Correlation between ECG Changes and Coronary Angiographic Findings in Patient with Inferior Myocardial Infarction in a Tertiary Care Hospital
Article Information
Shaikh Md. Shahidul Haque1*, Mohammad Morshedul Ahsan1, Alok Chandra Sarker1, Md. Shahadat Hossain1, Md. Shahriar Kabir1, Abu Baqar Md. Jamil1
1Department of Cardiology, Shaheed Ziaur Rahman Medical College & Hospital, Bogura, Bangladesh
*Corresponding author: Shaikh Md. Shahidul Haque, Department of Cardiology, Shaheed Ziaur Rahman Medical College & Hospital, Bogura, Bangladesh.
Received: 09 Febraury 2023; Accepted: 17 Febraury 2023; Published: 23 March 2023
Citation: Shaikh Md. Shahidul Haque, Mohammad Morshedul Ahsan, Alok Chandra Sarker, Md. Shahadat Hossain, Md. Shahriar Kabir, Abu Baqar Md. Jamil. Correlation between ECG Changes and Coronary Angiographic Findings in Patient with Inferior Myocardial Infarction in a Tertiary Care Hospital. Cardiology and Cardiovascular Medicine. 7 (2023): 90-96.
View / Download Pdf Share at FacebookAbstract
Background: In patients with coronary artery disease, abnormalities in 12 leads Electrocardiography (ECG) are often used to localize the anatomic site of myocardial infarction and ischemia. The same ECG findings are often used to corelate with anatomy of coronary arteries and as well as the site of occlusion. The determination of infarct related artery in acute inferior MI is extremely important for prediction of amount of myocardium at risk and guide decisions regarding urgency of revascularization which might have positive impact on mortality and morbidity. But we do not have enough research-based information regarding the correlation of ECG changes with CAG findings in acute inferior myocardial infarction.
Aim of the Study: Our objective of the study was to identify the infarct related artery either right coronary artery (RCA) or left circumflex artery (LCX) in acute inferior myocardial infarction using ECG criteria and comparing with coronary angiographic findings.
Methods: The prospective observational study was conducted in the department of Cardiology, Shaheed Ziaur Rahman Medical College & Hospital, Bogura, Bangladesh during the period from July 2020 to June 2022. In total 185 patients with acute inferior myocardial infarction by ECG criteria were enrolled in this study as the study subjects. The ECG of these patients evaluated for significant ST segment elevation in inferior leads and comparing the ST elevation of lead III exceeding in Lead II plus ST segment depression >1 mm in lead aVL as a prediction of right coronary artery occlusion. If criteria were negative, LCX occlusion was likely. Proper written consent was taken from all the participants before data collection. For all the participants, either symptomatic or silent coronary angiography (CAG) was done within 4-6 weeks after an event to identify the culprit artery and also to see the non-culprit artery. Then ECG changes in various leads were used to localize the vessels involve and were correlated with dominant vessels involved in coronary angiography in development of inferior MI. All data were processed, analyzed and disseminated by using MS excel and SPSS version 23 program as per necessity.
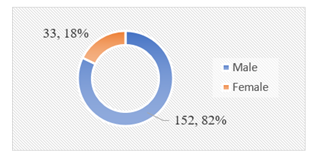
Results: The study population consists of 185 patients (152 male and 33 female) with mean ± SD age of 48.45 ±13.79 years. Among our participants, IRA disease burden were found 90%; in 70% RCA and in the rest 20% LCX were the culprit artery. On the other hand, non-IRA burden was 63%. In this study, as per the angiographic findings among our participants we observed that, cases with RCA, ‘RCA + LCX’, and ‘LAD + RCA + LCX’ were found in 20%, 23% and 28% respectively which were remarkable. Besides these, cases with LCX, ‘LAD + RCA’, ‘LAD + LCX’ and LM (Only) were found 5%, 8%, another 5% and 3% respectively whereas cases with normal vessels were found 10%. Finally, in assessing the vessel involvement we found DVD in more than one third (35%) of total patients. Besides this, cases with SVD and TVD were found in 28% and 26% respectively.
Conclusion: It is possible to predict the culprit artery whether right coronary artery or left circumflex artery by examining the surface electrocardiography in patient with inferior myocardial infarction. A higher ST segment elevation in lead III than in lead II and deeper ST segment depression in aVL of surface ECG is the most useful parameters for predicting the RCA culprit artery in acute inferior wall myocardial infarction.
Keywords
AMI (Inferior); Coronary Angiography (CAG); Correlation; Culprit Artery; ECG; Infarct related Artery (IRA)
AMI (Inferior) articles; Coronary Angiography (CAG) articles; Correlation articles; Culprit Artery articles; ECG articles; Infarct related Artery (IRA) articles
Article Details
1. Introduction
Coronary artery disease is a worldwide health epidemic. Worldwide 30 percent of all deaths can be attributed to cardiovascular disease of which more than half are caused by coronary heart disease. Globally of those dying from cardiovascular disease, 80 percent are in developing countries [1]. By 2020, cardiovascular disease will cause one of every three deaths worldwide. Coronary heart disease is the leading cause of cardiovascular disease. Every minute an American dies of coronary artery disease. About 38 percent of people experience an acute coronary event. Acute myocardial infarction (AMI) is one of the most common presentations of CAD [2]. Acute STEMI carries about 4-12% risk of death on admission despite in-hospital optimum medical management [3]. Primary percutaneous coronary intervention (PCI) in acute STEMI provides better survival benefit than medical management [4,5,6]. But number of primary PCI is much less in Bangladesh even in highly specialized cardiac centers [7]. Most of the medical college hospitals in Bangladesh are still lacking in logistic and manpower support for primary PCI in timely fashion. Provision of pharmaco-invasive therapy for this group of patients also a difficult task in most of the peripheral hospitals. The global burden of disease study suggests that, by 2020, this part (South Asian countries) of the world will have more people with atherosclerotic coronary artery disease (CAD) than in any other region [8]. Data related to different aspects of coronary artery disease (CAD) in Bangladesh are inadequate but it is highly prevalent in Bangladesh [9]. The electrocardiogram or ECG continues to be the primary clinical test in patients with suspected acute coronary syndromes (ACS) [10]. Recently there has been an increased focus on the accuracy of the electrocardiogram interpretation on the misinterpretation rate as well as on the false positive and false negative cath lab activation rates [10]. But, Jayroe et al [11] distributed difficult ECGs to 15 ‘‘expert’’ electro-cardiographers, with a clinical scenario suggestive of ischemia. There were in total 108 nonischemic ECGs with STE of various causes and eight STEMIs; mean sensitivity and the specificity of the readers were 75 % and 85 % respectively which was similar to Turnipseed’s 2005 study [12] in which neither emergency physicians nor cardiologists performed well to differentiate early repolarization from STEMI. Shu-Fen Wung and colleagues [13] have shown that ST-segment elevation in the right ventricular leads and inferior leads occurred more often during occlusion of the RCA than during the occlusion of the circumflex artery. They further concluded that ST-segment depression in lead aVL is highly suggestive of right coronary occlusion, whereas ST-segment elevation in posterior leads without depression of the ST segment in lead aVL is highly sensitive and specific for occlusion of the left circumflex artery. Mamun KSA et all [14] found that ST segment elevation in Lead III exceeding the Lead II and ST segment depression >1 in aVL had a high sensitivity and specificity for RCA occlusion. Gupta et all [15] conducted a study which showed ST segment elevation was greater in Lead III than Lead II when RCA was the culprit vessel and vice versa when LCX was the culprit vessel (P< .001). These criteria had a sensitivity of 99% and specificity of 100% for diagnosing RCA as the culprit vessel. When STE in Lead II was higher than Lead Ill with a sensitivity 93% and specificity of 100% in identifying the LCX as the culprit vessel. Coronary angiography provides prognostic information valuable in risk assessment and treatment decisions. In acute inferior myocardial infarction, the infarct related artery is usually the right coronary artery (RCA), less often the left circumflex coronary artery (LCX) and rarely the “wrapped” left anterior descending artery [LAD] [16]. The incidence of mortality and complications are high in patients of acute inferior wall MI with right ventricular involvement. In the presence of complications (hypotension, bradycardia, right heart failure, shock and arrhythmias etc.), right coronary artery (RCA) is generally the infarct related artery [17]. The ECG is noninvasive, affordable, easily available and essentially without any known adverse effects. ECG is generally used to diagnose myocardial infarction. However, it can also be used to predict the culprit artery in patients with myocardial infarction. Early prediction of infarct related artery by ECG can recognize the amount of myocardium at risk and guide decisions regarding urgency of revascularization. Urgent decision may facilitate management and prevention of complication. Although coronary angiography is the ‘’gold standard’’ for determination the infarct-related artery in acute myocardial infarction, the ECG can be a useful tool in identifying which artery is involved at the first point of care. We can confirm the ECG prediction by angiogram. In many Centers of our country, early intervention is not possible. By examining ECG, we can predict the infarct related artery and upcoming complications. For these groups, we can refer them to a center where early revascularization facility is present.
2. Methodology
2.1 Patients
It was a prospective, observational study. The study population consisted of patients with a diagnosis of acute inferior myocardial infarctions, who were admitted to coronary care unit, Department of Cardiology of Shaheed Ziaur Rahman medical college hospital between July 2020 and June 2022 and who subsequently underwent coronary angiography within 4-6 weeks. A total of 185 patients with acute inferior myocardial infarction were included in this study. Proper written consents were taken from all the participants before data collection. The whole intervention was conducted in accordance with the principles of human research specified in the Helsinki Declaration [18] and executed in compliance with currently applicable regulations and the provisions of the General Data Protection Regulation (GDPR) [19]. A patient with acute inferior myocardial infarction were recognized first from history, examination and ECG. Other history was taken from the patients regarding age, sex, hypertension, diabetes, smoking and other risk factors. A patient with acute inferior STEMI with or without right ventricular infarction (RVI) or posterior MI who received medical management only and who experienced recurrent episodes of angina or angina equivalent at rest or with exertion following discharge from hospital were included in this study. A diagnosis of inferior wall AMI was made on the basis of: chest pain lasting > 30 min; ST segment elevation > 1 mm in at least two of the three inferior leads (II,III and aVF); and elevation or fall of Troponin-I. Patients with a history of previous AMI or double wall AMI, severe left ventricular systolic dysfunction ( LVEF<30%), hemodynamically unstable patient, patient with significant renal impairment (serum creatinine > 1.5 mg/dl), unwilling to undergo revascularization strategy, known dye hypersensitivity, elderly patients age > 75yrs, patient with severe valvular and congenital heart disease, dependent on pacemaker, prior coronary angioplasty showing ECG evidence of bundle branch block or left ventricular hypertrophy were excluded from the study.
2.2 ECG
Standard twelve leads electrocardiography were recorded at a paper speed 25 mm/s with amplitude of 10 mm/mv, any ST segment deviation from isoelectric line (T-P segment) was measured to nearest 0.5mm at 80 msec after the J point. Serial ECGs performed on admission, within 6 hr of the onset of chest pain. The following ECG changes were assessed: ST-segment elevation in lead III exceeding that in lead II, defined as ratio of ST elevation in lead III/elevation in lead II>1, ST segment depression in lead aVL defined as >1 mm deviation from the isoelectric line.
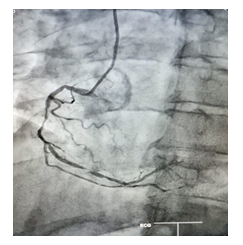
2.3 Coronary Angiography
The coronary angiography was done by percutaneous Judkin`s technique via femoral route in Cath lab, department of cardiology, SZMCH to identify the culprit artery. Coronary angiography was performed between 4 weeks and 6 weeks after the infarction. Coronary angiography films were reviewed by two cardiologists who were blinded to the ECG findings. The infarct related artery was identified from total occlusion or significant stenosis (>70%) of the RCA or LCX or their major branches, or from arteriographic evidence of intraluminal thrombosis. The stenosis >50% was considered as the diseased coronary artery. In coronary angiography- when both RCA and LCX are severely diseased, however deciding which one is the culprit can be difficult in that case dominant vessel involvement and ECG criteria were used to localize the vessel involved in developing acute inferior wall myocardial infarction. All data were processed, analyzed and disseminated by using MS Excel and SPSS version 23 program as per necessity.
3. Result
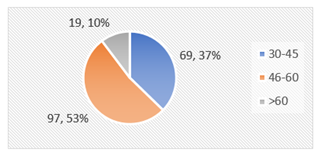
In this study, among total 185 participants, majority were from 46-60 years’ age group which was 53%. Besides this, 37% patients were from 30-40 years’ age group and the rest 10% were from >60 years’ age group. Among total participants, male patients were 82% and female patients were 18%. In analyzing the risk factors among the participants, we observed that, in 48% cases smoking and in 45% cases DM were the risk factors. Besides these, dyslipidemia and HTN were found in 30% and 41% cases as the risk factors respectively. As per our inclusion criteria of this study and ECG screening, all of our participants were with MI. The mean ±SD ejection fraction (EF) of total participant was fond as 57.83±9.37%. In this study, as per the angiographic findings among our participants we observed that, cases with RCA, ‘RCA + LCX’, and ‘LAD + RCA + LCX’ were found in 20%, 23% and 28% respectively which were remarkable. Besides these, cases with LCX, ‘LAD + RCA’, ‘LAD + LCX’ and LM (Only) were found 5%, 8%, another 5% and 3% respectively whereas cases with normal vessels were found 10%. Finally, in assessing the vessel involvement we found DVD in more than one third (35%) of total patients. Besides this, SVD and TVD were found 28% of cases. Among our participants, IRA disease burden were found 90%; in 70% RCA and in the rest 20% LCX were the culprit artery. On the other hand, non-IRA burden was 63%.
|
Risk factors |
Number (n) |
Percentage (%) |
|
Smoking |
88 |
48% |
|
DM |
84 |
45% |
|
Dyslipidemia |
56 |
30% |
|
HTN |
75 |
41% |
Table 1: Risk factors distribution among participants (N=185).
|
Findings |
Number (n) |
Percentage (%) |
|
ECG STEMI (Inferior) |
185 |
100% |
|
EF (Mean ±SD) % |
57.83±9.37 |
|
Table 2: Findings of ECG and Echo Cardiography among participants (N=185).
|
Diseased artery (≥50% Stenosis) |
(Number (n) |
Percentage (%) |
|
RCA |
37 |
20% |
|
LCX |
9 |
5% |
|
RCA + LCX |
42 |
23% |
|
LAD + RCA |
14 |
8% |
|
LAD + LCX |
9 |
5% |
|
LAD + RCA + LCX |
51 |
28% |
|
LM (Only) |
5 |
3% |
|
Normal |
18 |
10% |
Table 3: Angiographic findings among participants (N=185).
RCA- Right Coronary Artery; LCX- Left Circumflex Artery; LAD- Left Anterior Descending Artery; LM- Left Main (Artery).
|
Vessel involvement |
Number (n) |
Percentage (%) |
|
SVD |
51 |
28% |
|
DVD |
65 |
35% |
|
TVD |
51 |
28% |
|
Normal |
18 |
10% |
Table 4: Vessel involvement among participants (N=185).
SVD- Single Vessel Disease; DVD- Double Vessel Disease; TVD- Triple Vessel Disease.
|
Diseased artery (≥50% stenosis) |
Number (n) |
Percentage (%) |
||
|
IRA |
(RCA as culprit artery) |
129 |
70% |
|
|
(LCX as culprit artery) |
37 |
20% |
||
|
Non-IRA |
With/without IRA lesion |
116 |
63% |
|
Table 5: IRA and Non-IRA disease burden as per CAG findings (N=185).
IRA- Infarct-Related Artery; Non-IRA- Non-Infarct-Related Artery.
4. Discussion
Ischemic heart disease is a major health concern and confers to significant morbidity and mortality throughout the world. It is usually a disease of the elderly, though premature disease can occur in male before 55 years and female before 65 years of age in presence of risk factors for the disease in a particular patient [20]. In general, South Asian people including people of our country do suffer from ischemic heart disease at earlier age than that western people. Even South Asian migrants living in several countries have higher death rates from coronary heart disease (CHD) at younger age compared with the local population despite apparently lower levels of conventional risk factors [21,22]. The aim of this study was to assess the correlation of ECG changes with coronary angiographic findings in acute inferior myocardial infarction. In this study, among total 185 participants, majority were from 46-60 years’ age group which was 53%. Besides this, 37% patients were from 30-40 years’ age group and the rest 10% were from >60 years’ age group. The mean age of our study was comparable to 52±10 years in a study reported by Maqbool Jafary et al [23] in Pakistan and 62±5 years in COURAGE trial [24] and 58±11 years by Fournier et al [25]. In analyzing the risk factors among the participants, we observed that, in 48% cases smoking and in 45% cases DM were the risk factors. Besides these, dyslipidemia and HTN were found in 30% and 41% cases as the risk factors respectively. Diabetes mellitus (T2DM) alone was a risk factor in 7.13% patient and combined with hypertension and diabetes mellitus were been in 22.25% patients [26]. Although in our study T2DM was not found as a major risk factor, diabetes mellitus is well known to have an adverse influence on the prognosis of patients with acute myocardial infarction [23]. In a study [26] 36.13% patients were found as hypertensive. The prevalence of hypertension in South Asian cohort of INTERHEART study [24] (31.1%) is comparatively lower than this study but is similar to 35% in Ahmed et al [27] and Akanda et al [28]. In the present study among 185 patients with acute inferior wall infarction, we found that the IRA/Culprit lesion was RCA in 129 patients (70%) and LCX 37 patients (20%), a ratio of 3.4:1. Other studies of patients with acute inferior MI have found RCA to LCX ratios ranging from 2.2:1 to 7:1 and averaging 3.9:1 [29,30]. Thus, the RCA is much more likely than the LCX to contain the culprit lesion. In this study, as per the angiographic findings among our participants we observed that, cases with RCA, ‘RCA + LCX’, and ‘LAD + RCA + LCX’ were found in 20%, 23% and 28% respectively which were remarkable. Besides these, cases with LCX, ‘LAD + RCA’, ‘LAD + LCX’ and LM (Only) were found 5%, 8%, another 5% and 3% respectively whereas cases with normal vessels were found 10%. Finally, in assessing the vessel involvement we found DVD in more than one third (35%) of total patients. Besides this, in each of the cases groups with SVD and TVD there were 28% patients. All of our findings were found in accordance with some other studies [31,32, 33]. With IWMI, occlusion can be either in the RCA or the LCX coronary artery, and this is in accordance with some other studies [34,35]. In our study 10% of cases, we found normal coronary anatomy. As ischemia was the prime factor for enrollment of the patients in the study; completely normal CAG finding was less likely to observe. This may indicate recanalized RCA or LCX or coronary spasm causing myocardial infarction. In this study RCA appears to be culprit artery in 129 (70%) patients and another 37 (20%) patients LCX appears to be culprit artery which corelate with the study conducting by Kabir et al [36]. Late revascularization of IRA requires pre-procedural careful evaluations in all steps of evaluation. In our center for revascularization of the IRA is to assess the viability of infarcted area by angiographic profile substantiated by classical effort angina or positive ETT and absence of thinned out akinetic, scarred or aneurysmal segment on echocardiography. Doubtful cases were referred to higher center. Of much significance is that 74 (41%) of study population had LAD disease either in the form of DVD or TVD and 5(3%) of study population had Left main disease which correlate with Kabir et al [36]. A total of 116 (63%) patients had non-IRA related ischemic burden. Critical stenosis in a non-IRA vessel needs not much sophisticated evaluation like that of IRA to take a decision for revascularization. Even though primary PCI is not possible to vast majority of patients in our context; early detection of total ischemic burden and there by revascularization of critically diseased and physiologically significant stenoses can provide morbidity & mortality benefit by preventing or reducing post-MI angina and severity or incidence of heart failure and fatal arrhythmias [37].
5. Limitation of the Study
This was a single centered study with small sized samples. Moreover, the study was conducted at a very short period of time. Coronary angiogram was not done immediately on presentation but on later date. It may be sometimes difficult to attribute a lesion as culprit vessel if angiography is done later in the course after thrombolytic therapy or medically treated patients. So, the findings of this study may not reflect the exact scenario of the whole country.
6. Conclusion & Recommendation
It is possible to predict the culprit artery whether right coronary artery or left circumflex artery by examining the surface electrocardiography in patient with inferior myocardial infarction. A higher ST segment elevation in lead III than in lead II and deeper ST segment depression in aVL of surface ECG is the most useful parameters for predicting the RCA as a culprit artery in acute inferior wall myocardial infarction. Detection of residual myocardial ischemia by coronary angiogram following acute MI carries much significance to select patients for revascularization in both non-infarct & infarct related artery to save viable myocardium which can provide great mortality and morbidity benefit to our patients who receive only medical management for acute MI. All of our cases were ECG confirmed patients with myocardial infraction and coronary angiography showed more involvement of RCA culprit arteries along with a good number of LCX culprit arteries in our settings. We found a remarkable number of DVD cases in this study. For getting more specific results we would like to recommend for conducting similar more studies in several places with larger sized samples.
Funding
No funding sources.
Conflict of Interest
None declared.
References
- Kim MC, Kini AS, Fuster V. Definitions of acute coronary syndromes. In: Fuster V, O'Rourke RA,Walsh RA, Poole-Wilson P, editors. Hurst's the Heart. 13th ed. New York, USA: McGraw Hill (2011).
- Bashore TM, Granger CB, Hranitzky P, et al. Coronary heart disease. In: McPhee S, Papakadias MA, editors. Current medical diagnosis and treatment. 49th ed. New York, USA: McGraw Hill (2010): 316.
- Kristensen SD, Laut KG, Fajadct J, et al. European Association for Percutaneous Cardiovascular Interventions. Reperfusion therapy for ST elevation acute myocardial infarctio(!.71/y011: curreM status in 37 ESC countries. Eur Heart J 35 (2014): 1957-1970.
- West RM, Cattle BA, Bouyssie N, et al. Impact of hospital proportion and volume on primary percutaneous coronary intervention performance in England and Wales. Eur Heart J 32 (2011): 706-711.
- Zijlstra F, Hoorntje JC, Boer MJD, et al. Long-term benefit of primary angioplasty as compared with thrombolytic therapy (Al acute myocardial infarction. N Engl J Med 341 (1999): 1413-1419.
- Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomized trials. Lancet 361 (2003): 13-20.
- Cader FA, Haq MM, Nasrin S, et al. Presentation, Management Practices And in-hospital Outcome of Patients with Acute Coronary Syndrome in a Tertiary Cardiac Centre in Bangladesh. Bangladesh Heart Journal 32 (2017): 106-113.
- Yusuf S, Reddy S, Ôunpuu S, et al. Global burden of cardiovascular diseases part I: general considerations, the epidemiologic transition, risk factors, and impact of urbanization. Circulation 104 (2001): 2746-2753.
- Islam AKMM, Majumder AAS. Coronary Artery disease in Bangladesh: A review. Indian Heart J 65 (2013): 424-435.
- Smith, Stephen W. Updates on the electrocardiogram in acute coronary syndromes. Current Emergency and Hospital Medicine Reports 1 (2013): 43-52.
- Jayroe JB, Spodick DH, Nikus K, et al. Differentiating ST ele- vation myocardial infarction and nonischemic causes of ST elevation by analyzing the presenting electrocardiogram. Am J Cardiol 103 (2009): 301-306.
- Turnipseed SD, Bair AE, Kirk JD, et al. Electrocardiogram differentiation of benign early repolarization versus acute myocardial infarction by emer- gency physicians and cardiologists. Acad Emerg Med 12 (2005): 85-86.
- Wung SF. Discriminating between right coronary artery and circumflex artery occlusion by using a noninvasive 18-lead electrocardiography. American Journal of Critical Care 16 (2007): 63-67.
- Mamun KSA, Awal A, Murshed AKMM. Correlation of ECG Changes with Coronary Angiographic Findings in Acute Inferior Myocardial Infarction. Medicine Today 29 (2017): 33-36.
- Gupta A, Lokhandwala YY, Kerkar PG, et al. Electrographic differentiation between right coronary and left circumflex coronary arterial occlusion in isolated inferior wall myocardial infarction. Indian Heart J 51 (1999): 281-284.
- Bayram E, Atalay C. Identification of the Culprit Artery Involved in Inferior Wall Acute Myocardial Infarction Using Electrocardiographic Criteria. The Journal of International Medical Research 32 (2004): 39-44.
- Almansori M, Armstrong PW, Fu Y, et al. Electrocardiographic identification of the culprit coronary artery in inferior wall ST elevation myocardial infarction. Can J Cardiol 26 (2010): 293-296.
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bulletin of the World Health Organization 79 (2001): 373-374.
- Voigt, Paul, von dem Bussche A. Enforcement and fines under the GDPR. The EU General Data Protection Regulation (GDPR). Springer, Cham (2017): 201-217.
- Zeitouni M, Clare RM, Chiswell K, et al. Risk Factor Burden and Long-Term prognosis of Patients with Premature Coronary Artery Disease. JAm Heart Assoc 9 (2020): e017712.
- Joshi P, Islam 5, Paris P, et al. Risk factors for Early Myocardial Infarction in South Asians Compared With Individuals in Other Countries. JAMA 297 (2007): 286-294.
- Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation 97 (1998): 596-601.
- Jafary MH, Samad A, Ishaq M, et al. Profile of Acute Myocardial Infarction (AMI) in Pakistan. Pak J Med Sci 23 (2007): 485-489.
- Boden WE, O’ rouke RA. COURAGE trial group. The evolving pattern of coronary artery diseases in the US and Canada. Baseline characteistics of the clinical outcomes Utilizing Revascularization and aggressive Drug Evaluation (COURAGE) trial. Am J Cadiol 99 (2007): 208-212.
- Fournier JA, Sanchez A, Quero J, et al. Myocardial infarction in men aged 40 years or less: A prospective clinical-angiographic study. Clinical cardiology 19 (1996): 631-636.
- Hafeez S, Javed A, Kayani AM. Clinical profile of patients presenting with acute ST elevation myocardial infarction. JPMA 60 (2010): 190.
- Mohsin A, Rubaiyat KA, Saleh MAD, et al. Clinical characteristics and angiographic profile of acute coronary syndrome patients in a tertiary hospital of Bangladesh. Bangladesh Heart Journal 33 (2018): 10-15.
- Akanda MAK, Ali SY, Islam AEMM, et al. Demographic Profile, Clinical Presentation & Angiographic Findings in 637 Patients with Coronary Heart Disease. Faridpur Medical College Journal 6 (2011): 82-85.
- Birnbaun Y, Wagner GS, Barbash GI, et al. Correlation of angiographic findings and right(V1 to V3) versus left(V4 to V6) precordial ST-segment depression in inferior wall acute myocardial infarction. Am J Cardiol 83 (1999): 143-148.
- Zimetbaun Pi, Krishnan S, Gold A, et al. Usefulness of ST-segment elevation in lead III exceeding that of lead II for identifying the location of the totally occluded coronary artery in inferior wall myocardial infarction. Am J Cardiol 81 (1998): 918-919.
- Engelen DJ, Gorgels AP, Cheriex EC, et al. Value of the electrocardiogram in localizing the occlusion site in the left anterior descending coronary artery in acute anterior myocardial infarction. J Am Coll Cardiol 34 (1999): 389-395.
- Ghosh B, Indurkar M, Jain MK. ECG: A simple noninvasive tool to localize culprit vessel occlusion site in acute STEMI. Indian J Clin Pract 23 (2013): 590-595.
- Gorgels AP, Engelen DJ, Wellens HJ. The electrocardiogram in acute myocardial infarction. In: Fuster V, Alexander RW, O’Rourke RA, editors. Hurst’s The Heart. 11th ed. New York: McGraw-Hill (2004): 1351-1360.
- Kosuge M, Kimura K, Ishikawa T, et al. New electrocardiographic criteria for predicting the site of coronary artery occlusion in inferior wall acute myocardial infarction. Am J Cardiol 82 (1998): 1318-1322.
- Verouden NJ, Barwari K, Koch KT, et al. Distinguishing the right coronary artery from the left circumflex coronary artery as the infarct-related artery in patients undergoing primary percutaneous coronary intervention for acute inferior myocardial infarction. Europace 11 (2009): 1517-1521.
- Kabir MS, et al. Coronary Angiographic Evaluation of Patients of Northern Districts of Bangladesh with Inferior Myocardial Infarction at a Tertiary Care Multidisciplinary Hospital. M. Abdur Rahim medical college journal 15 (2022): 101-109.
- Jenca D, Melenovsky V, Stanek VS, et al. Heart Failure after myocardial infarction: incidence and predictors. ESC heart Fail 8 (2021): 222-237.