Aggressive form of Pancreatitis Worsened by Tuberculous Pleuritis
Article Information
Rosana Manea1, Lavinia Raicu2*
Head of the Department of Radiology and Medical Imaging, Transilvania University of Brasov, Emergency Clinical Hospital Brasov, Brasov, Romania
Medical Resident, Department of Radiology and Medical Imaging, Emergency Clinical Hospital Brasov, Brasov, Romania
*Corresponding Author: Dr. Lavinia Raicu, Medical Resident, Department of Radiology and Medical Imaging, Emergency Clinical Hospital Brasov, Brasov, Romania, E-mail: lavinia.raicu47@gmail.com
Received: 19 October 2020; Accepted: 11 November 2020; Published: 02 December 2020
Citation: Rosana Manea, Lavinia Raicu. Aggressive form of Pancreatitis Worsened by Tuberculous Pleuritis. Archives of Clinical and Medical Case Reports 4 (2020): 1146-1150.
View / Download Pdf Share at FacebookAbstract
Pancreatitis is an acute or chronic inflammatory condition caused by the disruption of exocrine pancreatic cells by the invasion of inflammatory cells. There are two subtypes of pancreatitis: interstitial edematous pancreatitis and necrotising pancreatitis. One of the most common cause of acute and chronic pancreatitis is alcohol use. Diagnostic criteria are usually used where a patient has distinctive signs, elevated amylase and lipase levels, and specific imaging findings. Treatment is usually supportive, there is no particular pharmacotherapy for this disorder [1]. We present the case of a 37-year-old man known with chronic pancreatitis worsened by massive pleural effusion with TB, presented to our hospital with shortness of breath. Globally, the incidence of TB effusions is higher in younger patients. Confirmed diagnosis was based upon histopathological and CT imaging results.
Keywords
Pancreatitis; Necrotizing pancreatitis; Extra-Pulmonary tuberculosis; Pleural biopsy; Pleural effusion
Article Details
1. Case Presentation
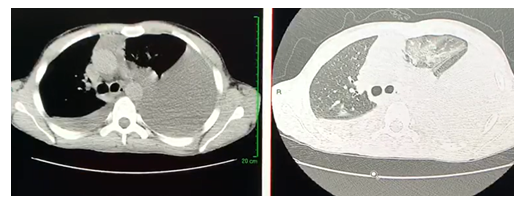
Thirty-seven-year-old male presented to the emergency department for evaluation of shortness of breath, abdominal pain, nausea, and shivering. Twelve months before, he was diagnosed with acute pancreatitis treated at home by his doctor. He has been a chronic alcoholic and he gave up alcohol when he was diagnosed with pancreatitis. He is also an ex-smoker. Computed tomography of the chest presented a massive pleural effusion, predominantly on the left pleural cavity, with a mediastinal shift towards the right. This was perceived initially as a complication of chronic
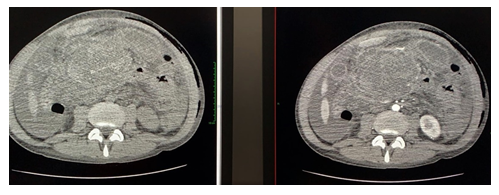
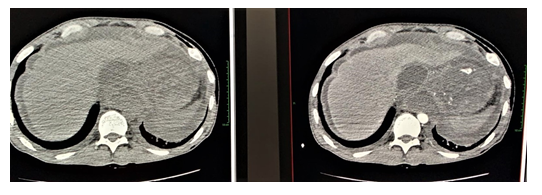
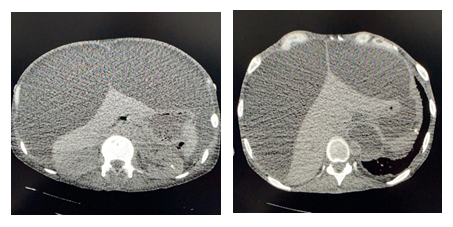
pancreatitis. Contrast-enhanced abdominal CT scan revealed a low-attenuation multiloculated collection with a relatively thick wall, with multiple hyperdense lesions included, localized in the omental bursa, with maximum dimensions of 8/13/14 cm. The erosion of the wall of the splenic artery by the pancreatic pseudocyst was also seen, a rare and highly lethal complication of pancreatitis. All of these findings were compatible with acute hemorrhagic-necrotizing pancreatitis. Free intraperitoneal fluid was also observed. Only a small part of the pancreatic tail was visible.
Blood tests from the first evaluation suggested neutrophilic leukocytosis (24 000 uL), mild anemia, hyperamylasemia (242 U/l), and a high level of CRP. All of these markers suggested acute pancreatic injury. Other blood parameters were unremarkable. The doctor performed immediate thoracocentesis and evacuated 2000 ml of sero-hemorrhagic fluid, with clinical improvement. The indication for diagnostic left thoracoscopy has been established and 5000 ml of sero-hemorrhagic fluid has been evacuated. Hyperemic parietal and visceral pleura was visualized with diffused white-gray pseudo-tumor lesions. Pleural biopsy revealed the presence of Mycobacterium tuberculosis in the pleural fluid. The evolution is subsequently accompanied by an intense thoracic and abdominal pain that requires fentanyl analgesic therapy. The patient refuses surgical consult for the abdominal collection and requested to be discharged at his own risk. He followed the advice for consultation and antituberculosis treatment. After two months, the patient returns to the emergency department with intense abdominal pain, abdominal distension, cachexia, hemodynamically unstable, and acute respiratory failure. An abdominal CT scan revealed increased peritoneal fluid, followed by paracentesis. The patient was unstable for laparotomy and he underwent supportive treatment.
2. Discussion
Tuberculosis is a major public health problem in some developed countries. The rate of TB effusions is higher in younger patients. While most people with TB have pulmonary TB, 25 percent of patients have pleural TB manifestations as an initial presentation. TB pleural effusions usually are characterized by fever (~85%), unilateral pleuritic chest pain (~75%), cough (~70%), dyspnea (~50%), night sweats (~50%) and weight loss (25–85%) [3-5]. The primary imaging tool with a high degree of accuracy for patients with acute pancreatitis is contrast-enhanced CT. It is also suited for staging, assess complications, and monitoring of treatment response. As for the patients who have no clinical signs of severe pancreatitis, contrast-enhanced CT is not indicated. The ideal time for evaluating pancreatitis-related complications is 72 hours after the onset of symptoms. If the clinical picture changes dramatically, CT should be repeated. CT is also useful to guide the positioning of catheters for drainage and to determine treatment progress in patients with pancreatitis [6].
The late stage of pancreatitis starts after the first week, can last for weeks to months, and is characterized by increased necrosis, inflammation, and recurrent multi-organ failure. Local complications include peripancreatic fluid collection, pancreatic or peripancreatic tissue necrosis (necrotizing pancreatitis), as defined in the updated Atlanta criteria. Walled-off necrosis or encapsulated collection of pancreatic or peripancreatic necrosis with an inflammatory wall usually occurs after four weeks by the onset of necrotizing pancreatitis [7]. Another sign of chronic inflammation is calcification throughout the pancreas [8]. The patient suffered from multiple organ failure with TB pleural infection and was unable to undergo surgery, thereby the peripancreatic abdominal collection evolved to severe acute pancreatitis with unfavorable prognostic signs. Furthermore, the patient needed TB treatment with close monitoring and minimally invasive radiologic procedures to improve the clinical condition. Unfortunately, while the doctors have tried their best to save him, the patient has not survived.
3. Conclusion
We presented a patient with chronic pancreatitis initially presented for massive pleural effusion, evolving to severe acute pancreatitis with large abdominal multiloculated collection, exacerbated due to TB infection, with unfavorable prognostic signs. The erosion of the wall of the splenic artery by the pancreatic pseudocyst was also seen on contrast-enhanced abdominal CT, a rare and highly lethal complication of pancreatitis.
References
- Klochkov A, Kudaravalli P, Sun Y. Alcoholic Pancreatitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing (2020).
- Shaw JA, Diacon AH, Koegelenberg CFN. Tuberculous pleural effusion. Respirology 24 (2019): 962-971.
- Baumann MH, Nolan R, Petrini M, et al. Pleural tuberculosis in the United States: incidence and drug resistance. Chest 131 (2007): 1125-1132.
- Berger HW, Mejia E. Tuberculous pleurisy. Chest 63 (1973): 88-92.
- Light RW. Update on tuberculous pleural effusion. Respirology 15 (2010): 451-458.
- Thoeni RF. The revised Atlanta classification of acute pancreatitis: its importance for the radiologist and its effect on treatment. Radiology 262 (2012): 751-764.
- Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis-2012: revision of the Atlanta classification and definitions by international consensus. Gut 62 (2013): 102-111.
- Sechel G, Repanovici A, Manea R, et al. The imaging evaluation of typical and atypical calcifications in different anatomical regions study in Brasov, Romania. The Medical-Surgical Journal 123 (2020): 290-297.