Exchange Transfusion-To do or Not to do for Neonatal Hyperbilirubinemia?
Article Information
Lajos Lakatos*
Department of Pediatrics, University of Debrecen, Debrecen, Hungary
*Corresponding Author: Lajos Lakatos, Department of Pediatrics, University of Debrecen, 4032 Debrecen, Nagyerdei Krt. 1, Hungary
Received: 04 March 2019; Accepted: 14 March 2019; Published: 18 March 2019
Citation:
Lajos Lakatos. Exchange Transfusion-To do or Not to do for Neonatal Hyperbilirubinemia?. Journal of Pediatrics, Perinatology and Child Health 3 (2019): 036-039.
View / Download Pdf Share at FacebookAbstract
Exchange transfusion for the treatment of neonatal hyperbilirubinemia is frequenly used also in the low- and middle-income countries. This unique intervention in the neonatal period is rather agressive and too expensive method as a therapy of a generally harmless disease. In neonates the chelating effects of D-Penicillamine (D-PA) play also important role: (i) in attenuating the oxidative stress, (ii) in the transient inhibition of heme oxygenase enzym resulting in a decrease of bilirubin production, and (iii) the age-relating effects of D-PA. Transition biometals now are in the focus of the etiopathogenesis of neurodegenerative and neurodevelopmental diseases (NDs) including the bilirubin-induced neurologic dysfunction (BIND). The “relatively” early diagnosis of jaundice takes suitable neonates for a short time (300 mg/kgbw per os, divided into three parts daily, for 2-5 days) D-PA treatment. It may be affordable especially in poorly resourced countries.
Keywords
D-Penicillamin, Hyperbilirubinemia, Exchange transfusion, Poorly resourced countries
Article Details
1. Introduction
In 1999, a provocative letter was written to persuade others to perform multicentre prospective randomized controlled clinical trials with the project of ~Prevention of Exchange Transfusion (ET) and Retinopathy of Prematurity (ROP) by D-Penicillamine (D-PA)~ [1].
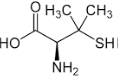
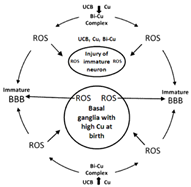
The chemical behavior of this drug can be discussed in terms of three types of reaction: formation of (1) disulfide bridges, (2) thiazolidine rings, (3) metal complexes and chelates [2]. Metal ions accumulate in the brain with aging and in several neurodegenerative diseases (NDs). In the neonatal period the chelating effects play also important role: (i) in attenuating the oxidative stress, (ii) in the transient inhibition of heme oxygenase (HO-1) enzym resulting in a decrease of bilirubin production, and (iii) the age-relating effects of D-PA [1]. Transition biometals now are in the focus of the etiopathogenesis of neurodegenerative and neurodevelopmental diseases (NDs) [3] including the bilirubin-induced neurologic dysfunction (BIND) in the neonatal period [4].
The neuropharmacological actions of metal-targeted agents most likely arise from local metal redistribution rather than from massive metal removal [5]. This goal may be achieved by abolishing abnormal metal/protein interactions, by contrasting localized metal excesses, by normalizing intra/extra cellular metal ratios or by restoring the correct balance among the main biometals: Cu, Fe, and Zn [6-8].
2. History and Protocol of Neonatal Exchange Transfusion
Neonatal hyperbilirubinemia (NHBI) is the most common condition (or symptom) in the first two weeks of postnatal life. Although generally harmless, some neonates may develop very high levels of total serum bilirubin level (TSB). Subtle encephalopathy or BIND refers to individuals with subtle neurodegenerative or neurodevelopmental damage.
- The term “acute bilirubin encephalopathy” is used to describe the acute manifestations of bilirubin toxicity.
- The term “kernicterus” is reserved for the chronic and permanent clinical sequelae of bilirubin toxicity.
- It is very difficult task to recognize which bilirubin levels are safe or which will definitely cause kernicterus or BIND.
- “Vigintiphobia”=if the serum bilirubin concentration is 20 mg/DL (340 μmol/L); at a level at which double volume exchange transfusion (ET) was recommended.
In rhesus hemolytic disease (Rh-HDN), it was found that kernicterus could be prevented if the TSB was kept below 20 mg/dL [9]. 30-35 years ago this recommendation was applied to other NHBIs as well. The guidelines are much more permissive nowadays concerning jaundice at 2 days to 2 weeks of age [10, 11].
3. The Neuroprotective Effects of Intravenously (or orally) Administered D-PA can make ETs
On the basis of our current knowledge, it is impossible to respond this question. Situations may arise, however, in the practice of neonatology, when the TSB is higher than the ET-compatible bilirubin values, and in these cases we have to apply alternative therapy (intensive phototherapy, drugs, including D-PA et cet.). In the retrospecting screening (in our 3 follow-up studies) these babies were examined at 1-44 years of age. They showed better somatic and mental development than the controls (the average Hungarian population without ET). In the Table 1, three particular interesting a convincing cases are demonstrated. Relevant data of their neonatal period were published in details earlier [12-14].
|
Variables |
Case of K.E |
Case of J.W |
Case of H.E |
|
Sex |
Female |
Female |
Male |
|
Birth weight (g) |
2200 |
2700 |
3100 |
|
Gestation (weeks) |
33 |
37 |
39 |
|
Blood group incomp. |
ABO-HDN |
Rh-HDN |
ABO-HDN |
|
Direct Coomps-test |
NP |
++++ |
NP |
|
Cord bilirubin (mg/dL) |
NA |
4.2 |
NA |
|
Peak bilirubin (mg/dL) at hours |
32.5 at 72 |
24.3 at 50 |
19.5 at 58 |
|
Hemoglobin (g/L) |
90.0 at 72 |
113.0 at 168 |
67.0 at 216 |
|
D-PA treatment (daily) |
IV 300 mg/kgbw |
p.o.300 mg/kg |
p.o. 300 mg/kg |
|
Phototherapy |
- |
+ |
+ |
|
Anemia “correction” |
60 ml PRBC |
Rh-erythropoetin |
60 ml PRBC 200 U/kgbw |
|
Last follow up (at years of age) |
44 |
18 |
18 |
|
Quality of life |
Opera singer |
Excellent in the school |
Suitable for a bad social situation |
(HDN-Hemolytic disease of the newborn; NP-Not performed; NA-Not available; IV-intravenously; PRBC-Packed red blood cells; Rh-erythropoetin-recombinant human erythropoietin.)
Table 1: Three, particular interesting cases in the praxis of Debrecen NICU (K.É.-ET was finished because of cardio respiratory arrest; J.W.-parents signed a request that blood should not be administered under any circumstances; H.E.-orally D-PA proved to be effective in early stage of ABO-HDN).
4. Conclusion
The “relatively” early diagnosis of hyperbilirubinemia takes suitable neonates for a short time (300 mg/kgbw per os, divided into three parts daily, for 2-5 days) D-PA treatment. It may be affordable, especially in poorly resourced countries [15].
References
- Lakatos L, Phelps DL, Watts JL. International replications, anyone? Arch Dis Childh Fetal Neonatal Ed 80 (1999): 252.
- Weigert WM, Offermans H, Scherberick P. D-penicillamine production and properties. Angew Chem Int Ed 14 (1975): 330-336.
- White A, Aschner M, Costa L, et al. Biometals in Neurodegenerative Diseases. Mechanisms and Therapeutics (1st) (2017).
- Lakatos L, Balla G. Bilirubin-induced neurologic dysfunction (BIND): appearances are fairly often deceptive. Birth Defect 2 (2017): 1-4.
- Mot AI, Wedd AG, Sinclair L, et al. Metal attenuating therapies in neurodegenerative disease. Exp Rev Neurother 12 (2011): 1717-1745.
- Aruoma OI, Halliwel B, Hoey BM, et al. The antioxidant action of N-acetylcysteine: Its reaction with hydrogen peroxide, hydroxyl radical, superoxide, and hypochlorous acid. Free Radic Biol Med 6 (1989): 593-597.
- Joyce DA, Day RO. D-penicillamine and D-penicillamine-protein disulphide in plasma and synovial fluid of patients with rheumatoid arthritis. Br J Clin Pharmacol 30 (1990): 511-517.
- Saugstad OD. Oxygen toxicity in the neonatal period. Acta Paediatr Scand 79 (1990): 881-892.
- Diamond LK, Allen FH, William OT. Erythroblastosis Fetalis-Treatment with Exchange Transfusion. NEJM 244 (1951): 39-49.
- Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. American Academy of Pediatrics. Pediatrics 114 (2004): 297-316.
- Patel RM, Josephson CD. 82-Neonatal Transfusion in: Avery’s diseases of the newborn (10th) (2018): 1180-1186.
- Lakatos L, Kover B, Peter F. D-penicillamine therapy of neonatal hyperbilirubinaemia. Acta Paediatr Acad Sci Hung 15 (1974): 77-85.
- Lakatos L, Csathy L, Nemes E. “Bloodless” treatment of a Jehovah’s Witness infant with ABO hemolytic disease. J Perinatol 19 (1999): 530-532.
- Lakatos L. Bloodless treatment of infants with hemolytic disease. Arch Dis Childh 89 (2004): 1076.
- Olusanya BO, Slusher TM. Infants at risk of significant hyperbilirubinemia in poorly resourced countries: evidence from a scoping review. World J Pediatr 11 (2015): 293-299.