Cognitive Orientation to daily Occupational Performance (CO-OP) Intervention for People with Cerebral Palsy: A Systematic Review with Meta-Analysis
Article Information
Hortensia Gimeno1, Michelle Jackman2, Iona Novak3*
1School of Life Course Sciences, Division of Women and Children’s Health, King’s College London, London, UK
2Paediatric Occupational Therapy Department, John Hunter Children’s Hospital, Newcastle, Australia
3Faculty of Medicine and Health, The University of Sydney, Sydney, Australia
*Corresponding Author: Iona Novak, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia
Received: 23 August 2021; Accepted: 30 August 2021; Published: 06 September 2021
Citation:
Hortensia Gimeno, Michelle Jackman, Iona Novak. Cognitive Orientation to daily Occupational Performance (CO-OP) Intervention for People with Cerebral Palsy: A Systematic Review with Meta-Analysis. Journal of Pediatrics, Perinatology and Child Health 5 (2021): 177-193.
View / Download Pdf Share at FacebookAbstract
Aim: Cognitive Orientation to daily Occupational Performance (CO-OP) was originally designed for children with Developmental Coordination Disorder but has more recently been applied to the cerebral palsy population who also have disorders of motor function and executive function. The aim of this review was to examine the feasibility, acceptability, and effectiveness of CO-OP in the cerebral palsy population.
Methods: A systematic literature review was carried out to identify studies on CO-OP for people with cerebral palsy, using the Medline, CINAHL and ERIC databases between 22 June and 30 June 2021.
Results: The search elicited 44 citations, of which 8 studies met eligibility. Five were observational studies (three of five Single Case Experimental Design), three were randomized controlled trials (RCTs), measuring the effects of CO-OP in 100 people with cerebral palsy. Since CO-OP was repurposed to cerebral palsy, initial studies focused on feasibility, acceptability and preliminary efficacy, and consequently sample sizes were small with high risk of bias. Pooled findings from RCTs indicate CO-OP produces greater gains in goal achievement than to body functions and structure intervention (Standardised Mean Difference 0.86 [95% Confidence Interval 0.20-1.52]).
Conclusions: Findings suggest preliminary efficacy of CO-OP for cerebral palsy compared to body functions and structure interventions for goal attainment, with CO-OP having comparable efficacy to other activities-based interventions. More clinical trials with adequate power and an individual patient meta-analysis are recommended.
Keywords
Cognitive Orientation to Occupational Performance; Cerebral Palsy; Systematic Review; Meta-Analysis; Motor Learning
Cognitive Orientation to Occupational Performance articles; Cerebral Palsy articles; Systematic Review articles; Meta-Analysis articles; Motor Learning articles
Article Details
Abbreviations:
ADL: Activities of Daily Living; AMPS: Assessment of Motor and Process Skills; BOTMP: Bruininks-Oseretsky Test of Motor Profici-ency; COPM: Canadian Occupational Performance Measure; CO-OP: Cognitive Orientation to Occupa-tional Performance; CP: Cerebral Palsy; CI: Confidence Interval; DCD: Developmental Coordination Disorder; DPA: Dynamic Performance Analysis; GMFCS: Gross Motor Function Classification System; Hr: Hour; ICC: Intraclass Coefficient; ICF: International Classification of Functioning, Disability and Health; Inc: Include; IQ: Intelligence Quotient; MACS: Manual Ability Classifi-cation System; Min: Minutes; PQRS: Performance Quality Rating Scale; RCT: Randomized Controlled Trial; RoB2: Cochrane Risk of Bias 2; ROBINS-I: Risk Of Bias In Non-randomized Studies – of Interventions; RoBiNT: Risk of Bias in N-of-1 Trials; SMD: Standardised Mean Differences; Wk: Week; Yrs: Years
1. Introduction
Cognitive Orientation to daily Occupational Performance (CO-OP) is an individualised intervention that employs cognitive strategies for problem-solving task-specific performance of daily activities[1]. CO-OP seeks to drive individualised motor skill acquisition and performance to enable improved participation. Its basis lies in both the motor learning and cognitive approaches. Central to CO-OP is the use of cognitive strategies to help children or adults generate their own solutions to overcome self-identified problems encountered in everyday living, rather than solutions identified by therapists or carer. The benefits, therefore, extend beyond the duration of the intervention, because the strategies can be applied to other tasks thereby increasing independence, transfer and self-management. The CO-OP approach was first developed over two decades ago to treat children with Developmental Coordination Disorder (DCD) [1]. Children with DCD experience motor and coordination difficulties when performing motor tasks, arising from problems with motor planning executive function [2]. Since the initial development for DCD, the approach has now been empirically tested with a number of populations, some of which have performance problems associated with issues of motor planning—as do children and young people with DCD—and others who have performance problems associated with both motor planning and motor control from neurological damage in conditions such as adults with stroke [3-6] and acquired brain injury [7] suggesting that CO-OP has much wider potential applicability. The cumulative evidence suggests that CO-OP results in improvements in function and everyday activity performance in a variety of populations, including cerebral palsy (CP) [8].
Cerebral palsy is an umbrella term describing movement disorders that result from damage to the developing brain [9]. The incidence of cerebral palsy ranges from 1.4 to 3.4 per 1000 live births in high and low income setting respectively [10-13]. The severity of cerebral palsy varies from mild to severe and impacts on a person’s ability to participate in important life activities. In addition to difficulties with movement, people with cerebral palsy often experience challenges with communication, cognition, behaviour, feeding, vision, pain, and sleep [14]. Therapeutic management of cerebral palsy has progressed significantly over the past 20 years. In line with the world health organisation’s International Classification of Functioning, Disability and Health (ICF) framework for children and youth [15], best practice therapeutic management of cerebral palsy is no longer focussed on addressing underlying impairments, but rather focusses on what is important to the individual, taking into consideration not only the abilities of the individual as well as the social and environmental context. Current evidence focusses on the importance of setting individual goals, with a focus on practice of the goals within real life contexts, rather than addressing underlying impairments. The CO-OP approach aligns with this current thinking about a focus on client-set goals, direct practice of goals and consideration of how practice will be needed to achieve carryover into everyday life, outside of the therapy environment. Much of the current research in cerebral palsy includes participants who present primarily with spasticity, with very little research to guide intervention for those who present with dystonia [16]. Dystonia is characterised by repetitive, abnormal movements and postures, that are often associated with, or exacerbated by voluntary actions [17]. Initial studies suggest the CO-OP approach may be feasible in facilitating goal achievement for children and young people with cerebral palsy, including those with dystonia.
The CO-OP approach consists of 10-12 one hour sessions dedicated to establishing client-set goals and teaching the client a global problem-solving strategy [1]. There are seven key features to CO-OP. The entire process is task performance based (i.e., the client is engaged in performing the skills inherent within the goals they identified). In an episode of care, generally three goals are identified and trained (key feature 1 – client centred goal setting). Some studies have measured up to 5 goals before and after CO-OP so that transfer and generalisation could be measured across non-trained goals. Two key features of CO-OP are designed to support transfer. First, Dynamic Performance Analysis (DPA) (key feature 2), is used collaboratively to ascertain where the performance of the task/activity is breaking down. Second, Guided Discovery (key feature 3), is a non-directive therapeutic process whereby the therapist prompts the client to develop and employ the analysis and problem-solving skills to identify possible strategies to achieve their goal. Cognitive strategy use (key feature 4) includes the use of the meta-cognitive strategy Goal-Plan-Do-Check which is taught in the first session of the intervention and used throughout the intervention. It is through the DPA, that clients are guided to self-identify potential solutions (known as plans). To support the child or adult’s discovery of possible plans, domain specific strategies are also applied (e.g. motor mnemonics) supporting skill acquisition, memory of strategies, generalisation and transfer. In combination with DPA and guided discovery, there are four other enabling principles (key feature 5) that therapists use throughout the intervention sessions, including: (i) making it fun; (ii) promoting learning; (iii) working towards independence; and (iv) promoting generalisation and transfer. The last two features are about the format CO-OP therapy, and the use of significant others such as carers to support strategy use, generalisation and transfer (key features 6 and 7). The aim of this review was to examine the feasibility, acceptability, and effectiveness of CO-OP in the cerebral palsy population.
2. Materials and Methods
2.1 Objectives
- To assess the feasibility and acceptability of CO-OP for people with cerebral palsy; and
- To assess the effectiveness of CO-OP for improving goal achievement of functional tasks in people with cerebral palsy.
To assess feasibility and acceptability of CO-OP in people with cerebral palsy we included observational studies (n-of-1 trials and single case experimental de-sign (SCED)) and randomized controlled trials (RCTs). To assess effectiveness, we included randomized contr-olled trials (RCTs) that compared the outcomes of CO-OP intervention to usual care or any other non-CO-OP intervention (controls), in people with cerebral palsy.
We included studies of humans with cerebral palsy. We included studies that had any participants with cerebral palsy. We did not apply any age or severity of motor impairment restrictions.
We included comparisons of outcomes after CO-OP intervention versus usual care (controls).
Goal achievement of functional tasks was the primary outcome because this is the chief claim of CO-OP intervention.
2.6 Instruments
The Canadian Occupational Performance Measure (COPM) is a client-centred measure of individual goal achievement over time, in which clients identify goals that are important to them, then rate their performance and satisfaction on a visual analogue scale of one to ten [18]. The COPM has adequate validity and reliability [19] and has been shown to have good responsivity to change in children with cerebral palsy [19, 20]. The Canadian Occupational Performance Measure (COPM) is the most widely used and accepted instrument for measuring changes in goal performance from intervene-tion for children with cerebral palsy, trailed by the Goal Attainment Scale (GAS), which has even better responsivity to change [20]. The Performance Quality Rating Scale (PQRS) is a COPM complementary tool which instead uses a therapist-rated visual analogue scale of performance of the exact same task that the client rates. The PQRS has shown substantial reliability and internal responsiveness in two different populations, adults with stroke and children with DCD [21]. An individualised criterion-based approach to rating perfor-mance (PQRS-i) has been suggested more appropriate to use for individuals with more severe motor impair-ments such as people with cerebral palsy (CP) [22]. Inter-rater reliability has been established specifically in some studies including people with cerebral palsy with Intraclass Coefficient (ICC) =0.830 [23] and ICC= 0.947 [22].
2.7 Search methods for identification of studies
2.7.1 Electronic searches: We used an a priori developed search strategy based upon the recommendations of the Cochrane Collaboration [24]. Our comprehensive search sought to identify randomized controlled trials and observational studies, with no restriction on language or study years. Search terms were Population = cerebral palsy OR dystonia OR hemiplegia; Intervention = CO-OP; Comparison = none specificized, all accepted; Outcome = none specificized, all accepted. The following electronic databases were searched: Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; CINAHL.
2.8 Data collection and analysis
2.8.1 Selection of studies: Two authors independently reviewed the titles and abstracts of studies identified in the search and to exclude ineligible studies. If the title or the abstract did not provide sufficient information to determine eligibility, two independent reviewers appraised the full texts. An independent third reviewer resolved disagreements.
2.8.2 Data extraction and management: Two review authors independently extracted the data from the included studies using the Cochrane methodology [24], extracting: citations; methodology; participants; interventions; comparators; goal, dose, and outcomes. Papers with duplicate data were excluded. There was agreement on all extracted data.
2.8.3 Risk of bias: Two authors independently assessed risk of bias. Authors of included papers did not rate their own publications. Randomized controlled trials were evaluated using the Cochrane Risk of Bias 2 [25] and observations studies using the Risk Of Bias In Non-randomized Studies – of Interventions (ROBINS-I) [26] with the single case experimental designs evaluated on the Risk of Bias in N-of-1 Trials (RoBiNT) [27]. There were no disagreements.
2.9 Data synthesis and measures of treatment effect
Results were presented in a summary of findings table (Table 1). A priori we planned to aggregate comparable findings in a meta-analysis, using Review manager software (RevMan5.4), to provide a summary estimate of the effect of CO-OP. For continuous outcomes with different units, effects were expressed as standardised mean differences (SMD) with 95% confidence intervals. We assessed heterogeneity using Chi2 with a significance level at p<0.05. We considered I2>25% moderate heterogeneity, I2>75% high heterogeneity.
- Results
3.1 Results of the search
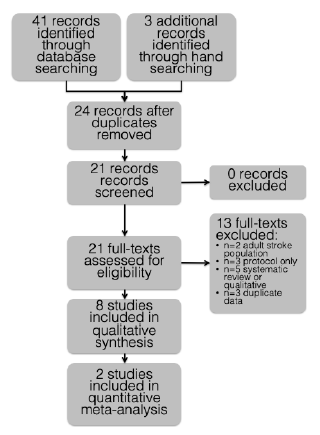
Results are reported in a PRISMA flow diagram (Figure 1) [28]. The search was carried out in June 2021. The electronic search plus hand searching elicited 44 citations. After screening, 21 studies were potentially eligible. After inspecting full texts, eight studies met eligibility [22, 29-35]. Reasons for exclusion are summarized in the flow diagram. Studies meeting inclusion criteria were all published in English. No data were missing and therefore contact with authors was required.
3.2 Included studies
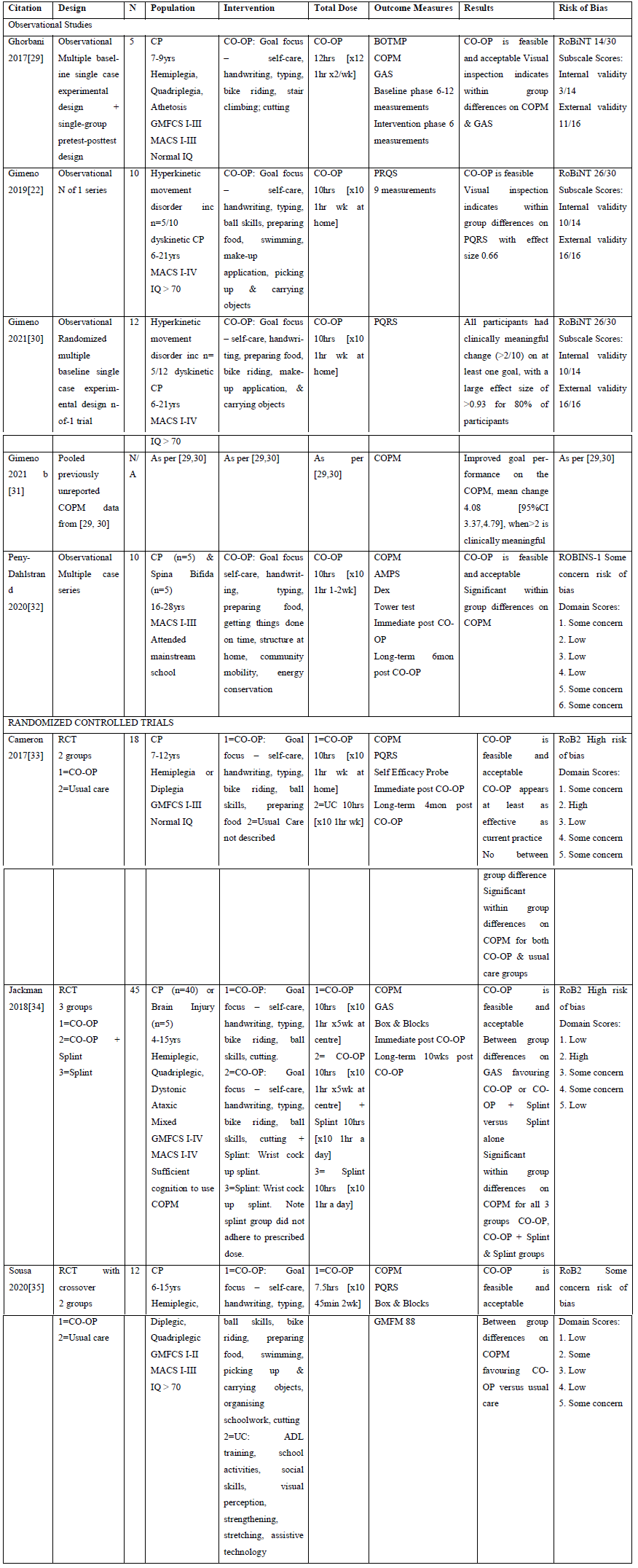
3.2.1 Types of study designs: We included five observational studies (3/5 Single Case Experimental Design) [22, 29-32] plus three RCTs [33-35] evaluating feasibility, acceptability and preliminary efficacy of CO-OP intervention for improving goal achievement in people with cerebral palsy. Results are summarized in Table 1.
3.2.2 Types of participants: The eight included trials studied 112 participants, which included 100 participants with cerebral palsy. The studies included all sub-types of cerebral palsy, which was spastic, dyskinetic and mixed. All eight studies included participants with Manual Ability Classification System (MACS) levels I-III and Gross Motor Function Classification System (GMFCS) levels I-III, and three of eight studies also included MACS level IV and GMFCS level IV. The age of participants ranged from 4-28 years old.
3.3 Feasibility and acceptability
Feasibility and acceptability parameters were specifically gathered in three observational studies [30-32], including the feasibility of outcome measure, adherence to intervention, and acceptability to therapists. At trial completion, all three RCTs also concluded that CO-OP was feasible and acceptable to repurpose to people with cerebral palsy [33-35]. There was little to no loss to follow-up in the n-of-1 Single Case Experimental Design Studies and the RCTs, suggesting acceptability. Fidelity to the CO-OP approach was measured and found to be variable in a study which included five different treating therapists [31] indicating future studies may require close supervision and training.
3.4 Effect on goal achievement
A total of 10 individuals with dyskinetic cerebral palsy were included in two multiple baseline n-of-1 trials [22, 30]. Whilst five children were classified as MACS II, there were also four children with MACS level IV (i.e. more severe physical disability). Ratings from the PQRS-I indicated improvement in all three goals only in three out of nine individuals at post-intervention and three out of five individuals at three months following the intervention. Most participants improved on at least two goals. Possible explanations include the difficulty of the selected goals in relation to the participants motor impairments, baseline motor fluctuations, fidelity of treatment, or the expertise of the therapist delivering the intervention. Other factors include dosage, which has not been explored in studies of CO-OP in cerebral palsy. The published pooled data for the two single case experimental designs [29-30] in dyskinetic patients showed strong effect size for goals selected (COPM and PQRS-i), self-efficacy, and quality of life despite no changes in dystonia or other body impairments [31]. The five children aged 7 to 9 years in one of the single case experimental designs achieved clinically signify-cant changes on the COPM, as rated separately by parents and children [29]. As did the five young people with cerebral palsy in a multiple case series who achie-ved clinically significant improvements in all three of the goals they each set [32]. These young people report-ed that they found the global problem-solving strategies helpful, and 80% of participants reported that they went on to apply these problem-solving strategies in new situations, after intervention was complete. Although acceptable, participants with cerebral palsy reported that the intervention required a lot of effort. Across the studies there was a range of goals related to self-care, leisure and productivity. In the studies that included young people up to 28 years of age, goals were more complex, relating to participation in life activities such as preparing meals, catching public transport and mana-ging daily routines [22, 30, 32]. Young people were able to achieve these more complex goals with CO-OP Approach. All three RCTs measured the effect of CO-OP on goal achievement using the COPM or GAS instruments, and found goals were achieved [33-35].
3.5 Risk of bias in included studies
The risk of bias across the studies was variable. In the five observational studies there were some concern about risk of bias [22, 29-32], with two of the single case experimental designs having excellent external validity scores [22, 30]. In the three RCTs, one had some concern [35] and two had high risk of bias [33, 34].
3.6 Quantitative results from randomized controlled trials
One of the three RCTs compared CO-OP with alike activities-based interventions [33] whereas two of three RCTs compared CO-OP to a body function and structures (i.e. impairment-based and thus distinctly different) intervention [34-35]. The one trial that compared CO-OP to alike activities-based interventions concluded that CO-OP was equally effective to usual care activities-based intervention. Plus the authors deemed this trial to have been contaminated as one participant in the usual care group to have also received CO-OP. The two RCTs that compared CO-OP to a body function and structures intervention were deemed to have suitable homogeneity to aggregate within a meta-analysis (Figure 2). One single common data point existed between the trials (the immediate post intervention data point after 10 sessions) and was therefore used in the meta-analysis. One of the two RCTs included within the meta-analysis was a three group RCT comparing: (1) CO-OP; versus (2) CO-OP plus splinting; versus (3) splinting alone [34]. For this multiple arm study, the control group data were split in the meta-analysis across the two CO-OP arms, to avoid duplicate counting of control cases, as per Cochrane Handbook recommendations [24]. The other trial included within the meta-analysis was a crossover trial [35]. Only the data collected before the crossover was used within the meta-analysis, to circumvent within person affects. The two trials that compared CO-OP to a body function and structures intervention reported statistically significant between group differences on COPM or GAS favoring CO-OP intervention. Overall, CO-OP had a greater effect on goal achievement (as measured on the COPM or GAS), than a body functions and structures intervention SMD=0.86 [95% CI 0.20-1.52] (Figure 2). With low heterogeneity between studies (I2=16%).
Table 1: Summary of Findings.
4. Discussion
We set out to examine the feasibility, acceptability and effectiveness of CO-OP repurposed to the cerebral palsy population and found that all studies concluded CO-OP was feasible and acceptable to people with cerebral palsy. We also found in a meta-analysis that CO-OP had a greater effect on goal achievement than a body functions and structures intervention. CO-OP was found to be both feasible and acceptable in low, middle [35] and high-income settings [33-34], for children and young people with cerebral palsy who ranged in age from 4 years to 28 years of age. CO-OP has now been used effectively with children presenting with unilateral, bilateral or diplegic cerebral palsy, including those with spasticity, dystonia and ataxia [22, 29-35]. Most participants in included studies had hand function at MACS level I to III and gross motor ability at GMFCS I to III, in other words mild-moderate disability with enough selective motor control to respond to a motor-training intervention. Qualitative studies investigating the experience of CO-OP report that young adults with cerebral palsy and spina bifida found CO-OP also improved self-efficacy and enabled these participants to master everyday life activities using problem solving strategies [36]. Mothers of children with cerebral palsy who participated in CO-OP perceived the CO-OP approach to be an effective intervention to enable their children to achieve goals, empowered their children to take some control, providing them with problem-solving strategies to that they could apply to future goals [37].
Of importance the two Single Case Experimental Design studies conducted with people with dystonic cerebral palsy, also indicated CO-OP to be feasible in this population [22, 30]. Moreover, 63% achieved their trained goals, with moderate to large effect sizes (0.66-1.00) [30]. There is a distinct lack of proven effective treatments for people with dystonia, as often clinical trials in the cerebral palsy population are conducted in the spastic motor sub-type and or include only small numbers of people with the dystonic motor sub-type and thus implications for dystonia are often ambiguous [16]. CO-OP appears to be a useful way forward in the cerebral palsy dystonic motor sub-type, which offers a new treatment option for people with this complex and disabling motor disorder [22, 30]. Skill improvement was observed in all individuals with dyskinetic cerebral palsy independently of their baseline characteristics included those receiving intervention by occupational therapists with no prior experience of delivering CO-OP or treatment to this population. It appears that CO-OP’s individualised self-generated movement plans support the needs of people with dystonia, who often have normal intelligence and problem solving, but highly variable involuntary postures that they need to suppress during voluntary movement. For the CO-OP Approach to be a feasible intervention, the individual should meet the key pre-requisites of (i) identifying three meaningful goals they are motivated to improve on; (ii) sufficient language and behavioural responsiveness to discuss their performance with the therapist; (iii) the cognitive ability to problem solve, and (iv) the potential to achieve the goal [1].
Given the small number of trials in cerebral palsy, it remains unclear if there are specific characteristics that are likely to predict which individuals would most benefit from use of the CO-OP Approach. In regard to cognitive ability, research has shown that children with cerebral palsy who have a moderate cognitive impairment can benefit from CO-OP [35], so it is important not to disregard CO-OP as a possible intervention for these individuals. In a small post-hoc analyses investigating best responders in cerebral palsy, analyses suggested that children with cerebral palsy who had co-morbidities, including autism spectrum disorder, behavioural difficulties, visual impairment or language impairment were less likely to achieve their goals following participation in CO-OP [38]. Consideration of family support and access to necessary resources (such as a bike at home if the goal is bike riding) are important for success in CO-OP [35]. The CO-OP approach, with its focus on client-centred goals and practice of whole tasks within real life contexts, is in line with current best practice principles for children and young people with cerebral palsy [16]. There are a number of effective goal-focussed interventions for children with cerebral palsy, including constraint-induced movement therapy, bimanual training and goal-directed training [16]. One benefit of CO-OP is that may require a much lower dose of therapy and practice [39] compared to alike alterative interventions. This may make CO-OP more feasible in regard to time constraints and may be an important consideration when discussing potential intervention options with children and families, plus more cost effective.
Almost all the studies made special mention that the CO-OP approach led to transference of the application of the global problem-solving strategy to tasks outside the CO-OP therapy episode. This led to the person acquiring even more skills than those targeted in the therapy sessions. In one of the dystonia single case experimental design studies there was 37% transfer [30]. The phenomenon of transference from CO-OP has also been observed previously in the Developmental Coordination Disorder population. Transference is an important principle of neuroplasticity and potentially provides cost savings to the healthcare system, if the recipient of CO-OP is better able to self-manage their condition. Cerebral palsy is a heterogeneous group of individuals and current trials and studies of CO-OP with this population remain small and mostly unpowered. However, proof-of-concept, feasibility and acceptability has been established for this intervention with unilateral and bilateral cerebral palsy, including those with associated dyskinesia. This is particularly important given the paucity of evidence for dyskinetic cerebral palsy. Whilst most individuals have less severe forms of cerebral palsy (MACS/GMFCS I-III), the intervention is also feasible with individuals with more severe forms (MACS/GMFCS level IV). Given the low intensity of this approach is feasible within the context of clinical practice.
4.1 Limitations
There were several limitations to this study. There were only a small number of studies, with a small number of participants that met our inclusion criteria, with the quality of evidence and risk of bias varying widely amongst these studies. Cerebral palsy is a heterogeneous condition, therefore the benefits of any approach that may benefit each unique individual with cerebral palsy is difficult to investigate with rigorous research methods. Objectively measuring change in individual goal achievement and meaningful activities continues to be a challenge. The COPM is responsive to change but is subjective as it is measured by the individual, which is partially overcome by therapist ratings on the PQRS.
4.2 Recommendations for future research
More RCTs with adequate statistical power and low risk of bias are warranted given the promising indication of CO-OP effectiveness from these early feasibility pilots and observational studies. Further powered studies are required to ascertain who the intervention works for best, how and when treatment starts to have an effect. There are very important lessons from the included studies suggesting that: (1) larger trials should have adequate sample size to account for the individual patient differences in this heterogenous population; (2) that inclusion criteria should be designed around the best responder data [38], (3) that there should be consideration of head-to-head comparisons with other alike interventions that have require a higher threshold intensity [38] to examine cost benefits plus duration of carryover effects and transference; and (4) endpoints should examine the effects of CO-OP on participation in addition to activities, given the complexity and community-based character of the daily life tasks people are setting as goals. An individual patient meta-analysis is also warranted to further examine characteristics of responders to design future RCTs with precision.
Acknowledgements
Nothing to declare.
Conflicts of Interest
All of the authors are certified CO-OP instructors with the International Cognitive Approaches Network (ICAN).
References
- Mandich A, Polatajko HJ. Enabling occupation in children: The cognitive orientation to daily occupational performance (CO-OP) approach (2004).
- Blank R, Smits-Engelsman B, Polatajko H, et al. European Academy for Childhood Disability (EACD): Recommendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Developmental Medicine and Child Neurology 54 (2012): 54-93.
- Henshaw E, Polatajko H, McEwen S, et al. Cognitive approach to improving participation after stroke: Two case studies. American Journal of Occupational Therapy 65 (2011): 55-63.
- McEwen S, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific training improve transfer to untrained activities in subacute stroke: an exploratory randomized controlled trial. Neurorehabilitation and Neural Repair 29 (2015): 526-536.
- McEwen SE, Polatajko HJ, Huijbregts MPJ, et al. Inter-task transfer of meaningful, functional skills following a cognitive-based treatment: Results of three multiple baseline design experiments in adults with chronic stroke. Neuropsychological Rehabilitation 20 (2010): 541-561.
- Linkewich E, Avery L, Rios J, et al. Minimal Clinically Important Differences in Functional Independence After a Knowledge Translation Intervention in Stroke Rehabilitation. Archives of Physical Medicine and Rehabilitation 101 (2020): 587-591.
- Dawson DR, Binns MA, Hunt A, et al. Occupation-based strategy training for adults with traumatic brain injury: a pilot study. Archives of Physical Medicine and Rehabilitation 94 (2013): 1959-1963.
- Scammell EM, Bates SV, Houldin A, et al. The Cognitive Orientation to daily Occupational Performance (CO-OP): A scoping review: L’approche CO-OP (Cognitive Orientation to daily Occupational Performance): Examen de la portee. Canadian Journal of Occupational Therapy 83 (2016): 216-225.
- Bax M, Goldstein M, Rosenbaum P, et al. Proposed definition and classification of cerebral palsy, April 2005. Developmental Medicine and Child Neurology 47 (2005): 571-576.
- Galea C, McIntyre S, Smithers-Sheedy H, et al. Cerebral palsy trends in Australia (1995-2009): a population-based observational study. Developmental Medicine and Child Neurology 61 (2019): 186-193.
- Hollung SJ, Vik T, Lydersen S, et al. Decreasing prevalence and severity of cerebral palsy in Norway among children born 1999 to 2010 concomitant with improvements in perinatal health. European Journal of Paediatric Neurology 22 (2018): 814-821.
- Chauhan A, Singh M, Jaiswal N, et al. Prevalence of Cerebral Palsy in Indian Children: A Systematic Review and Meta-Analysis. Indian Journal of Pediatrics 86 (2019): 1124-1130.
- Khandaker G, Muhit M, Karim T, et al. Epidemiology of cerebral palsy in Bangladesh: a population-based surveillance study. Developmental Medicine and Child Neurology 61 (2019): 601-609.
- Novak I, Hines M, Goldsmith S, et al. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics 130 (2012): e1285-e1312.
- World Health Organization. International Classification of Functioning, Disability, and Health: Children & Youth Version: ICF-CY. World Health Organization (2007).
- Novak I, Morgan C, Fahey M, et al. State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Current Neurology and Neuroscience reports 20 (2020): 1-21.
- Albanese A, Bhatia K, Bressman SB, et al. Phenomenology and classification of dystonia: a consensus update. Movement Disorders 28 (2013): 863-873.
- Law M, Baptiste S, Carswell A, et al. COPM Canadian occupational performance measure. 4th edition Ottowa, ON, CAOT Publications ACE (2005).
- Sakzewski L, Boyd RN, Ziviani J. Clinimetric properties of participation measures for 5- to 13-year-old children with cerebral palsy: a systematic review. Developmental Medicine and Child Neurology 49 (2007): 232–240.
- Cusick A, McIntyre S, Novak I, et al. A comparison of goal attainment scaling and the Canadian Occupational Performance Measure for paediatric rehabilitation research. Pediatric Rehabilitation 9 (2006): 149-157.
- Martini R, Rios J, Polatajko H, et al. The performance quality rating scale (PQRS): reliability, convergent validity, and internal responsiveness for two scoring systems. Disability and Rehabilitation 37 (2015): 231-238.
- Gimeno H, Brown RG, Lin JP, et al. Cognitive approach to rehabilitation in children with hyperkinetic movement disorders post-DBS. Neurology 92 (2019): e1212-e1224.
- Gimeno H, Farber J, Thornton J, et al. The relative merits of an individualised versus a generic approach to rating functional performance in childhood dystonia. Children. Submitted.
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration (2011).
- Sterne JAC, Savovi? J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ (2019): 366.
- Jüni P, Loke Y, Pigott T, et al. Risk of bias in non-randomized studies of interventions (ROBINS-I): detailed guidance. British Medical Journal (2016).
- Tate RL, Perdices M, Rosenkoetter U, et al. Revision of a method quality rating scale for single-case experimental designs and n-of-1 trials: The 15-item Risk of Bias in N-of-1 Trials (RoBiNT) Scale. Neuropsychological Rehabilitation 23 (2013): 619-638.
- Moher D, Liberati A, Tetzlaff J et al. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology 62 (2009): 1006-1012.
- Ghorbani N, Rassafiani M, Izadi-Najafabadi S, et al. Effectiveness of cognitive orientation to (daily) occupational performance (CO-OP) on children with cerebral palsy: A mixed design. Research in developmental disabilities 71 (2017): 24-34.
- Gimeno H, Polatajko HJ, Lin JP, et al. Cognitive Strategy Training in Childhood-Onset Movement Disorders: Replication Across Therapists. Frontiers in Pediatrics 8 (2021): 1-8.
- Gimeno H, Polatajko HJ, Cornelius V, et al. Rehabilitation in childhood-onset hyperkinetic movement disorders including dystonia: Treatment change in outcomes across the ICF and feasibility of outcomes for full trial evaluation. European Journal of Paediatric Neurology (2021).
- Peny-Dahlstrand M, Bergqvist L, Hofgren C, et al. Potential benefits of the cognitive orientation to daily occupational performance approach in young adults with spina bifida or cerebral palsy: a feasibility study. Disability and rehabilitation 42 (2020): 228-239.
- Cameron D, Craig T, Edwards B, et al. Cognitive orientation to daily occupational performance (CO-OP): a new approach for children with cerebral palsy. Physical & Occupational Therapy in Pediatrics 37 (2017): 183-198.
- Jackman M, Novak I, Lannin N, et al. Effectiveness of cognitive orientation to daily occupational performance over and above functional hand splints for children with cerebral palsy or brain injury: a randomized controlled trial. BMC pediatrics 18 (2018): 1-12.
- Sousa LK, Brandão MB, Curtin CM, et al. A Collaborative and Cognitive-based Intervention for Young People with Cerebral Palsy. Canadian Journal of Occupational Therapy 87 (2020): 319-330.
- Öhrvall AM, Bergqvist L, Hofgren C, et al. "With CO-OP I'm the boss" - experiences of the cognitive orientation to daily occupational performance approach as reported by young adults with cerebral palsy or spina bifida. Disability and Rehabilitation 42 (2020): 3645-3652.
- Jackman M, Novak I, Lannin N, et al. Parents' experience of undertaking an intensive cognitive orientation to daily occupational performance (CO-OP) group for children with cerebral palsy. Disability and Rehabilitation 39 (2017): 1018-1024.
- Jackman M, Novak I, Lannin NA, et al. The Cognitive Orientation to daily Occupational Performance (CO-OP) Approach: Best responders in children with cerebral palsy and brain injury. Research in Developmental Disabilities 78 (2018): 103-113.
- Jackman M, Lannin N, Galea C, et al. What is the threshold dose of upper limb training for children with cerebral palsy to improve function? A systematic review. Australian Occupational Therapy Journal 67 (2020): 269-280.