Development and Assessment of the Reliability and Validity of a Psychological Stress Scale for Catheterized Home Healthcare Patients
Article Information
Toshihide Ito1,*, Ryoichi Ichihashi2, Kouichi Tanabe3, Tomomi Umemura1, Masakazu Uemura1, Yoshimasa Nagao1
1Department of Patient Safety, Nagoya University Hospital, 65 Tsurumai-cho, Showa-ku, Nagoya, Aichi 466-0065, Japan
2General Home Care Clinic, 4-12 Yakushiji Ginan-cho Hashima-gun Gifu, Japan
3Faculty of Pharmacy, Meijo University, 150 Yagotoyama, Tempaku-ku, Nagoya, Aichi 468-8503, Japan
*Corresponding author: Toshihide Ito, Department of Patient Safety, Nagoya University Hospital, 65 Tsurumai-cho, Showa-ku, Nagoya, Aichi 466-0065, Japan. Tel: +81 52 741 2111
Received: 28 November 2021; Accepted: 07 December 2021; Published: 07 January 2022
Citation:
Toshihide Ito, Ryoichi Ichihashi, Kouichi Tanabe, Tomomi Umemura, Masakazu Uemura, Yoshimasa Nagao. Development and Assessment of the Reliability and Validity of a Psychological Stress Scale for Catheterized Home Healthcare Patients. Journal of Pharmacy and Pharmacology Research 6 (2022): 1-14.
View / Download Pdf Share at FacebookAbstract
Background: Accidental dislodgement of tubes/catheters from patients’ bodies is frequent in healthcare; making it a crucial patient safety management issue. Additionally, the number of pati-ents needing catheter management at home has increased with the rise in aging patients. Pain or stre-ss from directly inserting a tube/catheter into the body causes accidental dislodgement. However, quantitative measurements have not yet been devel-oped to evaluate patients’ stress resulting from dislodgement fear.
Aim: This study aimed to develop a psychological stress scale for patients using tubes/catheters at home (PSS-CP) and evaluate its reliability and validity.
Materials and Methods: The questionnaire was developed through interviews with 10 patients using tubes/catheters at home. Reliability was examined using the test-retest method and Cronbach’s α. Factorial and criterion-related validity were examined using exploratory factor analysis and the 12-item General Health Questionnaire, respectively.
Results: The PSS-CP comprised 16 items across four factors: “anxiety about catheter dislodgement while moving or in the toilet,” “anxiety about tube dislodgement when resting or lying down,” “anxiety about tube dislodgement while dressing/undressing,” and “anxiety about tube dislodgement while bathing.” Criterion-related validity was significantly correlated with general anxiety (r = 0.71, p < 0.01) and pain/discomfort (r = 0.364, p < 0.05). The retest method showed a highly significant correlation (r = 0.791, p < 0.01), with Cronbach’s α > .90.
Conclusions: A scale to measure psychological stress among catheterized home healthcare patients was developed and its reliability and validity demonstrated.
Keywords
stress, home healthcare, health safety, patient safety, scale development
stress articles, home healthcare articles, health safety articles, patient safety articles, scale development articles
Article Details
1. Introduction
Accidental dislodgement of tubes/catheters from patients’ bodies frequently occurs in healthcare settings [1, 2]. Such dislodgements, other than endangering the patient’s life, entail high costs for both patients and healthcare professionals alike, resulting in problems such as disruption of targeted drugs and nutritional delivery, persistence of foreign substances, pain/insertion error/injury at reinsertion, increased strain on labor resources, and elevated economic costs. Hence, the prevention of accidental dislodgements has emerged as a crucial issue in patient safety management.
Considering this clinical issue, hospitals have increasingly adopted countermeasures, including the use of more firmly secured tubes/catheters and physical restraints on patients [3]. According to the Japan Council for Quality Health Care Medical Accident Prevention Center’s online publication, “Japan Council for Quality Health Care Project to Collect Medical Near-Miss/Adverse Event Information 2018 Annual Report,” medical instit-utions reporting on tube/catheter management disclosed a high incidence of dislodgement: 1,210 self-dislodgement and 126 spontaneously dislodged tubes/catheters [4]. Furthermore, existing data attribute the highest incidence of accidental tube/catheter dislo-dgement to acute geriatric hospitals [5], signifying that such accidental dislod-gements still remain an unaddressed problem.
Meanwhile, with the progression of home healthcare systems, the number of patients needing catheter management at home is increasing. Tubes and catheters play an essential role in home healthcare and have been used to administer injectable narcotics in terminally ill cancer patients [6, 7], provide central venous and enteral nutrition in patients undergoing nutrition management [8, 9], and for many other purposes. This trend has unfortunately been accompanied by numerous incidents wherein a tube or catheter, such as a feeding tube, becomes dislodged in a home healthcare setting [10]. Dislodgements, particularly those involving central venous nutrition, can endanger life and diminish patients’ quality of life (QOL). Hence, the risk of tube/catheter dislodgement in these settings is a serious problem.
As to the causes of accidental dislodgement, tubes/catheters may be spontaneously dislodged due to body movements or stress experienced by the patient. Particularly, for stress-related self-dislod-gements, the pain and stress caused by catheterization may potentially be causative factors [6, 7]. Further, the catheterized patients’ constant fear of dislo-dgement causes them severe stress, adversely impacting their physical and mental wellbeing [11-13]. Hence, the measurement and mitigation of stress and fear in catheterized patients are crucial from the perspective of preventing tube/catheter self-dislod-gement and maintaining adequate QOL. A particular concern is that accidental dislodgements in home care settings cannot be dealt with immediately because patients in a home healthcare setting are not monitored around the clock by medical professionals as they would be in a hospital setting. This problem is serious because accidental dislodgement in drip infusion can endanger life. To mitigate this risk, it is important to regularly assess whether the patient in question can safely use the tube/catheter. To that end, it is necessary to visualize tube/catheter-related stress one of the causes of accidental dislodgement. However, although there are instruments that meas-ure patients’ stress responses to treatment [14, 15] and caregivers’ stress in home-based care [16-19], to the best of our knowledge, there are no instruments for measuring the stress and discomfort experienced by patients in home care settings in their daily lives as a result of using tubes/catheters. Thus, in this study, we developed a scale for measuring psych-ological stress in patients who use tubes/catheters in a home healthcare setting, a Psychological Stress Scale for Catheterized Home Healthcare Patients (PSS-CP).
2. Material and Methods
2.1 Data collection
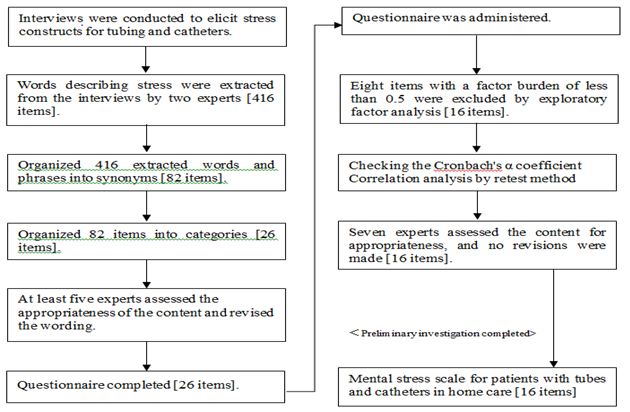
The PSS-CP was developed after conducting semi-structured interviews with 10 patients who were being treated at a general home health care clinic using tubes and catheters (e.g., indwelling bladder catheters, peripheral intravenous infusions, etc.; Fig. 1). Each interview lasted 40-60 minutes and was recorded and transcribed, and the content was analyzed to identify phrases indicative of stress. The series of interviews was terminated after the tenth patient, as data saturation had been achieved. Content analysis to identify phrases indicative of stress was independently performed by two patient safety specialists, resulting in the identification of 82 categories of stress and a Cohen’s kappa coefficient of 0.84. After consultation, the two specialists agreed on 26 categories that were used to develop relevant items for the scale. To measure these items as continuous variables and to score the scale, we only considered rating scales of at least five points. Considering Japanese people’s tendency to select a middle response alternative [20], we decided to avoid odd numbers of responses and used a six-point scale: “I don't think so at all: 1 point”; “I don't think so: 2 points”; “Somewhat disagree: 3 points”; “Somewhat agree: 4 points”; “I think so: 5 points”; “I totally agree: 6 points.”
2.2 Subjects
Patients using the following tubes and catheters at home were included in the study: intravenous hyperalimentation (IVH), percutaneous transhepatic cholangial drainage (PTCD), indwelling bladder catheters, nephrostomy, cystostomy, continuous subcutaneous injection of narcotics, peripheral intravenous infusion, oxygen cannula, percutaneous transhepatic gallbladder drainage (PTGBD), indwelling catheters, nasal drainage, nasal feeding, gastrostomy, enterostomy, and central venous (CV) port. Exclusion criteria were patients who had a short infusion and were accompanied by medical personnel during the infusion or who could not communicate verbally.
2.3 Procedure
A survey was conducted from August 2018 to July 2019 to develop a questionnaire. The target extraction includes patients using homecare and home-visit services (for those residing in Aichi and Gifu Prefectures). We also selected patients who met the selection criteria based on their medical records, and those who consented to participate were interviewed using the interview guide. Afterward, a questionnaire was created based on the interview data, and the contents and methods of the survey were explained to patients using home medical care or home-visit care after the medical treatment or home nursing care was completed. Those who provided consent received information on the details and methods of the survey during medical treatment or at the completion of home nursing care, and questionnaires were hand-delivered. If the consent form was signed and the questionnaire was filled out at the time of the second medical examination or nursing visit, the patient was considered to have consented, and the questionnaire was collected. However, if it was not filled out, it was determined that consent was not obtained.
2.4 Questionnaire items
In addition to the questionnaire items included in the PSS-CP, sociodemographic data was collected, including age, gender, duration of using home healthcare, duration of using tubes/catheters at home, and history of tubes/catheters removal.
2.5 Data Analysis
To account for differences in prognosis, the analysis was stratified into cancer and non-cancer patients.
2.6 Content Validity
Preliminary tube/catheter-related stress items were screened for inappropriateness by an expert committee consisting of five experts from each of the following fields: physicians specializing in medical safety, home health care physicians, home health care nurses, medical safety researchers, medical safety management pharmacists, scale development researchers, psychiatric nurse researchers, and administrative staff (statisticians). The experts gathered to discuss, confirm, and revise each item’s content after factor analysis.
2.7 Factorial Validity
An exploratory factor analysis (principal factor analysis, Promax rotation) was performed to determine the factor structure of the PSS-CP. Following the factor analysis, items with a factor load of 0.5 or higher were selected to reduce the number of questions.
2.8 Criterion-Related Validity
The GHQ-12, a concise version of the General Health Questionnaire (GHQ), was used to evaluate the criterion-related validity. Developed by Goldberg [19], it is used to assess one’s mental health and is an effective screening tool for identifying mental disorders. A Japanese version of the GHQ-12 was developed by Nakagawa and Daibo [20], and its reliability and validity have been verified by Niiro and Mori [21].
To investigate the relationship between the number of catheters and stress, the total PSS-CP score was calculated for each participant’s number of catheters inserted and compared using a t-test.
2.9 Reliability Testing
The internal consistency (Cronbach’s α coefficient) and the test-retest method were utilized for reliability testing. SPSS Ver. 28 for Windows was used for the analysis. The retest was conducted during the period from one week (lower limit) to several months (upper limit) following the first test [22].
2.10 Ethical Considerations
The study’s purpose, research plan, methodology, privacy protection policy, transparency of research outcomes, and any vested interests or conflicts of interest due to research collaborations were explained to the participants before their consent for participation was sought. We requested patients to cooperate only after their consent was received. This study was approved by the relevant institutional ethics committee (approval no. 2017-0111-2).
3. Results
3.1 Patient Background
Of the 87 survey forms distributed, 47 responses were received (54.02% response rate). Of these, 44 (93.6%) were deemed valid. Three invalid questionnaires were excluded: two because the respondent’s age was unclear and one because the majority of questions were unanswered.
Table 1 presents participants’ characteristics. The most common type of tubing used was a urinary catheter (n = 16). Twelve (27.3%) respondents had experienced either self-dislodgement or spontaneous dislodgement. The average time spent in home-based care was 44.96 months and the average time with tube/catheter was approximately 44.08 months.
Table 1: Participants’ characteristics
|
Attributes |
Cancer (n=8) |
Non-cancer (n=36) |
P-value |
|
|
Gender (n, Male/Female) |
3-May |
21/15 |
1 |
|
|
Age (years, Mean, SD) |
73.4 (9.9) |
72.0 (14.6) |
0.759 |
|
|
Time spent in home care (months, Mean, SD) |
18.8 (14.1) |
50.8 (66.8) |
0.014 |
|
|
Time spent using tube/catheter (months, Mean, SD) |
19.0 (13.9) |
49.7 (67.5) |
0.019 |
|
|
Previous history of tube/catheter dislodgement (n, %) |
1 (12.5) |
11 (30.6) |
0.413 |
|
|
Tube/catheter type a (n, %) |
Urinary catheter |
1 (12.5) |
15 (41.7) |
0.224 |
|
Oxygen cannula |
1 (12.5) |
12 (33.3) |
0.42 |
|
|
IVHb |
2 (25.0) |
4 (11.1) |
0.297 |
|
|
Parenteral nutrition tube |
1 (12.5) |
4 (11.1) |
1 |
|
|
Othersc |
3 (37.5) |
5 (13.9) |
0.145 |
a As multiple tube/catheter types may be inserted in each patient, the total ratio may exceed 100%.
b IVH: Intravenous Hyperalimentation
c Others: There were two cases each of nephrostomy tubes, peripheral venous catheters, and enterostomy tubes, and one using an indwelling bladder catheter with a balloon.
3.2 Content Validity Testing
Seven screeners (one patient safety specialist physician, one home healthcare physician, one pharmacist, one patient safety researcher, one home-visit nurse, one psychiatric nursing researcher, and one administrative clerk who did statistical analyses) scrutinized questions for the scale measuring tube/catheter-related stress and determined that no further revisions were necessary.
3.3 Factorial Validity Testing
Four factors were derived from the factor analysis (Table 2), with a cumulative contribution ratio of 83.17%. The first factor comprised six items with high factor loadings: Q7 “I feel that the tube is bothersome when I’m moving (walking or in a wheelchair),” Q8 “I’m afraid something will go wrong with the tube when I’m moving (walking or in a wheelchair),” Q9 “I’m worried about the tube when I’m moving (walking or in a wheelchair),” Q10 “I feel that the tube is bothersome when I’m in the toilet,” Q11 “I’m afraid something will go wrong with the tube when I’m in the toilet,” and Q12 “I’m worried about the tube when I’m in the toilet.” Based on these items, the first factor was labeled “Anxiety about catheter dislodgement while moving or in the toilet.”
Table 2: Factor Analysis of the PSS-CP a (N=44)
|
No. |
Questionnaire items |
Factor Load |
Scoreb (Mean ± SD) |
|
Factor 1: Anxiety about catheter dislodgement while moving or in the toilet |
|||
|
1 |
I feel that the tube is bothersome when I’m in the toilet |
0.948 |
3.2±1.8 |
|
2 |
I’m worried about the tube when I’m in the toilet |
0.869 |
3.2±1.8 |
|
3 |
I’m afraid something will go wrong with the tube when I’m in the toilet |
0.864 |
3.1±1.7 |
|
4 |
I’m worried about the tube when I’m moving (walking or in a wheelchair) |
0.862 |
4.0±1.7 |
|
5 |
I feel that the tube is bothersome when I’m moving (walking or in a wheelchair) |
0.781 |
4.1±1.8 |
|
6 |
I’m afraid something will go wrong with the tube when I’m moving (walking or in a wheelchair) |
0.77 |
3.8±1.8 |
|
Factor 2: Anxiety about tube dislodgement when resting or lying down |
|||
|
7 |
I’m afraid something will go wrong with the tube when I’m sleeping/lying down |
0.973 |
3.0±1.9 |
|
8 |
I’m worried the tube will shift when I’m sleeping/lying down |
0.915 |
3.2±1.9 |
|
9 |
I’m afraid of the tube not being securely in place |
0.695 |
2.7±1.7 |
|
10 |
I feel that the tube is bothersome when I’m sleeping/lying down |
0.606 |
3.3±2.0 |
|
Factor 3: Anxiety about tube dislodgement while dressing/undressing |
|||
|
11 |
I’m worried about the tube when I’m getting dressed/undressed |
1.003 |
3.6±1.8 |
|
12 |
I feel that the tube is bothersome when I’m getting dressed/undressed |
0.882 |
3.6±1.9 |
|
13 |
I’m afraid something will go wrong with the tube when I’m getting dressed/undressed |
0.732 |
3.0±1.7 |
|
14 |
I’m worried I’ll get skin problems because of the tube |
0.592 |
3.2±1.9 |
|
Factor 4: Anxiety about tube dislodgement while bathing |
|||
|
15 |
Sometimes I skip bathing because of the tube |
0.748 |
2.8±1.7 |
|
16 |
Because of the tube, I find it difficult to take a bath |
0.665 |
3.9±1.8 |
|
Total |
53.8±21.1 |
||
Factor extraction method: The principal factor method
Rotation method: Promax method with Kaiser's normalization
The rotation converged after 7 iterations.
aPSS-CP: Psychological Stress Scale for Catheterized Home Healthcare Patients
bSix-point scale, ranging from 1 to 6, with a higher score indicating higher stress.
The second factor comprised four items with high factor loadings: Q4 “I’m worried the tube will shift when I’m sleeping/lying down,” Q5 “I’m afraid something will go wrong with the tube when I’m sleeping/lying down,” Q6 “I feel that the tube is bothersome when I’m sleeping/lying down,” and Q21 “I’m afraid of the tube not being securely in place.” Based on these items, the second factor was labeled “Anxiety about tube dislodgement when resting or lying down.”
The third factor comprised four items with high factor loadings: Q1 “I’m worried about the tube when I’m getting dressed/undressed,” Q2 “I’m afraid something will go wrong with the tube when I’m getting dressed/undressed,” Q3 “I feel that the tube is bothersome when I’m getting dressed/undressed,” and Q19 “I’m worried I’ll get skin problems because of the tube.” Based on these items, the third factor was labeled “Anxiety about tube dislodgement while dressing/undressing.”
The fourth factor comprised two items with high factor loadings: Q13 “Because of the tube, I find it difficult to take a bath,” and Q15 “Sometimes I skip bathing because of the tube.” Based on these items, the factor was labeled “Anxiety about tube dislodgement while bathing.”
3.4 Criterion-Related Validity Testing
For the criterion-related validity testing, Pearson’s product moment correlation coefficients with GHQ-12, which measured the generalized anxiety, were calculated for the four factors of PSS-CP (Table 3). Regarding tube/catheter-related generalized anxiety, correlations were found for each factor, as follows: the first factor (r=.659, p<0.01), second factor (r=.555, p<0.01), third factor (r=.628, p<0.01), and fourth factor (r=.369, p<0.05). Regarding pain/discomfort, correlations with the first factor (r=.365, p<0.05) and third factor (r=.369, p<0.05), as well as an overall correlation (r=.364, p<0.05), were found. Regarding GHQ-12, a correlation was established for the first factor (r=.492, p<0.05) and third factor (r=.350, p<0.05), and overall correlation (r=.436, p<0.01) was also noted.
Table 3: Reliability and correlation coefficients for each factor (N=44)
|
Factor a |
Cronbach’s α |
Pearson's product-moment correlation coefficient (R) |
||||
|
Internal Consistency |
Test-retest method |
Generalized anxiety b |
Pain/Discomfortb |
GHQ-12c |
||
|
1 |
0.949 |
0.760** |
0.659** |
0.365* |
0.492** |
|
|
2 |
0.92 |
0.712** |
0.555** |
0.235 |
0.267 |
|
|
3 |
0.878 |
0.549* |
0.628** |
0.343* |
0.350* |
|
|
4 |
0.796 |
0.757** |
0.369* |
0.174 |
0.198 |
|
|
Total |
0.943 |
0.791** |
0.710** |
0.364* |
0.436** |
|
a Factors: 1 – anxiety about catheter dislodgement while moving or in the toilet; 2 – anxiety about tube dislodgement when resting or lying down; 3 – Anxiety about tube dislodgement while dressing/undressing; 4 – anxiety about tube dislodgement while bathing
b 6-item method
c General Health Questionnaire
* p < 0.05, ** p < 0.01
Factor extraction method: Principal component analysis
Rotation method: Promax method with Kaiser Normalization
The PSS-CP score (Mean, 95% CI) was 52.2 (45.8, 58.6) and 76.4 (68.6, 84.2), p = 0.004. The number of inserted tubes/catheters was 1 in 41 and 2 in 3. The majority of the patients (n = 32) had no history of tubing/catheter dislodgement, and the PSS-CP scores (Mean, 95% CI) showed with history of tub-ing/catheter dislodgement as 56.3 (45.8, 66.9) and without history of tubing/catheter dislodgement as 52.9 (45.2, 60.6), p = 0.612, respectively. Non-cancer patients had significantly higher PSS-CP scores than cancer patients when compared by disease (Table 4).
Table 4: Comparison between cancer and non-cancer patients
|
Factor |
PSS-CP Score (Mean, 95%CI) |
P-value (t-test) |
|
|
Cancer (n=8) |
Non-cancer (n=36) |
||
|
1 |
13.9 (5.5, 22.3) |
23.2 (20.6, 25.7) |
<.001 |
|
2 |
9.8 (4.4, 15.1) |
12.8 (10.7, 14.9) |
<.001 |
|
3 |
11.0 (2.6, 16.2) |
13.9 (11.9, 15.8) |
.003 |
|
4 |
6.4 (3.9, 8.9) |
6.8 (5.8, 7.9) |
.590 |
|
Total |
41.1 (23.1, 59.0) |
56.7 (50.4, 63.0) |
<.001 |
3.5 Reliability Testing
For reliability testing, an internal consistency analysis (Cronbach’s α coefficient) was performed (Table 3). The coefficients for the first, second, third, and fourth factors were 0.946, 0.92, 0.878, and 0.796, respectively. The coefficient derived for the entire scale was 0.943. The test-retest method indicated a highly significant correlation (r = 0.791, p < 0.01).
4. Discussion
The purpose of this study was to develop a stress scale for patients using tubing catheters. Importantly, 16 items across four factors on tube/catheter-related stress were identified, covering items such as psychological and physical distress in daily life activities.
The sixth items in the first factor (i.e., “anxiety about catheter dislodgement while moving or in the toilet”) allude to the basic human needs of “eliminating body wastes” and “moving the body’s position and maintaining body postures (movements),” as indicated in Henderson’s need theory [23]. When humans attempting to satisfy those needs face obstructions or inconvenience, they become highly stressed. Particularly, in terms of mobility, when certain behaviors (movements) are restricted to a certain degree due to tubes/catheters, such limitations become, in a sense, quasi-physical restraints. Physically restrained humans are reportedly prone to psychological reactions such as anger, anxiety, and fear [24]. Hence, it can be inferred that catheterized patients likely experience similar feelings and are thereby subject to stress. Therefore, we believe that the second factor is strongly correlated with the item on “general anxiety” about tubing and catheters because of a sense of restraint. Further, psychological influences may also be observed in the high correlation of the current scale with the GHQ-12.
In the fourth item of the second factor (i.e., “anxiety about catheter dislodgement when resting or lying down”), anxiety about dislodgement related to sleep and rest, including unconscious events when lying down, was extracted. From these items, we identified the presence of anxiety about possible dislodgement while the patient is unconscious. Sleep/rest is one of the basic human needs in Henderson’s need theory [23]. When sleep or rest is impeded by some disturbance, sleep quality deteriorates. Moreover, sleep exerts a strong influence on how a person responds to mental stress [25]. Moreover, anxiety during sleep or rest impairs sleep and may lead to depression. A cohort study of the correlation between insomnia and depression in present-day Japan reported that, compared to individuals devoid of sleep problems, the odds ratio of depression in those afflicted with sleep disorders was 1.59 [26].
The fourth item of the third factor was extracted as a sense of stress when putting on and taking off clothes. Regarding dressing and undressing, a previous study reported that catheterized patients who experience difficulties in daily life arrange their clothing to accommodate the catheter [27], suggesting that catheters can be a stressor during dressing/undressing. Additionally, skin problem items were extracted. Skin problems can be physically painful, and it has been posited that physical pain is closely linked with psychological stress [28]. When organ injury or inflammation is accompanied by pain, it is believed that psychological stress co-occurs with physical stress [29]. Therefore, it can be inferred that dermatological and similar disorders induced by catheterization entail both psychological and physical pain. This is the reason for the strong correlation with “general anxiety” about the tube and with GHQ-12 scores.
The fourth factor, “anxiety about catheter dislodgement while bathing,” consists of two items. As one of the basic human needs cited by Henderson [23], bathing has also been reported to be efficacious in bringing about mental relaxation that assuages bodily fatigue [30]. When a person is prevented from bathing by some particular impediment, stress arises. The fourth factor was strongly correlated with the item about “general anxiety” about tubing/catheters because tubing/catheters can be a disincentive to bathing, and there is a possibility of accidental dislodgement during bathing.
The next salient aspect of this study is the establishment of the reliability and validity of the scale. The internal consistency analysis (Cronbach’s α coefficient) of the scale showed coefficients ranging from 0.796 to 0.949 for the four factors, and although the third factor had a low coefficient, the entire scale had a coefficient of 0.943. Moreover, the test-retest method yielded a significant correlation, and accordingly, the scale was deemed reliable.
As for the scale’s validity, a significant correlation between generalized anxiety and pain/discomfort was noted, as well as between the PCC-CP and the GHQ-12. On this basis, we judged the scale to be valid. The PSS-CP score was higher when the number of tubes/catheters used was increased, which indicates that this scale is valid. It is possible to assume that the use of multiple tubing/catheters may limit activities and increase anxiety more than the use of a single catheter.
Regarding the other characteristics, by disease, the non-cancer group had a higher score than the cancer group. The non-cancer group included 10 cases of designated intractable diseases. These diseases are associated with a decline in physical functions and activities of daily living, although there are individual differences. We believe that this symptom characteristic of the designated intractable diseases is one of the reasons for the higher values in the cancer group. In the future, we believe that it is necessary to accumulate more sample data and conduct a detailed analysis of the disease.
Arguably, there should be separate instruments for each tube/catheter type and disease. However, we prioritized the development of a generic scale, as home healthcare can involve any kind of disease. As this study was limited by the fact that only validity and reliability tests were performed, further studies are needed. Although the reproducibility of each factor’s independent use in this scale was established using the test-retest method, each factor’s reproducibility with respect to each tube/catheter type may not have been adequately investigated. Having said that, capitalizing on this PSS-CP, further studies on prevention of accidental dislodgement and improvement of the quality of home healthcare are needed.
However, despite these limitations, a more objective apprehension of the stress weighing on catheterized patients has been facilitated by this study, potentially leading to its utilization in preventing self-dislodgement and ameliorating QOL. Those with a high stress score are likely to dislodge the tube/catheter by themselves; therefore, using the scale to aid in developing clinical interventions for discontinuing the use of tubes/catheters and alleviating stress may help prevent accidental dislodgement. The scale would be particularly valuable as a preventive tool in cases where dislodgement would endanger life or diminish QOL, such as cases involving injectable narcotics or central venous nutrition. It is necessary to develop preventive strategies involving inter-professional teams comprising doctors, pharmacists, nurses, etc. and to establish procedures for effective interprofessional communication.
5. Conclusions and Relevance
This study attempted to construct a PSS-CP, culminating in a four-factor scale whose reliability and validity were both duly corroborated. A factor analysis of the scale items for measuring stress from tubes and catheters extracted 16 items across four factors. This study newly showed that the PSS-CP score was higher in non-cancer than cancer patients and that mental stress caused by the intubation was greater as the number of intubation increased. Consequently, research on mental stress as an outcome and a clinical consideration, especially for patients in a home healthcare setting, should be taken into account.
Acknowledgements
This study was supported by the Yuumi Memorial Foundation for Home Health Care. We would like to express our gratitude to the home care clinic and home nursing station that cooperated with our study.
Conflict of Interests
There is no conflict of interest to declare.
References
- Hayashi Y, Nakano Y. Patient Safety and Quality of Medical Care. Topics: I. Incident and Accident in Hospital: Current Situation; 5. Frequency and Prevention of Medical Near-Miss/Adverse Event Related to Use/Management of Drainage Tube or Other Tubes. Nihon Naika Gakkai Zasshi 101 (2012): 3404-3412.
- Alivizatos V, Gavala V, Alexopoulos P, Apostolopoulos A, Bajrucevic S. Feeding Tube-Related Complications and Problems in Patients Receiving Long-Term Home Enteral Nutrition. Indian Journal of Palliative Care 18 (2012): 31-33.
- Japan Council for Quality Health Care-Certified Hospital Patient Safety Promotion Council Procedures/Tube Troubles Section. Recommended Prevention Measures Against Self-Dislodgement (Accidental) of Tubes etc. in Patients. J Patient Saf Promot (2007): 4-5.
- Japan Council for Quality Health Care Project to Collect Medical Near-Miss/Adverse Event Information. 2018 Annual Report. Accessed February 1, (2020).
- Ohta M, Miyamoto Y, Ito H. Current Status of Medical Accidents Involving Elderly Patients. Geriatric Medicine 46 (2008): 99-104.
- Oguro K, Jirei P. Opioid Switching in Home Care: A Case of Success. Japanese Journal of Community Medicine and Pharmaceutical Sciences 6 (2019): 27-29.
- Shiraishi T, Kaibara T, Kushida K. Pharmacy's Involvement in Discharge Coordination and Patient Support for Patients Who Use Injectable Narcotics. Japanese Journal of Cancer and Chemotherapy 37 (2010): 180-182.
- Hamada S, Komatsu S, Shibata R, et al. Better Effect of Home Night Enteral Nutrition in an Elderly Patient Following Laparoscopic Total Gastrectomy for Advanced Gastric Cancer. Gan To Kagaku Ryoho 47 (2020): 2030-2031.
- Hotta M, Araki M, Urano A, Ohwada R. Home Parenteral Nutrition Therapy in Seven Patients with Anorexia Nervosa: The Role and Indications. Internal Medicine 53 (2014): 2695-2699.
- Nikaidou K, Shinohara Y, Matsumura S, Kinoshita Y. Incident/accident at Visiting Nurse Service and their prevention/countermeasures : From the study at Visiting Nurse Service Station in N city 3 years after the enforcement of the Care Insurance Act. Bulletin of Niigata Seiryo University 4 (2004): 237-261.
- Okamoto T, Tsunajima T, Tsurumaki K, et al. Implementation and Practice to Reduce Accidents to as Close to Zero as Possible: Initiatives for Infusion Routes, Tubing, and Surgical Groups. The Japanese Journal of Clinical Nursing, Monthly 27 (2001): 1532–1543.
- Kikuchi M, Jyoko N, Amemiya C. Case Analysis of Self-Dislodgement of Lines. Repository of the Department of Nursing, Tokyo Medical University Hospital 25 (2005): 71-74.
- Kurayashiki M, Takama S. Distress in Patients Receiving Continuous Infusion. Proceedings of the Japan Society of Nursing 43 (2013): 27-30.
- Lee T-Y, Chen H-H, Yeh M-L, Li H-L, Chou K-R. Measuring Reliability and Validity of a Newly Developed Stress Instrument: Newly Diagnosed Breast Cancer Stress Scale. Journal of Clinical Nursing 17-18 (2013): 2417-2425.
- Sumiyoshi K, Kawata C, Okamoto T, et al. Development of the Treatment-Induced Stress Perception Scale for Diabetics. Journal of the Okayama Medical Association 129 (2017): 93-99.
- Arai Y, Tamiya N, Yano E. The Short Version of the Japanese Version of the Zarit Caregiver Burden Interview (J-ZBI_8): Its Reliability and Validity. Nihon Ronen Igakkai Zasshi 40 (2003): 497-503.
- Iida N, Kohashi N, Okamura T, Nagao K. Reliability and Validity of the New Assessment of the Burden on Caregivers (ABC-16). Japanese Journal of Geriatrics 42 (2005): 209-213.
- Tasaki K, Shin J. Japanese Response Bias: Cross-Level and Cross-National Comparisons on Response Styles. The Japanese Journal of Psychology 88 (2017): 32-42.
- Goldberg D. The Detection of Psychiatric Illness by Questionnaire. Oxford: Oxford University Press, London (1972): 257-264.
- Goldberg D. A Guide to the GHQ Psychological Well-Being Survey., ed. by Nakagawa Y, Daibo I, Nihon Bunka Kagakusha (2013): 69-80.
- Niiro M, Mori T. Development of a Shortened Version of the Japanese Version of the Zarit Care Burden Scale (J-ZBI_8): A Study of Its Reliability and Validity. Seishin Igaku 43 (2001): 431-436.
- Hasegawa H. On the Relationship between Recognition Memory of Items and Test–Retest Effect. The Japanese Journal of Psychology 68 (1997): 417-422.
- Virginia H. Basic Principles of Nursing Care. Amer Nurses Pub, California (1997).
- Strumpf N, Evans L. Physical Restraint of the Hospitalized Elderly: Perceptions of Patients and Nurses. Nursing Research 37 (1988): 132-137.
- Shimura A, Tanaka T, Misaki S, et al. Sleep Exerts a Major Influence on Stress Check Results. Seishin Igaku 60 (2018): 783-791.
- Yokoyama E, Kaneita Y, Saito Y, et al. Association between Depression and Insomnia Subtypes: A Longitudinal Study on the Elderly in Japan. Sleep 33 (2018): 1693-1702.
- Yamada M, Uchiyama M. Physical Restraint of the Hospitalized Elderly: Perceptions of Patients and Nurses. Proceedings of the Japan Society of Nursing, Acute Nursing 50 (2020): 67-70.
- Senba E. The Mechanism of Stress-Aggravated Pain. Japanese Journal of Pharmaceutical Palliative Care and Sciences 3 (2010): 73-84.
- Senba E, Ueyama T. Stress-Induced Expression of Immediate Early Genes in the Brain and Peripheral Organs of the Rat. Neuroscience Research 29 (1997): 183-207.
- Wada Y, Takamura M, Yamazaki M, Suzuki A. Measurement of the Bathing Effect by a Psychological Scale and Chromogranin A levels During Sleep: A Comparison between the Young and the Elderly. Health Sci University Bull 7 (2011): 85-96.