried out using the following keywords: ”varicocele”, “varicocelectomy”, “male infertility”, “varicocelectomy and fertility outcome”. Study selection was in the language (English only), model (humans only), open accesses, and all types of studies were included as long as they were relevant to our study.
Limitations: While we were gathering the information for this review, there were some limitations. Our data was primarily obtained from articles with free full access and written in English language only; thus, relevant articles of closed acces
Keywords
Male infertility; Varicocele; ART; ICSI; IVF; Asthenozoospermia; Oligozoospermia; Varicocelectomy
Male infertility articles; Varicocele articles; ART articles; ICSI articles; IVF articles; Asthenozoospermia articles; Oligozoospermia; Varicocelectomy articles, Male infertility articles Male infertility Research articles Male infertility review articles Male infertility PubMed articles Male infertility PubMed Central articles Male infertility 2023 articles Male infertility 2024 articles Male infertility Scopus articles Male infertility impact factor journals Male infertility Scopus journals Male infertility PubMed journals Male infertility medical journals Male infertility free journals Male infertility best journals Male infertility top journals Male infertility free medical journals Male infertility famous journals Male infertility Google Scholar indexed journals Varicocele articles Varicocele Research articles Varicocele review articles Varicocele PubMed articles Varicocele PubMed Central articles Varicocele 2023 articles Varicocele 2024 articles Varicocele Scopus articles Varicocele impact factor journals Varicocele Scopus journals Varicocele PubMed journals Varicocele medical journals Varicocele free journals Varicocele best journals Varicocele top journals Varicocele free medical journals Varicocele famous journals Varicocele Google Scholar indexed journals ART articles ART Research articles ART review articles ART PubMed articles ART PubMed Central articles ART 2023 articles ART 2024 articles ART Scopus articles ART impact factor journals ART Scopus journals ART PubMed journals ART medical journals ART free journals ART best journals ART top journals ART free medical journals ART famous journals ART Google Scholar indexed journals ICSI articles ICSI Research articles ICSI review articles ICSI PubMed articles ICSI PubMed Central articles ICSI 2023 articles ICSI 2024 articles ICSI Scopus articles ICSI impact factor journals ICSI Scopus journals ICSI PubMed journals ICSI medical journals ICSI free journals ICSI best journals ICSI top journals ICSI free medical journals ICSI famous journals ICSI Google Scholar indexed journals IVF articles IVF Research articles IVF review articles IVF PubMed articles IVF PubMed Central articles IVF 2023 articles IVF 2024 articles IVF Scopus articles IVF impact factor journals IVF Scopus journals IVF PubMed journals IVF medical journals IVF free journals IVF best journals IVF top journals IVF free medical journals IVF famous journals IVF Google Scholar indexed journals Asthenozoospermia articles Asthenozoospermia Research articles Asthenozoospermia review articles Asthenozoospermia PubMed articles Asthenozoospermia PubMed Central articles Asthenozoospermia 2023 articles Asthenozoospermia 2024 articles Asthenozoospermia Scopus articles Asthenozoospermia impact factor journals Asthenozoospermia Scopus journals Asthenozoospermia PubMed journals Asthenozoospermia medical journals Asthenozoospermia free journals Asthenozoospermia best journals Asthenozoospermia top journals Asthenozoospermia free medical journals Asthenozoospermia famous journals Asthenozoospermia Google Scholar indexed journals Oligozoospermia articles Oligozoospermia Research articles Oligozoospermia review articles Oligozoospermia PubMed articles Oligozoospermia PubMed Central articles Oligozoospermia 2023 articles Oligozoospermia 2024 articles Oligozoospermia Scopus articles Oligozoospermia impact factor journals Oligozoospermia Scopus journals Oligozoospermia PubMed journals Oligozoospermia medical journals Oligozoospermia free journals Oligozoospermia best journals Oligozoospermia top journals Oligozoospermia free medical journals Oligozoospermia famous journals Oligozoospermia Google Scholar indexed journals Varicocelectomy articles Varicocelectomy Research articles Varicocelectomy review articles Varicocelectomy PubMed articles Varicocelectomy PubMed Central articles Varicocelectomy 2023 articles Varicocelectomy 2024 articles Varicocelectomy Scopus articles Varicocelectomy impact factor journals Varicocelectomy Scopus journals Varicocelectomy PubMed journals Varicocelectomy medical journals Varicocelectomy free journals Varicocelectomy best journals Varicocelectomy top journals Varicocelectomy free medical journals Varicocelectomy famous journals Varicocelectomy Google Scholar indexed journals
Article Details
Introduction & Background
In” De Medicina,” written by Celsus during the first century AD, credited the Greeks with the first description of a varicocele and recorded his astute observation: “The veins are swollen and twisted over the testicle, which becomes smaller than its fellow, in as much as its nutrition has become defective” [1].
Varicocele is found in about one in six males, and it is more common in younger males aged 15-25. Varicocele is usually harmless but can be associated with infertility problems by contributing to low sperm production and decreased sperm quality. While approximately 15% of men have a varicocele, about 40% have a varicocele in at least one testicle among men evaluated for infertility. Surgical repair of varicocele can restore fertility when this is the source of the problem [2]. The association between varicoceles and male infertility is undeniable, and this problem was first noted in the late 1800s by British surgeon Barfield and was subsequently confirmed by others in the early 1900s [3].
What is a varicocele?
Varicocele: Elongation and enlargement of veins within the veins (pampiniform plexus) that leave the testis to form the testicular vein. A varicocele appears bluish through the scrotum, can cause pain or discomfort, and feels like a bag of worms [4].
What causes a varicocele to develop?
The etiology of varicocele still remains arguable, with the involvement of factors like congenital/anatomical abnormalities, the presence of anti-sperm antibodies, and reflux of spermatic venous blood [5].
Varicoceles are more common (80% to 90%) in the left testicle, and if a left varicocele is identified, there is a 30% to 40% possibility that it is a bilateral condition [3]. As shown below in the Table 1, there are some anatomical theories involved in varicocele formation.
There are three theories as to the anatomical cause:
|
Theories as to the anatomical cause of a varicocele [3] |
|
|
1 |
When the left internal spermatic vein gets caught between the superior mesenteric artery and the aorta, the "Nutcracker" effect occurs. Due to entrapment which causes venous compression, spermatic vein obstruction develops. |
|
2 |
Where the internal spermatic vein joins the left renal vein, a failure of the anti-reflux valve can occur. This failure causes reflux and retrograde flow in the testicular vein. |
|
3 |
Angulation at the junction of the left renal vein and the left internal spermatic vein. |
Table 1: The anatomical theories which can be involved in the pathology of a varicocele.
Rare causes of varicoceles include renal arteriovenous malformations, deep vein thrombosis, and thrombosis of the pampiniform plexus [3]. Tobacco smoking and mutations in the gene expressing glutathione S-transferase Mu 1 increase the risk of male infertility. These factors may also increase the risk for a varicocele [3].
The varicocele causes a "stress pattern" on microscopic semen examination. This pattern consists of a low sperm count, poor motility, and an increase in the percentage of abnormal sperm [3]. Figure 1, summarize the causes which are proposed to be involved in a varicocele formation.
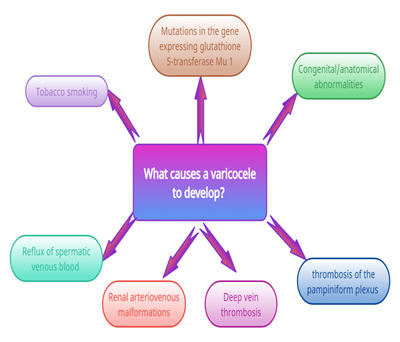
Figure 1: Leading causes involved in a varicocele formation.
Possible signs and symptoms of a varicocele
A varicocele is a collection of veins that are enlarged and often look or feel like a bag of worms. Usually – 85% of the time – due to the position of the veins on the left side, varicoceles develop mostly on the left. A varicocele is associated with an uncomfortable, dull ache pain in the scrotum and worse after prolonged or strenuous exercise. Lying down can ease the blood drain from the scrotum, thus relieving pain. Varicocele may affect sperm production, motility and can interfere with the actual production of testosterone, leading to male factor infertility. Additionally, the varicocele can cause an inability to get a firm erection, low sex drive, fatigue or lack of energy, lack of ambition, difficulty sleeping, trouble concentrating, decreased exercise tolerance, hot flashes, decreased muscle mass, and increased fat mass. In fact, varicoceles are a major cause of problems in four out of 10 men experiencing infertility issues [6].
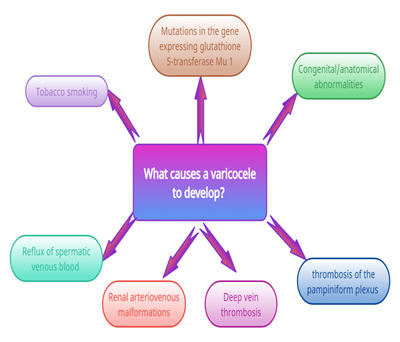
Figure 2: Signs and symptoms of a varicocele
Methods of treatment for varicoceles
Varicocele treatment might not be always necessary. Many patients with varicoceles are able to father a child without any treatment. However, if a varicocele causes pain, testicular atrophy or infertility, the patient might undergo a varicocele repair [7].
Repair methods include: open surgery, laparoscopic surgery, and percutaneous embolization.
Open surgery- During a general or local anesthetic on an outpatient basis, the surgeon will approach the vein through the groin (inguinal or sub-inguinal) or by an incision in the abdomen or below the groin. Open surgery using a microscope and sub-inguinal approach has the highest success rates when compared with other surgical methods [7].
Laparoscopic surgery- The surgeon makes a small incision under general anesthesia in the abdomen and passes a tiny instrument through the incision to see and to repair the varicocele [7].
Percutaneous embolization- A tube is inserted into a vein in the groin or neck through which instruments can be passed. Enlarged veins are blocked with a solution that causes scarring of the testicular veins, which interrupts the blood flow and repairs the varicocele. However, this procedure isn't as widely used as surgery [7]. If the patient has a varicocele that causes minor discomfort but doesn't affect his fertility, he might try over-the-counter painkillers, such as acetaminophen or ibuprofen. Wearing an athletic supporter to relieve the pressure is also advised [7].
Discussion
As described above, percutaneous embolization, microsurgical varicocelectomy, laparoscopic varicocelectomy are the main treatment options for varicoceles in infertile men. The main goal of treatment is to eliminate venous backflow [8].
Vermeulen and Vandeweghe compared fertility after varicocele correction by embolization of the vena spermatica in 62 subjects with infertility and untreated group (n = 20) of patients with varicocele. One year after varicocele repair of males with asthenozoospermia, oligozoospermia, teratozoospermia but normal follicle-stimulating hormone (FSH) levels, 15 of 62 had achieved a pregnancy; however, in the untreated group, eight had achieved a pregnancy. Varicocele correction showed only a slight improvement of sperm quality; the severity of varicocele had no influence either on sperm characteristics or on the outcome of treatment [9].
Ashkenazi et al. assessed the impact of spermatic vein ligation on the male factor infertility in vitro fertilization-embryo transfer (IVF-ET) and its relation to testosterone levels before and after the operation. Twenty-two couples participated in the study; group I consisted of 12 couples with mechanical female infertility, and group II of 10 with normal female fertility, in whom the male had subfertile semen in the presence of varicocele and had failed preoperative IVF-ET attempts. They were readmitted for the IVF-ET procedure following the repair of varicocele. In the group I, a 20% pregnancy rate was achieved after the operation, while in group II, four pregnancies (40%) were achieved after the operation. Plasma testosterone (T) levels significantly increased in 50% of the patients of both groups after surgery, resulting in concurrently improved fertilization, cleavage, and pregnancy rates [10].
Yamamoto et al. assessed whether subclinical varicocele ligation improves fertility and/or semen parameters. A total of 85 patients with a subclinical varicocele participated in a randomized prospective controlled study. Patients were randomly assigned to groups I (high ligation of the internal spermatic vein) and II (followed without any treatment). The pregnancy rate in group I was 6.7% compared to 10% in group II, and the difference was not statistically significant. Group, I had significantly higher levels of sperm density and total motile sperm count at one year. There were no significant differences between groups I and II regarding a change in seminal volume, sperm motility, and abnormal sperm morphology [11].
Grasso et al. evaluate the effect of spermatic vein ligation in patients over 30 years old and with low-grade left varicocele. In a randomized clinical trial participated 68 infertile patients of 30-38 years old with sperm abnormalities and had low-grade varicocele (grade I according to Hirsch), comparing left spermatic vein ligation with no treatment. However, there was no improvement in sperm quality after left spermatic vein ligation for low-grade varicocele in both groups one year after surgery, and no significant difference in paternity [12].
Hsieh et al. reported the result after using a modified microsurgical method, specifically a loup-assisted high inguinal varicocelectomy, rather than the usual microscope and sub-inguinal approach. One hundred sixteen patients underwent modified high inguinal varicocelectomy, From 1997 through 2000. An x3.0 loupe was used during the spermatic cord dissection at the level of the internal inguinal ring. The dilated veins were ligated and divided, along with vasal veins and external spermatic veins. Motile sperm concentration increased from 31.8 +/- 18.6% to 47.5 +/- 16.9% (p = 0.0004) and sperm concentration (10(6)/cc) increased from 26.2 +/- 18.7 to 42.8 +/- 28.5 (p = 0.0002) in the sample group after the procedure [13].
Nabi et al. assessed the technical feasibility and compared the semen quality in men after percutaneous embolization of varicoceles for infertility management. Between January 1997 and January 2002, 71 patients underwent an operation consisting of retrograde varicocele embolization for infertility. In 68 (95.7%), it was a technically successful and statistically significant improvement in the motility parameters, and semen density was achieved [14].
Schlegel and Kaufmann evaluated in a retrospective review effect of prior microsurgical varicocelectomy on sperm retrieval rates in men with nonobstructive azoospermia. Of 31 men who underwent varicocele repair for nonobstructive azoospermia, 7/31 (22%) had sperm reported on at least one semen analysis postoperatively. However, only 3/31 (9.6%) men after varicocele repair had adequate motile sperm in the ejaculate for intracytoplasmic sperm injection (ICSI) without testicular sperm extraction (TESE) [15].
Baazeem et al. evaluated the pregnancy outcomes of two groups of oligospermic men with varicocele. Group, I had a varicocelectomy, and the other not (group II). They retrospectively reviewed 233 oligospermic men who had microsurgical varicocelectomy (group I) between September 1996 and January 2002 and 127 men from the group of oligospermic men with varicoceles who did not have surgery (group II). The mean sperm concentration and motility increased significantly after varicocelectomy (P < 0.05). The natural pregnancy rate in group I (38%) was higher than in group II (30%). Additionally, the use of ART was significantly greater in group II than in group I. In the subset of couples with bilateral varicocele, the natural pregnancy rate was significantly higher in group I than group II (48% vs. 15%, respectively) [16].
Abdelrahman and Eassa evaluated the outcome of varicocelectomy after undergoing a modified microsurgical method-a loupe-assisted method, and its effects on sperm characteristics in infertile men. Half of the patients (20 patients from 40) were treated following a sub-inguinal approach assisted by loupe magnification (Group A), and the other (20 patients) were treated by the same approach but without magnification (Group B). An ×3.0 loupe was used to facilitate the procedure during the spermatic cord dissection at the level of the external inguinal ring. Group A showed a significant improvement in the sperm count, sperm motility, and decreased abnormal forms was observed after surgery. Group B showed similar effects without any significant differences [17].
Ollandini et al. reviewed the results of 376 patients from 2000 to 2010 who underwent varicocele correction using the retrograde sclerotization approach. The mean age at the time of surgery was 32 years, and 32% of them were 35 years and older. At three months after surgery, 253 (67%) patients showed improvement in sperm concentration, 227 (60%) in sperm motility, in morphology 180 (47%). Overall, 104 (28%) patients showed improvement in all the analyzed parameters [18].
Guo et al. investigated the clinical effect of microsurgical varicocelectomy on severe oligo-asthenospermia patients failing in fertilization assisted by intracytoplasmic sperm injection (ICSI). From January 2013 to August 2014, 49 patients with severe oligo-asthenospermia and serious varicoceles were treated by microsurgical varicocelectomy after unsuccessful fertilization assisted by ICSI. After surgery, 61.2% (30/49) of spouses became pregnant, among whom 22.4% (11/49) became naturally pregnant, 32.65% (16/49) conceived after second IVF-ET assistance, and 6.1% (3/49) conceived with the third or further assistance of intracytoplasmic sperm injection – embryo transfer (ICSI-ET). All of the patients improved in sperm concentration and motility. The fertility rate of IVF significantly improved to (83.36 ± 19.36) % from (72.36 ± 17.88) % [19].
Reddy et al. evaluated the effect of varicocele repair on sperm motility and concentration, testicular volume, and pregnancy rate in three different degrees of clinical varicocele. They retrospectively evaluated 482 infertile patients with varicocele who underwent varicocelectomy from December 2008 to December 2013. Significant differences were noted in sperm motility and concentration of patients with Grade 3 varicocele (as per World Health Organization grading (WHO 1993) system) as compared with Grade 1 and Grade 2 varicocele. Varicocelectomy markedly improved sperm motility, concentration, along with testicular volume. As a result, 32 to 41% of infertile patients achieved pregnancy spontaneously [20].
Majzoub et al. conducted a retrospective study of 378 patients who underwent left microsurgical sub-inguinal varicocelectomy. Patients were divided into abnormal and normal semen groups based on their initial semen results and additionally subdivided into three groups according to the number of veins ligated intraoperatively. Of the 378 patients, 332 patients had an abnormal semen analysis, while the remaining 46 patients had a normal result. The postoperatively result showed that sperm count, total motility, and progressive motility significantly increased after varicocelectomy. Sperm count and total motility, along with progressive motility, were significantly increased in 53.3% of patients postoperatively [21].
De Souza Alves and de Oliveira evaluated patients with non-obstructive azoospermia (NOA) and varicocele undergoing bilateral surgical correction for recovery of sperm production. They conducted a retrospective study from 2002 to 2015 at a private urologic service. In total, 25 patients underwent bilateral surgical repair of varicocele following a sub-inguinal approach assisted by loupe magnification. Four months after the operation, sperm was found in three patients (12%); after six months, sperm was identified in five (20%) patients. And after one year, only five (20%) patients had sperm in the ejaculate. However, out of 25 patients, three (12%) had changes in karyotype, and two (8%) had Y-chromosome microdeletions [22].
Balla et al. collected the data of 120 patients over seven years between 2010-2017 through a retrospective study. All patients were operated on for clinical varicocele associated with an abnormal spermogram. After the surgical treatment, an improvement in 14 (28%) spermograms was noted: 11 spermograms became normal, two with oligospermia and one with mild asthenospermia, the number of spontaneous pregnancies obtained was around 26% (13 couples). In Table 2 are summarized the results of previously published data on varicocele repair and outcomes [23].
|
Authors |
Year of publication |
Number of participants |
Procedures |
Results |
|
Vermeulen and Vandeweghe [9] |
1984 |
62 and untreated group (n = 20) |
Embolization of the vena spermatica |
15 of 62 had achieved a pregnancy; and 8 in untreated group. Varicocele correction showed a slight improvement of sperm quality; the severity of varicocele had no influence either on sperm characteristics or on the outcome of treatment. |
|
Ashkenazi et al. [10] |
1989 |
22 couples group I- 12 couples with mechanical female infertility, and group II -10 with normal female fertility |
spermatic vein ligation |
In the group, I, a 20% pregnancy rate was achieved after the operation, while in group II, four pregnancies (40%) trough IVF-ET. Plasma testosterone (T) levels increased in 50% of the patients of both groups after surgery, resulting in concurrently improved fertilization, cleavage, and pregnancy rates. |
|
Yamamoto et al. [11] |
1996 |
85 Group I -high ligation of the internal spermatic vein Group II- without any treatment |
High ligation of the internal spermatic vein |
The pregnancy rate in group I was 6.7% compared to 10% in group II, Group I had significantly higher levels of sperm density and total motile sperm count at one year. There were no significant differences between groups I and II regarding a change in seminal volume, sperm motility, and abnormal sperm morphology. |
|
Grasso et al. [12] |
2000 |
68 |
spermatic vein ligation |
No improvement in sperm quality after left spermatic vein ligation for low-grade varicocele and no significant difference in paternity. |
|
Hsieh et al. [13] |
2003 |
116 |
a loup-assisted high inguinal varicocelectomy |
The sperm concentration (10(6)/cc) increased from 26.2 +/- 18.7 to 42.8 +/- 28.5 (p = 0.0002). Motile sperm concentration increased from 31.8 +/- 18.6% to 47.5 +/- 16.9% (p = 0.0004) in the sample group. |
|
Nabi et al. [14] |
2004 |
71 |
Percutaneous embolization of varicoceles |
In 68 (95.7%), motility parameters, and semen density was improved. |
|
2004 |
31 |
Microsurgical varicocelectomy |
7/31 (22%) had sperm reported on at least one semen analysis postoperatively. 3/31 (9.6%) had adequate motile sperm in the ejaculate for ICSI without TESE. |
|
|
Baazeem et al. [16] |
2009 |
233 Compared to 127 men from the group of oligospermic men without operation |
Microsurgical varicocelectomy |
Sperm concentration, motility increased after varicocelectomy (P < 0.05). The natural pregnancy rate in group I (38%) and in group II (30%). The ART was greater in group II than in group I. Couples with bilateral varicocele, the natural pregnancy rate was significantly higher in group I than group II (48% vs. 15%). |
|
Abdelrahman and Eassa [17] |
2012 |
40 |
A loupe-assisted method 20 patients were treated by a sub-inguinal approach assisted by loupe magnification (Group A) 20 patients- were treated by the same approach but without magnification (Group B). |
Group A and B showed a significant improvement in the sperm count, sperm motility, and decreased abnormal forms was observed after surgery. |
|
Ollandini et al. [18] |
2014 |
376 |
Retrograde sclerotization approach |
After three months after surgery, 253 (67%) patients showed improvement in sperm concentration, 227 (60%) in sperm motility, morphology 180 (47%). 104 (28%) patients showed improvement in all parameters. |
|
Guo et al. [19] |
2016 |
49 |
Microsurgical varicocelectomy |
61.2% (30/49) of spouses became pregnant, among whom 22.4% (11/49) became naturally pregnant, 32.65% (16/49) conceived after second IVF-ET assistance, 6.1% (3/49) conceived with the third or further assistance of ICSI-ET. All improved in sperm concentration and motility. The fertility rate of IVF improved to (83.36 ± 19.36) % from (72.36 ± 17.88) %. |
|
Reddy et al. [20] |
2015 |
482 |
Varicocelectomy (unspecified) |
Sperm motility, concentration, testicular volume of patients with Grade 3 varicocele compared with Grade 1 and Grade 2 varicocele. 32 to 41% of infertile patients achieved pregnancy spontaneously. |
|
Majzoub et al. [21] |
2016 |
378 |
Microsurgical sub-inguinal varicocelectomy |
Sperm count, motility, progressive motility, were significantly increased in 53.3% of patients postoperatively. |
|
De Souza Alves and de Oliveira [22] |
2017 |
25 |
Bilateral surgical repair of varicocele by a sub-inguinal approach assisted by loupe magnification |
4 months after the operation, sperm was found in 3 patients (12%). After 6 months- in five (20%) patients. After 1 year, only five (20%) patients had sperm in the ejaculate. |
|
Balla et al. [23] |
2019 |
120 |
Varicocelectomy (unspecified) |
An improvement in 14 (28%) spermograms 11 spermograms became normal. Two with oligospermia one with mild asthenospermia Spontaneous pregnancies were around 26% (13 couples). |
Table 2: The summary of the results of previously published data on varicocele repair and fertility outcomes.
IVF-ET - in vitro fertilization-embryo transfer, ICSI - intracytoplasmic sperm injection, TESE - testicular sperm extraction, ICSI-ET - intracytoplasmic sperm injection – embryo transfer.
Conclusion
Varicocele is the most common clinical finding found in infertile males. The exact pathophysiology of varicocele remains unknown; however, there is a shred of convincing evidence that varicocele has an increasingly harmful effect on testes over time. Varicocele repair can help increase fertility by restoring blood flow to the scrotum, increasing sperm concentration and motility. Additionally, varicocele correction improves testosterone production, testicular volume and decreases sperm DNA fragmentation. However, it's still a challenge for andrologists to identify infertile men with varicocele who will most benefit from varicocele repair.
On the other hand, varicocele repair may improve the fertility of some patients, which is particularly important for couples desiring a child.
The efficacy of varicocele treatment for increasing fertility and pregnancy rate remains controversial over the last decade. Further studies should identify which treatment option better works for patients with a varicocele and which of them will benefit from it.
Further larger randomized, controlled trials are demanded for more precise assessments of the impact of varicocelectomy on fertility outcomes.
Conflict of Interest
The authors have no conflict of interest to declare.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Saypol DC. Varicocele. J Androl 2 (1981): 61-71.
- Conditions Treated. UCLA Health. Accessed on March 6, 2021. https://www.uclahealth.org/urology/body.cfm?id=478&action=detail&ref=19#:~:text=Varicocele%20Causes,veins%20to%20dilate%20(enlarge).
- Leslie SW, Sajjad H, Siref LE. Varicocele. 2021 Feb 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 28846314. https://pubmed.ncbi.nlm.nih.gov/28846314/
- Shiel WC. Jr. Medical definition of Varicocele. Medicine Net. Last Editorial Review: 12/27/2018. Accessed on March 6, 2021. https://www.medicinenet.com/varicocele/definition.htm
- Moazzam A. Oxidative Stress Induced Infertility in Varicocele. Andrology 5 (2016): 2167-2250.
- The Top 9 Symptoms of a Varicocele. Azura Vascular Care. Published May 2, 2017. Accessed on March 6, 2021. https://www.azuravascularcare.com/infovaricocele/symptoms-of-a-varicocele/
- Mayo Clinic. January 16, 2020. Accessed March 7, 2021. https://www.mayoclinic.org/diseases-conditions/varicocele/diagnosis-treatment/drc-20378772
- Chiba K, Fujisawa M. Clinical outcomes of varicocele repair in infertile men: a review. The World Journal of Men's Health 34 (2016): 101.
- Vermeulen A, Vandeweghe M. Improved fertility after varicocele correction: fact or fiction?. Fertility and Sterility 42 (1984): 249-256.
- Ashkenazi J, Dicker D, Feldberg D, et al. The impact of spermatic vein ligation on the male factor in in vitro fertilization-embryo transfer and its relation to testosterone levels before and after operation. Fertility and Sterility 51 (1989): 471-474.
- Yamamoto M, Hibi H, Hirata Y, et al. Effect of varicocelectomy on sperm parameters and pregnancy rate in patients with subclinical varicocele: a randomized prospective controlled study. The Journal of Urology 155 (1996): 1636-1638.
- Grasso M, Lania C, Castelli M, et al. Low-grade left varicocele in patients over 30 years old: the effect of spermatic vein ligation on fertility. BJU International 85 (2000): 305-307.
- Hsieh ML, Chang PL, Huang ST, et al. Loupe-assisted high inguinal varicocelectomy for sub-fertile men with varicoceles. Chang Gung Medical Journal 26 (2003): 479-484.
- Nabi G, Asterlings S, Greene DR, et al. Percutaneous embolization of varicoceles: outcomes and correlation of semen improvement with pregnancy. Urology 63 (2004): 359-363.
- Schlegel PN, Kaufmann J. Role of varicocelectomy in men with nonobstructive azoospermia. Fertility and Sterility 81 (2004): 1585-1588.
- Baazeem A, Boman JM, Libman J, et al. Microsurgical varicocelectomy for infertile men with oligospermia: differential effect of bilateral and unilateral varicocele on pregnancy outcomes. BJU International 104 (2009): 524-528.
- Abdelrahman SS, Eassa BI. Outcome of loupe-assisted sub-inguinal varicocelectomy in infertile men. Nephro-Urology Monthly 4 (2012): 535.
- Ollandini G, Trombetta C, Mazzon G, et al. Should older patients be offered varicocoele correction to improve their fertility?. Andrology 2 (2014): 402-407.
- Guo TH, Tong XH, Luo LH, et al. Value of microsurgical varicocelectomy for severe oligo-asthenospermia patients failed in fertilization assisted by in vitro fertilization. Eur Rev Med Pharmacol Sci 20 (2016): 1669-1674.
- Krishna Reddy SV, Basha Shaik A, Sailaja S, et al. Outcome of varicocelectomy with different degrees of clinical varicocele in infertile male. Advances in Andrology 2015 (2015).
- Majzoub A, Elbardisi H, Arafa M, et al. Does the number of veins ligated during varicococele surgery influence post-operative semen and hormone results?. Andrology 4 (2016): 939-943.
- Alves LD, Oliveira FB. Should azoospermic patients with varicocele disease undergo surgery to recover fertility?. Revista da Associação Médica Brasileira 63 (2017): 332-335.
- Balla B, Belcaid N, Elkaoukabi A, et al. Real Impact of Varicocele Surgery on Male Fertility.
