Cardiology Teleconsultation in the Region with the Largest Number of Isolated Cities in Brazil: Initial Data from the Government Program and Insights for Improvement
Article Information
Tarso A. D. Accorsi*, Antonio F. B.de Azevedo Filho, Bruna R. S. Matuck, Mariana P. Lopes, Italo M. Ferreira, Mauricio R. Mocha, Joao R. C. Fernandes, Matheus de O. L. Ribeiro, Marcelo Kirschbaum, Fernando F. Ribas, Renata A. Morbeck, Karine De Amicis Lima, Carlos H. S. Pedrotti, Eduardo Cordioli
Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil
*Corresponding Author: Tarso A. D. Accorsi, MD, PhD, Telemedicine Department, Hospital Israelita Albert Einstein, Sao Paulo, Brazil, 08084
Received: 29 May 2020; Accepted: 09 June 2020; Published: 21 July 2020
Citation: Tarso A. D. Accorsi, Antonio F. B.de Azevedo Filho, Bruna R. S. Matuck, Mariana P. Lopes, Italo M. Ferreira, Mauricio R. Mocha, Joao R. C. Fernandes, Matheus de O. L. Ribeiro, Marcelo Kirschbaum, Fernando F. Ribas, Renata A. Morbeck, Karine De Amicis Lima, Carlos H. S. Pedrotti, Eduardo Cordioli. Cardiology Teleconsultation in the Region with the Largest Number of Isolated cities in Brazil: Initial Data from the Government Program and Insights for Improvement. Cardiology and Cardiovascular Medicine 4 (2020): 361-375.
View / Download Pdf Share at FacebookAbstract
In remote areas with geography barriers, lack of healthcare and financing, many cardiac patients lack access to face-to-face cardiac care. Telemedicine is an efficient way to reduce the long wait for consultations with several applications, probable reason why it is being developed in many countries including Brazil. In February 2020, the Brazilian government launched an official program for teleconsultation in cardiology, with a telemedicine team from Hospital Israelita Albert Einstein, in the region with the largest number of isolated and low-income cities in Brazil (North region). Teams were provided no training (in loco and telemedicine) for consultations carried out according to the conduct of each professional. Teleconsultation in cardiology mainly aims to allowing better access to specialists, implying accurate diagnosis, better treatment, reduced mortality and significant reduction in costs, but speed of implementation is relatively slow with no standardization of care. The objective of this study was to survey attendance data, create a basis for standardization of attendance and conduct, educational actions, assist in the effectiveness of teleconsultation, rational use of resources, allow sustainable expansion of the program and assist to implement other projects. It is a retrospective and descriptive study with a single telemedicine center (Hospital Israelita Albert Einstein) reference for 120 outpatient clinics in the northern region of Brazil. Data obtained anonymously from care routine of all patients treated by the program from 02/17/2020 to 03/31/2020 was analyzed, including the referral reason, demographic profile, clinical characteristics, physical examination, medications, previous examinations and after teleconsultation.
Keywords
Telemedicine; Cardiology; Referral and Consultation; Ambulatory Care; Delivery of Health Care
Telemedicine articles, Cardiology articles, Referral and Consultation articles, Ambulatory Care articles, Delivery of Health Care articles
Article Details
Introduction
Since the 1990s, the World Health Organization (WHO) has recognized telemedicine as a remote resource for medical support through interactive methodologies of audiovisual and data communication, aimed at health care, education, and research. The development of technologies such as the internet, audio, image and video systems has undoubtedly made telemedicine expand exponentially in the last five years [1].
Physicians, hospitals and medical schools have been exploring the uses of telemedicine since 1964, primarily in the area of medical education. The emergence of telemedicine has altered the structure of the media industry, management of health providers and is likely to have an impact on changing the standard of medical care [2]. Contemporary telemedicine and telemonitoring solutions have shifted their focus, trying to work on a system that is ubiquitous, efficient and sustainable [3].
The strongest evidence for the efficacy of telemedicine for diagnostic and management decisions came from psychiatry and dermatology specialties. There was also reasonable evidence that general medical history and physical examinations performed via telemedicine had relatively good sensitivity and specificity. Other specialties in which some evidence for efficacy existed were cardiology and certain areas of ophthalmology [4].
Currently, cardiovascular diseases are the main causes of morbidity and mortality worldwide, as well as the demand for outpatient, urgent and emergency medical services. Brazil is a country of continental extension; its north region has peculiar characteristics. Despite being the larger region in size, it has the lowest population density compared to all other regions of the country and is characterized by the Amazon forest—a dense forest with the most concentration of remote areas with difficult access and locomotion between its cities and lowest Human Development Index in the country. This configures a challenge to offer the population essential health services, as seen in the availability of medical specialists in this region. This is the role of telemedicine in this population [5-10] (Table 1, Figure 1).
Table 1: Classification of isolation of Brazilian municipalities according to region and population
Source: IBGE (Brazilian Institute of Geography and Statistics). Classification and Characterization of Rural and Urban Spaces in Brazil [15].
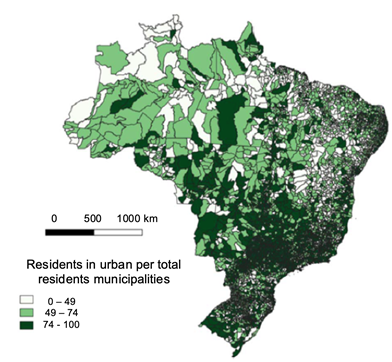
Figure 1: Proportion of urban population municipalities to region and population
Source: IBGE (Brazilian Institute of Geography and Statistics) – 2010 Census [17].
In remote areas with barriers created by geography, lack of health care system and funding, many cardiac patients do not have access to face-to-face cardiologic care. Telemedicine is an efficient way to reduce the long wait for in-person consultations and has a range of applications, probably the reason why it is being developed in several countries, including Brazil [11]. Beyond this, there is evidence that telemedicine can help compensate cardiologic chronic conditions with improvement in overall mortality and hospitalization, mainly in heart failure patients [12]. Finally, a review of the Cochrane Library and Centre for Review and Dissemination confirmed that telemedicine is cost-effective for being applied in major medical fields, especially cardiology [13].
Cardiology teleconsultation mainly aims to enable better access to heart specialists, implying accurate diagnosis, better treatment, reduction of mortality, and significant reduction in costs, but speed of implementation is relatively slow with no standardization of care [14]. Several factors, including improved technology and policies aimed to reduce hospitalization, boosted interest in the use of telemedicine in cardiology. Emerging evidence also indicates that primary care electronic consultations with cardiologists can reduce emergency room visits. A study on 36 primary care physicians and 590 patients found that asynchronous electronic consultations with a cardiologist could resolve about two-thirds of cardiac concerns without a specialist visit and reduced cardiac-related emergency visits during the 6-month follow-up period [15]. Some studies show telemedicine improves adherence of medication in an important way to improve disease outcomes and reduce burden of cardiovascular diseases in our population [15-16].
In February 2020, an official Brazilian government program for cardiology teleconsultation was launched in the north region, characterized by the largest number of isolated and low-income cities in Brazil, with few specialists working there. Once the reasons for referral, population characteristics and treatment standards are not known, this study aimed to analyze multiple demographic and clinical characteristics, as well as the medical management of all cases referred in the first 45 days of the program to redesign and adapt the current project and self-expand and guide other programs.
Materials & Methods
This was a retrospective and descriptive study, with a single telemedicine center (Hospital Israelita Albert Einstein, Sao Paulo - Brazil) reference for 120 outpatient clinics in the northern region of Brazil.
All telemedicine cardiologists were not previously trained, performing care according to their judgment. All patients referred by general practitioners, previously scheduled, attended consultations lasting 30 minutes in an eight-hours a day service.
Teleconsultation was performed after confirmation of perfect audio and image functioning in the presence of the patient and a general practitioner. Both patients and in-loco physicians did not receive any special instruction before the cardiology teleconsultation. The parameters analyzed were: the reason for referral, demographic data, clinical history, and physical exam, previous diagnostic tests, medications in use, diagnoses made, prescription of medications and exams.
All continuous variables were described as mean and standard deviation and categorical variables as absolute numbers and percentages.
Results
Total 249 patients scheduled from 02/17/2020 to 03/31/2020 were sequentially evaluated. In this initial phase, fair adherence of patients to scheduled medical appointments with an attendance of 78.5% was observed. The most common reason for referral was coronary artery disease or chest pain corresponding to 30.7% of the calls, followed by heart failure or dyspnea (20.5%), arrhythmia, palpitation or syncope (19.3%) and presence of risk factors for cardiovascular disease (17.5%). Few patients were referred for altered heart diagnostic test results (7.8%) or perioperative evaluation (4.2%). The population was predominantly female (61.3%) with average age of 57.7 + 16.8 years. There was little information on schooling, occupation, marital status, and religion (Table 2).
|
Variable |
Description |
|
Attendance, n (%) |
|
|
No |
49 (21,5) |
|
Yes |
179 (78,5) |
|
Reason for referral, n (%) |
|
|
CAD / chest pain |
51 (30,7) |
|
HF / dyspnea |
34 (20,5) |
|
Arrhythmia / palpitation / syncope |
32 (19,3) |
|
DCV RF |
29 (17,5) |
|
Altered heart diagnostic test |
13 (7,8) |
|
Preoperative evaluation |
7 (4,2) |
|
Age (years) |
|
|
mean ± SD |
57,7 ± 16,8 |
|
Gender, n (%) |
|
|
Female |
106 (61,3) |
|
Male |
67 (38,7) |
|
Marital status, n (%) |
|
|
Single |
17 (27,4) |
|
Married |
38 (61,3) |
|
Stabel union |
3 (4,8) |
|
Widower |
4 (6,5) |
|
Scholarity, n (%) |
|
|
Absent |
3 (25) |
|
Literate |
2 (16,7) |
|
Basic education |
1 (8,3) |
|
High school |
3 (25) |
|
University |
3 (25) |
|
Occupation, n (%) |
|
|
Housewife |
18 (35,3) |
|
Disabled |
1 (2) |
|
Retired |
9 (17,6) |
|
Informal |
16 (31,4) |
|
Formal |
7 (13,7) |
|
Religion, n (%) |
|
|
None |
1 (5,6) |
|
Catholic |
9 (50) |
|
Evangelical |
6 (33,3) |
|
Others |
2 (11,1) |
Table 2: Attendance, referral, and demographic data
CAD, coronary artery disease; CVD, cardiovascular disease; HF, heart failure; RF, risk factor
Among patients who reported chest pain, 83.2% pain could be defined as atypical (type C: probably not angina; or type D: definitely not angina). The majority of patients did not report pain on usual efforts, without categorization of this information. Besides, dyspnea was classified by the New York Heart Association (NYHA) functional classification as II and III in 58% of the patients. Although 27.3% of the patients reported palpitations, only 6% had warning signs extracted by anamnesis. Syncope was an uncommon event (4.1%) (Table 3).
|
Variable |
Description |
|
Dyspnea, n (%) |
70 (41) |
|
NYHA |
|
|
I |
24 (34,2) |
|
II |
35 (50) |
|
III |
6 (8) |
|
IV |
1 (1,4) |
|
Not classified |
4 (5,7) |
|
Chest pain, n (%) |
78 (46,1) |
|
A |
5 (6,4) |
|
B |
8 (10,2) |
|
C |
35 (44,8) |
|
D |
30 (38,4) |
|
Palpitation, n (%) |
47 (27,3) |
|
Without warning sign |
79 (94) |
|
With red flag |
5 (6) |
|
Syncope, n (%) |
7 (4,1) |
|
With prodrome |
3 (1,8) |
|
Without prodrome |
1 (0,6) |
|
Effort-induced |
1 (0,6) |
|
Preceded by chest pain |
1 (0,6) |
|
Preceded by dyspnea |
1 (0,6) |
Table 3: Symptoms
CCS, Canadian Cardiovascular Society; NYHA, New York Heart Association
Physical examination was performed immediately before teleconsultation by a general practitioner and guided by the cardiologist, when necessary. Patients were on average overweight (BMI 27.4 ± 5.1 kg/m2); both mean blood pressure and heart rate values were within the normal range (mean systolic arterial blood pressure 138.6 ± 23.3 mm Hg, mean diastolic arterial blood pressure 85.2 ± 13.4 mm Hg, mean heart rate 72.8 ± 15 beats per minute). Altered physical examination suggestive of heart failure was uncommon, but 7.2% of patients had a heart murmur (Table 4). Concerning pre-existing comorbidities of cardiological importance, hypertension was the most prevalent (66.9%) followed by diabetes (18.6%); 5.9% had altered fasting glycemia and dyslipidemias (12.7%). The study population had a large proportion of sedentarism (92.5%) and low smoking rate (3.7%), similar to national averages, despite previous smoking habits (28.7%). The number of people who reported current use of alcohol is also non-impressive (2.4%). Regarding previous heart disease, only 8.7% reported a heart attack, 2.9% angioplasty and 4.1% myocardial revascularization. Previous ischemic or hemorrhagic stroke and peripheral obstructive arterial disease were present, respectively, in 6.9% and 2.3%, of the population. Valvular heart diseases, structural diseases, pacemaker, implantable defibrillator, and resynchronizer were uncommon (Table 5). There was also little other comorbidity in the patients evaluated, with emphasis on 5.2% with dyspepsia and 5.2% with anxiety (Table 6).
|
Variable |
Description |
|
Weight (Kg) |
|
|
mean ± SD |
68,6 ± 13,5 |
|
Height (cm) |
|
|
mean ± SD |
158,2 ± 7,7 |
|
BMI |
|
|
mean ± SD |
27,4 ± 5,1 |
|
HR (BPM) |
|
|
mean ± SD |
72,8 ± 15 |
|
SBP (mmHg) |
|
|
mean ± SD |
138,6 ± 23,3 |
|
DPB (mmHg) |
|
|
mean ± SD |
85,2 ± 13,4 |
|
Jugular stasis, n (%) |
1 (0,7) |
|
Lower limb edema n (%) |
4/151 (2,6) |
|
Altered lung auscultation, n (%) |
|
|
Crackles |
3 (2) |
|
Wheezing |
1 (0,7) |
|
Heart murmur, n (%) |
11 (7,2) |
Table 4: Physical Examination
BMI, body mass index; BPM, beat per minute; HR, heart rate; DBP, diastolic blood pressure; SBD, systolic blood pressure
|
Variable |
Description |
|
Hypertension, n (%) |
115 (66,9) |
|
Impaired fasting blood glucose, n (%) |
10 (5,9) |
|
Diabetes mellitus, n (%) |
32 (18,6) |
|
Dyslipidemia, n (%) |
21 (12,7) |
|
Sedentary lifestyle, n (%) |
136 (92,5) |
|
Smoking, n (%) |
|
|
Never |
111 (67,7) |
|
Previous |
47 (28,7) |
|
Current |
6 (3,7) |
|
Alcohol use, n (%) |
|
|
Never |
147 (90,7) |
|
Up to the WHO recommended dose |
2 (1,2) |
|
More than the WHO recommended dose |
2 (1,2) |
|
Ex-alcoholic |
11 (6,8) |
|
Myocardial infarction, n (%) |
15 (8,7) |
|
Angioplasty, n (%) |
5 (2,9) |
|
Coronary artery bypass, n (%) |
7 (4,1) |
|
POAD, n (%) |
4 (2,3) |
|
Stroke, n (%) |
|
|
Lacunar ischemic |
4 (2,3) |
|
Lacunar ischemic |
5 (2,9) |
|
Hemorrhagic |
1 (0,6) |
|
Transient ischemic attack, n (%) |
2 (1,2) |
|
Cardiac murmur / Valvular heart disease / Structural disease, n (%) |
|
|
Yes |
15 (9,3) |
|
Previous intervention |
1 (0,6) |
|
Pacemaker, n (%) |
2 (1,2) |
|
Cardiodefibrillator, n (%) |
0 (0) |
|
Resynchronizer, n (%) |
0 (0) |
Table 5: Risk factors for cardiovascular history
POAD, peripheral obstructive arterial disease; WHO, World Health Organization
|
Variable |
Description |
|
Respiratory system disease, n (%) |
|
|
Asthma |
2 (1,2) |
|
Chronic obstructive pulmonary disease |
3 (1,7) |
|
Digestive system disease, n (%) |
|
|
Dyspepsia |
9 (5,2) |
|
History of upper and lower gastrointestinal bleeding |
1 (0,6) |
|
Genito-urinary system disease, n (%) |
|
|
Chronic kidney disease |
4 (2,3) |
|
Kidney tumor |
2 (1,2) |
|
Prostate tumor |
1 (0,6) |
|
Rheumatological disease, n (%) |
|
|
Arthrosis |
1 (0,6) |
|
Arthritis |
1 (0,6) |
|
Osteoporosis |
4 (2,3) |
|
Systemic lupus erythematosus |
1 (0,6) |
|
Psychiatric and neurological disease, n (%) |
|
|
Depression |
4 (2,3) |
|
Anxiety |
9 (5,2) |
|
Epilepsy |
2 (1,2) |
|
Endocrinological disease, n (%) |
|
|
Hypothyroidism |
1 (0,6) |
|
Hyperthyroidism |
2 (1,2) |
|
Hematological and immune disease, n (%) |
|
|
HIV / AIDS |
1 (0,6) |
|
Anemia |
1 (0,6) |
|
HIV, human immunodeficiency virus; AIDS, acquired immunodeficiency syndrome |
|
Table 6: Comorbidities
|
Variable |
Previously prescribed – n (%) |
New Prescribed % |
Discontinued % |
|
ACE inhibitor, n (%) |
18 (11,5) |
4,7 |
1,8 |
|
ARBs, n (%) |
71 (44,1) |
23,1 |
0 |
|
Beta Blocker HF, n (%) |
22 (13,9) |
5,3 |
0 |
|
Spironolactone, n (%) |
10 (6,3) |
1,8 |
0,6 |
|
ARNI, n (%) |
1 (0,6) |
0,6 |
0 |
|
Diuretic, n (%) |
43 (26,9) |
16,6 |
1,2 |
|
Digoxin, n (%) |
1 (0,6) |
0 |
0 |
|
Beta blocker no HF, n (%) |
20 (12,6) |
10,7 |
0,6 |
|
Aspirin, n (%) |
39 (24,4) |
14,2 |
0 |
|
P2Y12 inhibitor, n (%) |
6 (3,8) |
1,2 |
0,6 |
|
Warfarin, n (%) |
2 (1,3) |
0,6 |
0 |
|
New oral anticoagulants, n (%) |
0 (0) |
0 |
0 |
|
Calcium Channel Blocker, n (%) |
24 (15) |
11,2 |
0 |
|
Other antihypertensive, n (%) |
4 (2,5) |
1,8 |
0 |
|
Nitrate, n (%) |
2 (1,3) |
0 |
0 |
|
Other anti-anginal or medicine for POAD, n (%) |
6 (3,8) |
0 |
0,6 |
|
Oral antidiabetic, n (%) |
|||
|
1 medicine |
20 (12,3) |
4,8 |
0 |
|
2 medicine |
6 (3,7) |
0 |
0 |
|
Insulin, n (%) |
|||
|
1 kind |
4 (2,5) |
0 |
0 |
|
New diabetes medicine, n (%) |
1 (0,6) |
0 |
0 |
|
Statin, n (%) |
27 (16,8) |
20,2 |
0 |
|
Fibrate, n (%) |
3 (1,9) |
0,6 |
0 |
|
ACE inhibitor, angiotensin-converting enzyme; ARBs, angiotensin receptor blockers; ARNI, angiotensin receptor-neprilysin inhibitor; HF, heart failure; POAD, peripheral obstructive arterial disease |
|||
Table 7: Medication
This innovative telemedicine project provided therapeutic changes in 77.4% of medical consultations. The mean number of changes per patient was 2.12 + 1.84. There was an increase in 20.2% of statin prescriptions and reduction of diuretics administration. It is important to highlight that in 34.9% of the cases, diuretics were discontinued especially due to postural hypotension. Furthermore, a considerable need was verified for additional diagnostic testing in most of the cases. Among them, electrocardiogram (ECG), transthoracic echocardiogram (TTE), laboratory tests and ischemic evaluation tests were ordered, respectively, in 57.3%, 54.4%, 65.5% and 26.3% of the patients. Due to the need for additional tests, 90.1% of the patients were asked to return.
Discussion
Telemedicine is an efficient method to increase access to health care, particularly evaluation by specialists [17-20]. Implementation of organized teleconsultation might mitigate cardiovascular diseases’ burden in isolated and socio-economically deprived communities. In Brazil, although telemedicine is legally standardized since 2002, development of specific programs is new and still slow. In this regard, the national cardiology consultation program has a very particular patient profile [21].
In the present study, the absence percentage (21.5%) can be considered quite low; especially due to improvements in health care access this specific telemedicine project was offered to the population in northern Brazil. Usually, the wait time for specialist consultations can be many months and this specific population has huge mobility and transportation issues, many times taking several hours to get to the health care facility.
As this population has been previously screened by a healthcare provider, it was expected to see a profile of high complexity cardiologic patients, but this is not what the analyses revealed. The population attended had few morbid heart conditions, but without optimized treatment for hypertension and dyslipidemia, as recommended by international guidelines. Was observed that lifestyle is compromised, as there is high prevalence of overweight and sedentary individuals, and high rate of previous smokers, although the rate of active smokers is low. All the data can contribute to the improvement of health policies by regional authorities on several different levels, from basic health care in solving the less complex cases to a population level effort of improving lifestyle measures.
Even though most medical literature considers higher prevalence of the cardiovascular disease in male subjects, the present study showed higher prevalence of female subjects needing cardiology consultation. This is probably due to cultural aspects of the male Brazilian population, in which is noticed great difficulty in convincing them to seek medical care, for several reasons, whether personal or socio-economic.
From the present data, we acknowledge that most chest pain consultations are of medium to low probability of coronary artery disease. Its correct stratification, especially in limited-resource settings, is extremely important to optimize cost-effectiveness of the health care system, which in our opinion can be best achieved with specialist consultation.
The present study provided increase in statin prescription compared with previous care, critical for cardiovascular patients with atherosclerosis and may improve outcomes on follow-up.
Telemedicine applied to cardiology will play a particularly important role when there is lack of resources or unavailability of access to health care. There are populations with few resources or in places with difficult access to health professionals in Brazil, due to regional, cultural and socio-economic characteristics. In these cases, the opportunity to use instruments for effective prevention, diagnosis, treatment, as well as monitoring cardiovascular diseases, opens the doors for excellent perspectives in these populations and communities’ health care.
Several opportunities for improvement in the expansion of this program and in supporting the implementation of other programs alike were found. Regarding the reason for referral, probably a therapeutic update to general practitioners on risk factor control could have a significant impact, as well as guidance for perioperative evaluations of surgeries and low-risk patients. Patients living in remote areas must have government assistance for transportation and access to consultation. It is essential to proceed with teleconsultation after standardized anamnesis, physical exam and basic diagnostic tests are available. In this way, consultation can be more focused on the specialist's questions with more rational use of resources and better specialist time optimization. It may be important to increase consultation time for complex and very symptomatic patients.
Probably, prescription improvement to 75% of patients might have a good impact on reducing the burden of cardiovascular diseases. Thus, we believe periodic census to assess the implementation of telemedicine guideline recommendations, as well as more health-trained professionals in this area, can be useful to improve local health conditions.
We must always remember that bioethical aspects cannot be neglected and, therefore, regulated operational models, based on guidelines organized by medical-scientific authorities, are essential to find a balance to avoid abuses and misuse of this technology.
Conclusions
Telemedicine applied to cardiology specialist consultations is an acceptable alternative to remote Brazilian regions with limited resources. It is necessary to standardize referral and service conditions and training of local staff in teleconsultation. With the implementation of the project, data can demonstrate points of improvement in the local health system and theoretically benefit patients and managers through several aspects, potentially in a cost-effective way, including faster access to specialists, rational use of resources, optimization of prescription and better quality of care.
Acknowledgments
We thank the "Programa de Desenvolvimento Institucional do Sistema Único de Saúde (PROADI-SUS)" of the Ministry of Health of Brazil and the "Instituto Israelita de Responsabilidade Social Albert Einstein (IIRS)" for the service provided.
Conflicts of interest statement
The authors declare they have no conflicts of interest related to the present manuscript.
Funding
The project was funded by the "Programa de Desenvolvimento Institucional do Sistema Único de Saúde (PROADI-SUS)" of the Ministry of Health of Brazil.
References
- World Health Organization. (WHO). Digital Atlas Health [Internet]. Available from: https://digitalhealthatlas.org/en//
- Singh G, O'Donoghue J, Soon CK. Telemedicine: issues and implications. Technology and Health Care 10 (2002): 1-10.
- Volterrani M, Sposato B. Remote monitoring and telemedicine. Eur Heart J Suppl 21 (2019): M54–M56.
- Hersh W, Helfand M, Wallace J, et al. A systematic review of the efficacy of telemedicine for making diagnostic and management decisions. Journal of Telemedicine and Telecare 8 (2002): 197-209.
- Federal Council of Medicine (CFM-Brasil). CFM Resolution 2,227 / 2018: defines and disciplines telemedicine as a way of providing medical services mediated by technology. Available from: https://portal.cfm.org.br/images/PDF/resolucao222718.pdf
- Brazilian Institute of Geography and Statistics. (IBGE). Classification and characterization of rural and urban spaces in Brazil; a first approximation. Rio de Janeiro (2017). (Studies and Research - Geographic Information. N.11)
- Brazilian Institute of Geography and Statistics. (IBGE). Mapping system for territorial base - SISMAI - User Manual. Rio de Janeiro (2010).
- Brazilian Institute of Geography and Statistics. (IBGE). IBGE 2010 Census. Available from: ps: // censo2010. ibge.gov.br (2010).
- Scheffer M, Biancarelli A, Cassenote A. Demografia médica no Brasil 2015 [Internet]. São Paulo: Departamento de Medicina Preventiva, Faculdade de Medicina da USP (2018): 284.
- Ministry of Health. National Registry of Health Establishments. [Internet]. Available from: http: // cnes. datasus.gov.br/ (2019).
- Lopes MA, Oliveira GM, Ribeiro AL, et al. Guideline of the Brazilian Society of Cardiology on Telemedicine in Cardiology-2019. Arquivos Brasileiros de Cardiologia 113 (2019): 1006-1056.
- Dierckx R, Inglis SC, Clark RA, et al. Telemedicine in heart failure: new insights from the Cochrane meta-analyses. European Journal of Heart Failure 19 (2017): 304-306.
- Delgoshaei B, Mobinizadeh M, Mojdekar R, et al. Telemedicine: A systematic review of economic evaluations. Medical journal of the Islamic Republic of Iran 31 (2017): 113.
- Naser N, Tandir S, Begic E. Telemedicine in Cardiology-Perspectives in Bosnia and Herzegovina. Acta Informatica Medica 25 (2017): 263.
- Escobar-Curbelo L, Franco-Moreno AI. Application of telemedicine for the control of patients with acute and chronic heart diseases. Telemedicine and e-Health 25 (2019): 1033-1039.
- Comín-Colet J, Enjuanes C, Verdú-Rotellar JM, et al. Impact on clinical events and healthcare costs of adding telemedicine to multidisciplinary disease management programmes for heart failure: Results of a randomized controlled trial. Journal of Telemedicine and Telecare 22 (2016): 282-295.
- Kuehn BM. Telemedicine helps cardiologists extend their reach. Circulation 134 (2016): 1189-1191.
- Stahl JN, Zellner C, Chou TM. Telemedicine in cardiology. Am Heart J 138 (1999): 1200.
- Maldonado JM, Marques AB, Cruz A. Telemedicina: desafios à sua difusão no Brasil. Cad Saúde Pública 32 (2016): e00155615.
- Mattos SD, Hazin SM, Regis CT, et al. A telemedicine network for remote paediatric cardiology services in north-east Brazil. Bulletin of the World Health Organization 93 (2015): 881-887.
- Federal Council of Medicine. Resolutions / CFM / 2002/1642 [Internet]. Available from: http://www.portalmedico.org.br/resolucoes/CFM/2002/1642_2002.htm
- Baldwin L, Clarke M, Hands L, et al. The effect of telemedicine on consultation time. J Telemed Telecare 9 (2003): S71–S73.
