Digital Smile Design Applied to Dental Esthetic: A Case Report
Article Information
Marina Rodrigues Santi1*, Beatriz Ometto Sahadi1, Rodrigo Barros Esteves Lins2, Marcelo GIANNINI3, Luis Roberto Marcondes Martins4
1Department of Restorative Dentistry, Operative Dentistry Division, Piracicaba Dental School, University of Campinas, Piracicaba, Brazil
2Substitute Professor, Dentistry Course, Center of Science, Technology, and Health, Paraíba State University, Araruna, Brazil
3Associate Professor, Department of Restorative Dentistry, Operative Dentistry Division, Piracicaba Dental School, University of Campinas, Piracicaba, Brazil
4Full Professor, Department of Restorative Dentistry, Operative Dentistry Division, Piracicaba Dental School, University of Campinas, Piracicaba, Brazil
*Corresponding Author: Marina Rodrigues Santi, Department of Restorative Dentistry, Operative Dentistry Division, Piracicaba Dental School, University of Campinas, Av. Limeira, 901 – ZIP CODE13414-903, Piracicaba, SP, Brazil
Received: 26 August 2020; Accepted: 02 September 2020; Published: 07 September 2020
Citation: Marina Rodrigues Santi, Beatriz Ometto Sahadi, Rodrigo Barros Esteves Lins, Marcelo GIANNINI, Luis Roberto Marcondes Martins. Digital Smile Design Applied to Dental Esthetic: A Case Report. Dental Research and Oral Health 3 (2020): 141-152.
View / Download Pdf Share at FacebookAbstract
The digital smile design (DSD) has been used as a tool for esthetic dentistry that improves predictability of rehabilitation procedures such as direct restorative techniques, which are an effective alternative with low cost to obtain dental esthetics in a short clinical time. This case report aimed to present an integrated planning related to functional, esthetic and emotional requirements from the patient based on digital design parameters. A 23-years-old male patient presented yellowed lateral incisors and canines, with diastema among anterior teeth, and dento-gingival disharmony. The facial harmony, dento-gingival parameters and teeth dimensions were analyzed using DSD. The following clinical procedures were performed: gingivoplasty surgery around the upper right and left lateral incisors (teeth 12 and 22), dental bleaching with 35% hydrogen peroxide combined with 15% carbamide peroxide, and upper anterior direct restorations using resin composite, which resulted in natural aspect and the harmony of the smile.
Keywords
Operative Dentistry, Resin Composite, Dental Esthetics, Dental Bleaching, Periodontal Esthetics
Operative Dentistry articles, Resin Composite articles, Dental Esthetics articles, Dental Bleaching articles, Periodontal Esthetics articles
Operative Dentistry articles Operative Dentistry Research articles Operative Dentistry review articles Operative Dentistry PubMed articles Operative Dentistry PubMed Central articles Operative Dentistry 2023 articles Operative Dentistry 2024 articles Operative Dentistry Scopus articles Operative Dentistry impact factor journals Operative Dentistry Scopus journals Operative Dentistry PubMed journals Operative Dentistry medical journals Operative Dentistry free journals Operative Dentistry best journals Operative Dentistry top journals Operative Dentistry free medical journals Operative Dentistry famous journals Operative Dentistry Google Scholar indexed journals Resin Composite articles Resin Composite Research articles Resin Composite review articles Resin Composite PubMed articles Resin Composite PubMed Central articles Resin Composite 2023 articles Resin Composite 2024 articles Resin Composite Scopus articles Resin Composite impact factor journals Resin Composite Scopus journals Resin Composite PubMed journals Resin Composite medical journals Resin Composite free journals Resin Composite best journals Resin Composite top journals Resin Composite free medical journals Resin Composite famous journals Resin Composite Google Scholar indexed journals Dental Esthetics articles Dental Esthetics Research articles Dental Esthetics review articles Dental Esthetics PubMed articles Dental Esthetics PubMed Central articles Dental Esthetics 2023 articles Dental Esthetics 2024 articles Dental Esthetics Scopus articles Dental Esthetics impact factor journals Dental Esthetics Scopus journals Dental Esthetics PubMed journals Dental Esthetics medical journals Dental Esthetics free journals Dental Esthetics best journals Dental Esthetics top journals Dental Esthetics free medical journals Dental Esthetics famous journals Dental Esthetics Google Scholar indexed journals Dental Bleaching articles Dental Bleaching Research articles Dental Bleaching review articles Dental Bleaching PubMed articles Dental Bleaching PubMed Central articles Dental Bleaching 2023 articles Dental Bleaching 2024 articles Dental Bleaching Scopus articles Dental Bleaching impact factor journals Dental Bleaching Scopus journals Dental Bleaching PubMed journals Dental Bleaching medical journals Dental Bleaching free journals Dental Bleaching best journals Dental Bleaching top journals Dental Bleaching free medical journals Dental Bleaching famous journals Dental Bleaching Google Scholar indexed journals Periodontal Esthetics articles Periodontal Esthetics Research articles Periodontal Esthetics review articles Periodontal Esthetics PubMed articles Periodontal Esthetics PubMed Central articles Periodontal Esthetics 2023 articles Periodontal Esthetics 2024 articles Periodontal Esthetics Scopus articles Periodontal Esthetics impact factor journals Periodontal Esthetics Scopus journals Periodontal Esthetics PubMed journals Periodontal Esthetics medical journals Periodontal Esthetics free journals Periodontal Esthetics best journals Periodontal Esthetics top journals Periodontal Esthetics free medical journals Periodontal Esthetics famous journals Periodontal Esthetics Google Scholar indexed journals
Article Details
1. Introduction
Modern dentistry has moved beyond simply being concerned with teeth and gums, requiring clinicians to integrate the smile with the “frame” of the overall face [1]. The smile disharmony that in many cases is associated with the asymmetry and/or disproportionality among the teeth, periodontal and orofacial structures is the main reasons why patients seeking for clinical procedures in esthetic dentistry [1, 2]. The increase demand for esthetic standards, beauty and dental harmony has provided a constant development in dental technology, aiming to facilitate and complement the performance of clinical procedures using digital simulations [1]. An example of digital simulator is the Digital Smile Design (DSD), which provides better analysis of possible treatments, predictability of results, professional-patient approach and interdisciplinary communication between the professionals [1, 3]. A clinical application of this technology is to evaluate proportions and corrections in the shape and size of the teeth, such as in cases of dental diastemas [1, 3, 4]. Diastemas are defined as a space between the teeth or the absence of contact between two or more consecutive teeth, usually found in the anterior teeth [2, 4]. Among the suggested clinical decisions for the closing of diastemas, orthodontics, direct restorations, and prosthodontics are the most used. Direct restorative techniques are preferred because the technique is simpler, faster and of lower cost value [1, 2, 5].
The preparations according to the minimally invasive concepts have changed the restorative dentistry and the combination of the adhesive technique with esthetic restorative materials allow to recover the tooth function and natural features [2, 4]. Resin composites are materials that has esthetic characteristics with a wide range of colors and translucency. Also, they present adequate mechanic properties that allow procedures to be performed with minimal or no removal of healthy dental structure and reproducing the optical properties of the natural teeth [6]. To promote a desirable esthetic outcome, a pleasing smile involves, besides restorative material placement, the multidisciplinary among areas of dentistry, such as the gingival tissues [7]. Gingival exposure higher than 3 mm may compromise facial harmony and the relationship between white esthetics (teeth) and pink esthetics (gingiva) [7, 8]. Therefore, a multidisciplinary approach is essential for an accurate esthetic diagnosis and to attain an adequate treatment plan in order to achieve satisfactory results and restore oral health pragmatically and conservatively. This case report aimed to present a multidisciplinary approach with an integrated treatment related to functional, aesthetic and conservative restorative procedures based on DSD diagnostic.
2. Case Report
Patient LGG, male, 23-years-old, sought care at the Dentistry Clinic of Piracicaba Dental School complaining of “yellowish smile, with spaces between teeth”. Initially, the anamnesis and clinical examination were performed. For the analysis and treatment planning of the case it was taken the complete photograph documentation (extra and intraoral), with the following sequence:1.Extra-oral photos: (Figure 1): forced smile (Figure 1a); spontaneous smile (Figure 1b); and 2.Intra oral photos (Figure 2) initial intraoral photo (Figure 2a); right side (Figure 2b) and left side view of smile (Figure 2c). In the same appointment, the patient was submitted to the impressions using alginate to obtain the die cast that were scanned (R700, 3Shape, Copenhagen K, Denmark) for digital planning. Subsequently, with the aid of the software (Keynote-iWork, Apple, Cupertino, California, USA), lines were drawn to analyze orofacial harmonization (Figure 3). In the die cast, length of the left central incisor was measured in the width-height ratio in order to calibrate the digital ruler, based on the measurements obtained. A design with an optimal length/width ratio (80%) was established on the central incisors to compare actual and ideal proportion for the case (Figure 4). From the centrals incisors, the final drawing of the contour of the teeth was performed according to the patient's characteristics and guided by the lines drawn in the extra oral photo and by the calculated proportion, showing the relationship between the ideal dental situation and the relationship with the midline closing the diastema (Figure 5).
According to the options for restorative technics, the treatment choice for the restoration procedure was resin composite. It was planned direct restorations of upper canine to canine (13 to 23) and gingivoplasty on upper lateral incisors (teeth 12 and 22) to correct teeth length and gingival zenith harmony (Figure 6). The treatment plan based on the DSD was proposed to the patient and analyzing the images and the predictability of the final result, the patient consented the execution. The final 3D file was exported to a 3D printer (W3D Print, Wilcols, RJ, Brazil) which generated the new model with the smile design planed. To begin the clinical procedures, the gingivoplasty was the first step. With a periodontal probe, it was checked if the patient had 3 mm from the gingival margin to the cementum-enamel junction, then, demarcation of bleeding points was made. The primary incision was done with a scalpel (blade # 15c) at 45° angled incision with internal bevel to provide a thin and rounded margin of the remaining gingiva. The incised tissues were carefully removed with the help of Gracey's curettes (Figure 7).
Following 45 days after gingivoplasty, the in-office dental bleaching technique was performed using 38% hydrogen peroxide gel (Opalescence Xtra Boost, Ultradent Products Inc; S. Jordan, UT, USA). The prophylaxis and photograph records were done before bleaching (Figure 8a). Gingiva and soft tissues were protected with an oral retractor and a light-cured gingival barrier (Opaldam, Ultradent Products Inc; S. Jordan, UT, USA). After two bleaching gel applications, a neutral and colorless fluoride was applied. The patient was oriented to use 15% carbamide peroxide gel (Opalescence PF, Ultradent Products Inc; S. Jordan, UT, USA) during 15 days, for 4 hours daily. After following the dental bleaching treatments, the new photographs were taken to record the teeth color (Figure 8b).
Elapsed 15 days bleaching treatment, it was taken the color of the teeth according to the VITA scale (Vita Tooth guide, Zahnfabrik, Bad Säckingen, Germany) to start the restorative procedure. A silicon guide (Express XT, 3M ESPE; St. Paul, MN, USA) was made following the model with the digital wax up in order to facilitate the restorative procedure (Figure 9). The dental enamel was slightly abraded with a carbide burr no. 2135 (KG Sorensen, Cotia, SP, Brazil), with an inclination of approximately 45° in relation to the long axis of the tooth. Then, the modified rubber dam isolation of the operative field was applied to protect the patient and improve the quality of composite restorations. Teeth was conditioned with 37% phosphoric acid (Ultra-etch, Ultradent Products Inc; S. Jordan, UT, USA) for 30 seconds, washed with water and dried for 60 seconds. The adhesive system (Scotchbond Multipurpose, 3M ESPE; St. Paul, MN, USA) was applied and light-cured (Valo, Ultradent Products Inc; S. Jordan, UT, USA) for 20 seconds (Figure 10). An increment of resin composite of WE shade (Filtek Supreme Ultra, 3M ESPE; St. Paul, MN, USA) to serve as the palatine enamel was placed in the silicone guide (Figure 11). This silicon guide was positioned on respective teeth surfaces and the resin composite was light cured for 20s (Figure 12). Subsequently, resin composite of A1D and A1B shade were placed (Filtek Supreme Ultra, 3M Oral Care; St. Paul, MN, USA), performing the dentin characteristics. The last layer of 0.5 mm of enamel resin composite (Estelite Sigma Quick, Tokuyama Dental Corporation; Tokyo, Japan) was added in A1WE shade. After flash removal and checking the occlusal contacts and guides, the procedure of finishing and polishing was performed. The texture of surface was made with 12-fluted multi-laminated bur (Kerr Corporation, Joinville, SC, Brazil). The polishing was performed with abrasive points (Jiffy Brush, Ultradent Products Inc; S. Jordan, UT, USA) and silicon carbide brushes (FlexiBrush, Cosmedent; Chicago, IL, USA) followed by an aluminum oxide polishing paste (Enamelize Polishing Paste, Cosmedent; Chicago, IL, USA) with a felt disc (FlexiBuff, Cosmedent; Chicago, IL, USA) (Figures 13 and 14).
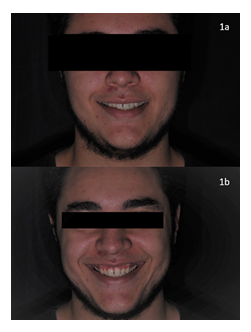
Figure 1: Extra-oral photos: 1a) Forced smile; 1b) Spontaneous smile.

Figure 2: Intra oral photos: 2a) Initial intraoral photo; 2b) Right side; 2c) Left side view of smile.
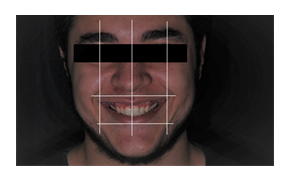
Figure 3: Orofacial harmonization lines.

Figure 4: Ideal proportion.

Figure 5: Final draw.
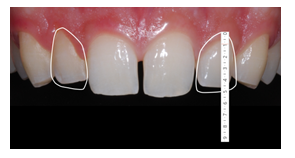
Figure 6: Delimitation for zenith correction.
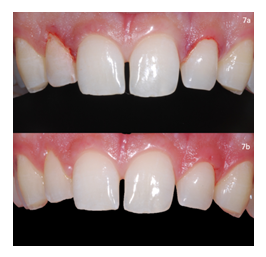
Figure 7: Gingivoplasty procedure: 7a) Inicial aspect before the gingivoplasty; 7b) Final aspect after the gengivoplasty.
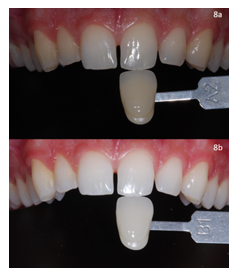
Figure 8: Bleaching procedure: 8a) Inicial substrate color (A2); 8b) Substrate color after the dental bleaching (B1).

Figure 9: Silicone barrier.
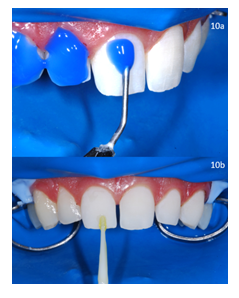
Figure 10: Inicial of the restorative procedure: 10a) Acid conditioning; 10b) Adhesive system.
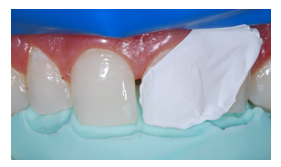
Figure 11: Silicone guide positioned.

Figure 12: Resin composite increment light-cured.

Figure 13: volume and alignment analysis.

Figure 14: Final smile.
3. Discussion
Progress in dental techniques and materials has enabled the accomplishment of procedures that reestablish the esthetics, function, and biologic characteristics of oral tissues [9]. Diastemas in anterior teeth can affect the appearance of a smile and the treatment are based on, orthodontic treatment, restorative treatment, or their combination [10]. Depending on certain factors, such as the treatment costs, the available clinical time, and the number and size of diastema, direct adhesive restorations with composite resins or indirect restorations with porcelain veneers may represent an excellent alternative of restorative treatments [11]; however, regardless of technique used, it is mandatory to establish a treatment plan, based on complementary exams performed [12]. The importance to determine a treatment plain is related to patient’s understanding of the clinical steps, often based on multidisciplinary treatment. Moreover, it helps in the communication between all the professionals, as well as a guideline to operators [12]. When esthetic procedures are required for diastema corrections, the diagnostic wax-up is important method that shows a previous result of the final appearance, and it is an important laboratory step to confirm the treatment plan fixed [7]. After choosing the ideal treatment plan, the diagnostic wax-up was used to analyze the proportional balance of dental and gingival tissues, because both influence in the facial beauty of smile. Incorrect proportion and teeth dimensions are related to “an unpleasing smile”, because the excessive gingival tissue zone is exposed.
Besides of the proportion balance between the soft and hard tissues, there are other components also important and should be considered in the smile evaluation, such as: midline position, smile line, incisal edge, incisal crenels, age, gender, color and texture of the teeth [1]. To facilitate the planning of this case, a simple technique that requires only a software, such as Power Point or Keynote and photos taken from a digital camera were used [1, 3]. The use of the DSD makes the treatment highly personalized and the multidisciplinary approach achieved with esthetic dental improvement in short period of time [1, 3]. This digital tool allows a previous esthetic result, from the placement of lines and digital draws on extra and intraoral photos following a specific sequence to guide and evaluate the esthetic relationship among teeth, gingiva, smile and face [1]. These images allow the dentist and the patient to have a better understanding of existing problems and make possible to create the best solutions for the case [13]. According to the DSD applied for this 23-year-old male patient, the dental proportion calculation showed that the length and width of the central incisor and canine was higher than the lateral incisor on both sides. To establish the balance of teeth dimensions and gingival tissues, a gingival plastic surgery was performed to reduce the gingival exposed, correct the teeth proportion and maintaining a 3 mm distance from the marginal gingiva to the alveolar bone crest, as recommended by several authors to ensure an adequate biologic space when placing the restoration 0.5 mm under the gingival margin avoiding gingival inflammation, pocket formation, and alveolar bone loss [7, 14, 15]. The conformation of a new dental zenith after periodontal surgery promoted a new proportional dental architecture and this was an important step to accomplish an esthetic result, because an unbalance proportion of the anterior teeth differed from the dimensions of the golden proportion concept [8, 16].
The “golden proportion” is one of the most popular dental proportion architecture theories used in maxillary anterior teeth restoration and it is based on the relationship between natural beauty and mathematics [1, 11, 16]. It is worth stressing that the visible width of an anterior upper tooth should not exceed 80% of its length [10]. Thus, based on this proportion, from the frontal view, the maxillary lateral incisor should be approximately 62% of the width of the maxillary central incisor, and the width of the maxillary canine should be approximately 62% of the width of the respective lateral incisor [11]. This clinical report considered the DSD to establish the treatment plan; however, some authors affirm that the golden proportion is not observed by non-dentist population [17] . and there is no significance any proportion for the anterior teeth [18]. Other authors affirm is that the color of the teeth is a more common concern for many patients than the shape [19, 20, 21]. Tooth whitening was performed with the combined technique of in-office and at-home bleaching. In younger patients, such as this 23-year-old, lighter-colored teeth can be improved if the tooth color is close to the eye sclera [19]. According to Rezende et al [22], this combination of in-office and at-home bleaching enables the bleaching process to be accelerated, promotes stability of the bleaching effects and may help motivate the patient due to faster visual results. The recommended time to place composite restorations after carbamide peroxide bleaching is up to 3 weeks [23, 24]. Several previous investigations found a significant reduction in resin–enamel bond strengths after hydrogen or carbamide peroxide bleaching, when the composite restoration was performed immediately after completing bleaching [19, 23]. Residual oxygen from the bleaching agent on enamel surfaces may cause poor bond strength [24]. As an alternative to reduce time after bleaching, Sultan and Elkorashy [25] suggested that the use of antioxidants (10% ascorbic acid or 10% hesperidin for 10 minutes, 1 hour after the bleaching procedure) to improve the bond strength between enamel and restoration, allowing the final restoration to be performed in the same session. In this clinical case, an interval of 2 weeks was respected to start the restorative procedures.
Orthodontic treatment is considered as an option available for diastema closure, such as direct composite resin restorations or laminate veneers, but many patients are not receptive to orthodontic treatment due to extended time required [26]. Moreover, the esthetic resolution of this case may not occur only or restrict for orthodontic intervention. Individual characteristics of the dental elements, such as shape, size, and height are not altered, requiring multidisciplinary treatment for satisfactory results in esthetics and function [27]. The use of resin composite is considered the restorative technique more conventional, conservative compared with full facial coverage porcelain veneers, requires less clinical time, preserves tooth structure, with the possibility of being performed in a single session, and low cost [2, 10]. A study of 5 year follow up of closing diastema using direct resin composite showed less or no unfavorable marginal gaps, secondary caries or loss of retention and most of the recorded events were incisal cohesive chipping within the resin composite [28]. This is the best benefit for the patient, who experiences shorter treatment time and lower treatment cost and, indubitably, induces a better prognosis for the tooth, in which the beginning of the repeated restorative cycle is prevented [29].
In the current clinical case, a non-or minimally invasive treatment approach was performed, which provided an alternative treatment for the esthetic correction and reshaping of anterior teeth. With the predictability of the ideal size and shape of the teeth from the diagnostic wax-up and a silicone guide [30]. This guide facilitates the placement of composite to create the new enamel palatal wall, which results in a functionally correct surface. Moreover, the stratification technique of dentin core, internal staining, and subsequent enamel layer give the optical illusion and represent a simple and effective alternative to obtain the best teeth appearance [31]. To achieve esthetically pleasing treatment, a multidisciplinary approach and smile analysis are essential [32]. Dental photographs and a DSD digital tool provided the dimensions and proportions of the teeth and are also important in dentist–lab technician communication bringing predictability results [1, 13]. A diagnostic wax-up can display the desired treatment outcome and thus can be visualized by both the practitioner and the patient. With the correct treatment plan, the direct composite resin can provide an excellent esthetic result correcting and reshaping anterior teeth. This clinical case was finalized with patient’s feeling of satisfaction from multidisciplinary treatments performed with a conservative approach.
4. Conclusion
In clinical cases in which a non- or minimally invasive treatment approach is indicated, DSD combined with direct composite restorations provide predictability and an excellent alternative treatment for the esthetic corrections and reshaping of anterior teeth.
Acknowledgements and Conflicts of Interest
None.
References
- Coachman C, Calamita M. Digital smile design: a tool for treatment planning and communication in esthetic dentistry. Quintessence Dent Technol 35 (2012): 103-111.
- Kina M, Leal FA, Fabre AF, et al. Treatment minimally invasive aesthetic restorative through direct technique with composite: Case report. Arch Health Invest 4 (2015): 50-55.
- Okida RC, Moura APDE, Franco LM, et al. The use of dsd (digital smile design) for the optimization of the dental esthetics. Revista Odontológica de Araçatuba (2017): 9-14.
- Sene F, Kasuya AVB. Esthetic remodeling of maxillary incisors with composite resin: color, shape and proportion correction. J Clin Dent Res 13 (2016): 70-77.
- Bernardon JK, Gondo R, Baratieri LN. Minimally invasive restorative treatment of hypoplastic enamel in anterior teeth. Am J Esthet Dent 1 (2011): 10-24.
- Nahsan FP, Mondelli RF, Franco EB, et al. Clinical strategies for esthetic excellence in anterior tooth restorations: understanding color and composite resin selection. J Appl Oral Sci 20 (2012): 151-156.
- Jha N, Ryu JJ, Wahab R, et al. Treatment of oral hyperpigmentation and gummy smile using lasers and role of plasma as a novel treatment technique in dentistry: an introductory review. Oncotarget 8 (2017): 20496-20509.
- Tawfik OK, El-Nahass HE, Shipman P, et al. Lip repositioning for the treatment of excess gingival display: a systematic review. J Esthet Restor Dent 30 (2018): 101-112.
- Baratieri LN, Araujo EM Jr, Monteiro S Jr. Composite restorations in anterior teeth: fundamentals and possibilities. Chicago (IL): Quintessence Books (2005).
- Araujo EM Jr, Baratieri LN, Monteiro S Jr, et al. Direct adhesive restoration of anterior teeth: part 3: procedural considerations. Pract Proced Aesthet Dent 15 (2003): 433-438.
- Ward DH. A study of dentists’ preferred maxillary anterior tooth width proportions: comparing the recurring esthetic dental proportion to other mathematical and naturally occurring proportions. J Esthet Restor Dent 19 (2007): 324-339.
- Ittipuriphat I, Leevailoj C. Anterior space management: interdisciplinary concepts. J Esthet Restor Dent 25 (2013): 16-30.
- Niranjan NT, Kanaparthy A, Kanaparthy R, et al. Photographic and manual evaluation of golden percentage and recurrent aesthetic dental proportion in aesthetic smiles. J Evolution Med Dent Sci 5 (2016): 2267-2270.
- Pontoriero R, Carnevale G. Surgical crown lengthening: a 12-month clinical wound healing study. J Periodontol 72 (2001): 841-848.
- Ahmed AJ, Nichani AS, Venugopal R. An evaluation of the effect of periodontal biotype on inter-dental papilla proportions, distances between facial and palatal papillae in the maxillary anterior dentition. J Prosthodont 27 (2018): 517-522.
- Basting RT, Trindade RS, Flório FM. Comparative study of smile analysis by subjective and computerized methods. Oper Dent 31 (2006): 652-659.
- Mahshid M, Khoshvaghti A, Varshosaz M, et al. Evaluation of “golden proportion” in individuals with an esthetic smile. J Esthet Restor Dent 16 (2004): 185-193.
- Ufuk H, Semih B, Kerem A, et al. An analysis of maxillary anterior teeth: facial and dental proportions. J Prosthet Dent 94 (2005): 530-538.
- Joshi SB. An overview of vital teeth bleaching. J Interd Dent 6 (2016): 3-13.
- Joiner A, Luo W. Tooth colour and whiteness: A review. J Dent 67S (2017): S3-S10.
- Gómez-Polo C, Montero J, Gómez-Polo M, et al. Natural Tooth Color Estimation Based on Age and Gender. J Prosthodont 26 (2017): 107-114.
- Rezende M, Ferri L, Kossatz S, et al. Combined bleaching technique using low and high hydrogen peroxide in-office bleaching gel. Oper Dent 41 (2016): 388-396.
- Cavalli V, Carvalho RM, Giannini M. Influence of carbamide peroxide-based bleaching agents on the bond strength of resin-enamel/dentin interfaces. Braz. oral res 19 (2005): 23-29.
- Nour El-din AK, Miller BH, Griggs JA, et al. Immediate bonding to bleached enamel. Oper Dent 31 (2006): 106-114.
- Sultan MS, Elkorashy ME. Influence of natural antioxidants on microshear bond strength to bleached enamel: chemical versus laser assisted bleaching. Egyptian Dent J 63 (2017): 419-427.
- Fortkamp S, Araújo Junior EM, Baratieri LN. Papillary induction in anterior teeth with diastema using direct adhesive restorations: a case report. Clínica – Int J Braz Dent 1 (2005): 127-123.
- Seymour DW, Patel M, Chan MFWY. Aesthetic preview: a novel approach. Dent Update 39 (2012): 422-426.
- Frese C, Schiller P, Staehle HJ, et al. Recontouring teeth and closing diastemas with direct composite buildups: a 5-year follow-up. J Dent 41 (2013): 979-985.
- Poyser NJ, Briggs PF, Chana HS, et al. The evaluation of direct composite restorations for the worn mandibular anterior dentition – clinical performance and patient satisfaction. Journal of Oral Rehabilitation 34 (2007): 361-376.
