Acquired Clitoromegaly Cyst: Consequence of Persistent Unorthodox Practice in the 21st Century
Article Information
Olutosin Alaba Awolude1*, Oluyomi Akinyotu2
1Department of Obstetricst and Gynaecology, College of Medicine, University of Ibadan/University College Hospital, Ibadan, Nigeria
2Department of Obstetricst and Gynaecology, University College Hospital, Ibadan, Nigeria
*Corresponding Author: Olutosin Alaba Awolude, Department of Obstetricst and Gynaecology, College of Medicine, University of Ibadan/ University College Hospital, Ibadan, Nigeria
Received: 02 July 2019; Accepted: 29th July 2019; Published: 26 August 2019
Citation:
Olutosin Alaba Awolude, Oluyomi Akinyotu. Acquired Clitoromegaly Cyst: Consequence of Persistent Unorthodox Practice in the 21st Century. Obstetrics and Gynecology Research 2 (2019): 043-049.
View / Download Pdf Share at FacebookAbstract
Objective: To present case report a patient with clitoral cyst, following type II female genital cutting performed in childhood, management and literature review.
Design: Report of cases managed and review of available current literatures.
Setting: University College Hospital Ibadan.
Patients: The case was a 30 year old Para 2+0 , 2 alive, known hypertensive, with perineal swelling since childhood. She presented 30 years later with increasing size of the clitoral swelling associated with pain.
Management: Surgical excision of the cyst following thorough evaluation of the patients.
Results: Better cosmetic outcome, vulvar discomfort subsided and improved sexual satisfaction post-operatively.
Conclusion: While a good cosmetic and stoppage of vulvar discomfort can be managed with acceptable outcomes, these case, again, brings to attention of persistence of unacceptable female genital cutting with attendant effects even in the 21st century. Also, to let us know that there is need for more and continuous awareness creation of the need to stop this dehumanizing practice, of female genital cutting, which is of no health importance, rather numerous adverse sequelae.
Keywords
Female genital cutting; Clitoral cyst; Complications
Female genital cutting articles Female genital cutting Research articles Female genital cutting review articles Female genital cutting PubMed articles Female genital cutting PubMed Central articles Female genital cutting 2023 articles Female genital cutting 2024 articles Female genital cutting Scopus articles Female genital cutting impact factor journals Female genital cutting Scopus journals Female genital cutting PubMed journals Female genital cutting medical journals Female genital cutting free journals Female genital cutting best journals Female genital cutting top journals Female genital cutting free medical journals Female genital cutting famous journals Female genital cutting Google Scholar indexed journals Clitoral cyst articles Clitoral cyst Research articles Clitoral cyst review articles Clitoral cyst PubMed articles Clitoral cyst PubMed Central articles Clitoral cyst 2023 articles Clitoral cyst 2024 articles Clitoral cyst Scopus articles Clitoral cyst impact factor journals Clitoral cyst Scopus journals Clitoral cyst PubMed journals Clitoral cyst medical journals Clitoral cyst free journals Clitoral cyst best journals Clitoral cyst top journals Clitoral cyst free medical journals Clitoral cyst famous journals Clitoral cyst Google Scholar indexed journals Complications articles Complications Research articles Complications review articles Complications PubMed articles Complications PubMed Central articles Complications 2023 articles Complications 2024 articles Complications Scopus articles Complications impact factor journals Complications Scopus journals Complications PubMed journals Complications medical journals Complications free journals Complications best journals Complications top journals Complications free medical journals Complications famous journals Complications Google Scholar indexed journals Obstetricst articles Obstetricst Research articles Obstetricst review articles Obstetricst PubMed articles Obstetricst PubMed Central articles Obstetricst 2023 articles Obstetricst 2024 articles Obstetricst Scopus articles Obstetricst impact factor journals Obstetricst Scopus journals Obstetricst PubMed journals Obstetricst medical journals Obstetricst free journals Obstetricst best journals Obstetricst top journals Obstetricst free medical journals Obstetricst famous journals Obstetricst Google Scholar indexed journals Gynaecology articles Gynaecology Research articles Gynaecology review articles Gynaecology PubMed articles Gynaecology PubMed Central articles Gynaecology 2023 articles Gynaecology 2024 articles Gynaecology Scopus articles Gynaecology impact factor journals Gynaecology Scopus journals Gynaecology PubMed journals Gynaecology medical journals Gynaecology free journals Gynaecology best journals Gynaecology top journals Gynaecology free medical journals Gynaecology famous journals Gynaecology Google Scholar indexed journals urinary meatus articles urinary meatus Research articles urinary meatus review articles urinary meatus PubMed articles urinary meatus PubMed Central articles urinary meatus 2023 articles urinary meatus 2024 articles urinary meatus Scopus articles urinary meatus impact factor journals urinary meatus Scopus journals urinary meatus PubMed journals urinary meatus medical journals urinary meatus free journals urinary meatus best journals urinary meatus top journals urinary meatus free medical journals urinary meatus famous journals urinary meatus Google Scholar indexed journals vaginal introitus articles vaginal introitus Research articles vaginal introitus review articles vaginal introitus PubMed articles vaginal introitus PubMed Central articles vaginal introitus 2023 articles vaginal introitus 2024 articles vaginal introitus Scopus articles vaginal introitus impact factor journals vaginal introitus Scopus journals vaginal introitus PubMed journals vaginal introitus medical journals vaginal introitus free journals vaginal introitus best journals vaginal introitus top journals vaginal introitus free medical journals vaginal introitus famous journals vaginal introitus Google Scholar indexed journals Labia majora articles Labia majora Research articles Labia majora review articles Labia majora PubMed articles Labia majora PubMed Central articles Labia majora 2023 articles Labia majora 2024 articles Labia majora Scopus articles Labia majora impact factor journals Labia majora Scopus journals Labia majora PubMed journals Labia majora medical journals Labia majora free journals Labia majora best journals Labia majora top journals Labia majora free medical journals Labia majora famous journals Labia majora Google Scholar indexed journals Pelvic articles Pelvic Research articles Pelvic review articles Pelvic PubMed articles Pelvic PubMed Central articles Pelvic 2023 articles Pelvic 2024 articles Pelvic Scopus articles Pelvic impact factor journals Pelvic Scopus journals Pelvic PubMed journals Pelvic medical journals Pelvic free journals Pelvic best journals Pelvic top journals Pelvic free medical journals Pelvic famous journals Pelvic Google Scholar indexed journals vulvar incision articles vulvar incision Research articles vulvar incision review articles vulvar incision PubMed articles vulvar incision PubMed Central articles vulvar incision 2023 articles vulvar incision 2024 articles vulvar incision Scopus articles vulvar incision impact factor journals vulvar incision Scopus journals vulvar incision PubMed journals vulvar incision medical journals vulvar incision free journals vulvar incision best journals vulvar incision top journals vulvar incision free medical journals vulvar incision famous journals vulvar incision Google Scholar indexed journals
Article Details
1. Introduction
World Health Organization (WHO) defines female genital mutilation (FGM) as “all procedures that involve partial or total removal of the external female genitalia or other injury to the female genital organs for cultural or other nontherapeutic reasons” [1]. Other synonyms are female genital cutting or female circumcision. The time of performance of the procedure varies from time to time depending on the culture of the people. It can be performed in infancy, at the time of initiation into womanhood or just before marriage. The procedure is practiced mainly in African countries, and an estimated 130 million women worldwide have had it done in some form [1]. Annually, over two million procedures of FGM are performed globally [2]. Nigeria as a result of its high population has the highest absolute number of FGM accounting for about a quarter of the estimated 115-130 million women circumcised worldwide. The national prevalence rate of FGM in Nigeria is 41% among adult women [3].
Despite the abundance information of the lack of benefit of this practice and the associated complications, this procedure of female genital cutting is still common in our environment. It is, therefore, our responsibility as health care workers to constantly draw the attention of the public to the observed complications following FGM and its associated emotional, health, social and economic implications. Associated reproductive health sequalae of FGM include haemorrhage with or without shock, infection especially bacterial vaginosis and herpes simplex type-II, [4], obstetrics sequale like pelvic outlet-associated difficult labour, clitoral scarring and cyst formation (clitoral epidermoid inclusion cyst) with resultant psychological and sexual problems [5]. In this report, we describe a case of a multiparous female adult with a histologically confirmed epidermoid inclusion cyst of the clitoris who had a history of type II FGM performed as a neonate.
2. Case Presentation
This is a case of 30-year old Para 2+0, 2 alive woman who presented at the Gynaecology clinic, University College Hospital, Ibadan, Nigeria, with a swelling at the upper part of the external genitalia which she noticed since childhood. There was a history of circumcision in childhood like her other two senior female siblings. She first noticed this as a small clitoral mass as a teenager, with occasional itchy sensations. The patient had never sought any medical treatment for prior to this presentation. A month prior to presentation she noticed progressive increase in size with associated tenderness. There was no swelling in any other part of the body. The patient had been married for 6 years and had no history of dyspareunia, or urinary symptoms. She has had 2 normal full term and spontaneous vaginal deliveries. Both children were alive and well. Patient was a known hypertensive diagnosed in 2013 and managed on Tabs Methyldopa. She had excision of a left breast lump in 2008, with histological diagnosis of fibroadenoma.
The main finding on physical examination was Type II female genital mutilation, a, well-circumscribed, mobile, nontender, round, cystic mass about 8cm x 6 cm on the partially amputated clitoris with no differential warmth (Figure 1). The urinary meatus and vaginal introitus were identified and normal. the labia minora were absent. Labia majora were preserved. Pelvic ultrasound done was reported normal.

Figure 1: Acquired Clitoromegaly Cyst
She was appropriately counseled and scheduled for surgical removal under anaesthesia. Pre-surgery haematological and chemical investigations were normal. She had surgical resection of the mass with aesthetic repair of the vulvar incision under sub-arachnoid block anaesthesia. Intraoperative findings included the presence of a well-demarcated, encapsulated subcutaneous cystic 6cm x 8cm x 10cm mass containing gelatinous material. This was dissected completely from the surrounding structures via a midline incision made on the swelling (Fig. 2). The neurovascular bundle of the clitoral area was spared. After hemostasis, the skin was approximated with a continuous suture, without trimming of the redundant tissues.

Figure 2: Dissection of the Clitoral Cyst
The cystic mass (Fig.3) containing gelatinous materials was sent for histological assessment.
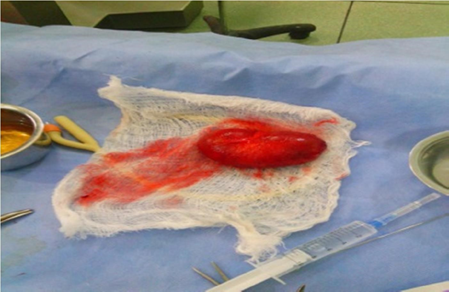
Figure 3: Clitoral cystic specimen
The postoperative period was without any complications. During the follow-up at outpatient clinic one-month post-surgery, there was no complaint. The pathologic examination of the excised clitoral mass showed stratified squamous epithelium with overlying collagenous tissue and containing desquamated keratinous materials. The histopathology conclusion was that of epidermoid inclusion cyst. The follow-up of the patient at the second postoperative visit a month later revealed no recurrence, with a fine cosmetic result. The patient reported complete resolution of her complaints, absence of dyspareunia and satisfactory sexual relationship with her husband. There was no hypertrophic scar tissue on the perineum.
3. Discussion
Clitoral cyst is an epidermoid inclusion cyst, a slowly growing, intradermal cyst of the clitoris in female, mostly, as a result of female genital mutilation (FGM), a procedure which involves partial or total removal of the external female genitalia, for cultural or non-therapeutic indications [6-9]. The FGM associated clitoral epidermoid inclusion cysts are non-hormonal cause of clitoromegaly [6,10,11]. However, hormonal conditions such as endocrinopathies, masculinizing tumors, exposure to the androgens, pseudo-clitoromegaly due to masturbation, and clitoral neurofibromatosis are the other causative factors in the aetiology of the acquired clitoral enlargement [12]. Spontaneous onset of this clitoral lesion is rare [7]. The inclusion cyst arises from the invagination of keratinizing squamous epithelium within the dermis, accumulation of epidermal desquamations, secretions and other debris in a circumscribed space which becomes cystic and filled with laminated keratin [13]. The formed cyst is often painless and gradually increases in size over time [14].
The WHO has classified female genital mutilation into four types: Type I: Partial or total removal of the clitoris and/or the prepuce (clitoridectomy); Type II: Partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora (excision); Type III: Narrowing of the vaginal orifice with creation of a covering seal by cutting and apposition of the labia minora and/or the labia majora, with or without excision of the clitoris (infibulation); Type IV: Unclassified and described as all other harmful procedures to the female genitalia for non-medical purposes. Example of the type IV include ‘’introcision’’ (splitting of the vaginal opening with sharp objects or the fingers) , cutting of the vaginal wall or the cervix, pricking or piercing or stretching of the clitoris or the labia, cauterization by burning of the clitoris and surrounding tissue , scraping of the tissue surrounding the vaginal orifice (‘’angurya’’ cuts) or cutting the vagina (‘’gishiri’’ cuts), introduction of corrosive substances or herbs into the vagina to cause bleeding or for purposes of tightening or narrowing it and any other procedure that falls under the definition of female genital mutilation [6]. Types I and II FGM are the most practiced worldwide constituting 80% of cases as seen in our case (Type II FGM), the more extreme type III FGM are commoner in many African countries home to majority of cases of FGM [1,15]. This report describes a case of epidermal clitoral inclusion cyst as a long-term complication of type II FGM in an adult female with latency period of 3 decades. Long term complications of female genital mutilation include chronic pain, infections, inclusion cysts and abscesses (which might be the cause of the pain in this patient), decreased sexual enjoyment, infertility, posttraumatic stress disorder, urinary dysfunction, and dangers in childbirth [3].
The clinical presentation of epidermal inclusion cyst of the clitoris usually consists of a silent course with a painless swelling gradually increasing in size [6,7,16]. A soft, mobile, nontender mass in the clitoral region in the absence of any virilization sign is the typical physical finding, which are similar with the findings in our patient.
Late presentation, which is the norm, following complications as seen in this case above has been attributed to,essentially, symptomless nature in most cases, ignorance, shame about discussing issues concerning the genital areas, financial constraints and fear of prosecution in countries where female genital mutilation is illegal [10].
Complications associated with clitoral cyst include superficial dyspareunia, urinary disturbances, pain in the vulva, as seen in this case, and infection which may necessitate presentation at the hospital by the patient [17,18].
Management of clitoral cyst is by complete surgical excision. The surgical technique used in our case for removal of the cyst was like in some other cases reported in literature [6-8,19]. The cyst was easily dissected from the surrounding structures through a midline incision made on the overlying skin of the mass. The preservation of the neurovascular bundle was provided during the dissection of this region. Post-operative review showed good healing with satisfactory cosmetic appearance. Other techniques of skin incision include the use of ‘reverse V-shaped incision’ which is said to omit the necessity for skin trimming [20]. However, this case demonstrated that skin trimming can, also, be avoided in the linear, midline incision approach.
Our patient was an adult, multiparous Nigerian woman with long-standing and large epidermoid cyst from FGM performed as neonates with presentation about 30 years later due to pain, possibly, following an infective process. This case was successfully managed surgically with resolution of symptoms. What was difficult to adequately assessed but has been documented in literature is the associated improved quality of life and spousal relationship following successful outcomes [18]. However, this can be assumed in this case of ours from her follow-up clinic review that confirmed absence of dyspareunia and satisfactory sexual relationship with her husband.
4. Conclusion
Clitoral cyst is still a common but relatively under reported long-term complication of female genital mutilation in our environment and many other parts of the world. It is important to continue to create awareness amongst women, generally, and ethnic groups that indulge in the practice of female genital mutilation about the myriad of complications both early and late which can arise as a result of this harmful practice. Enlightenment of women about availability of safe surgical procedures for removal of clitoral cyst and need for early presentation is very important. Even at that, stoppage of FGM remains the ultimate because the patients are still at risk of many of the unpredictable, but known, anaesthesia and surgery-related complications that can arise.
References
- World Health Organization. Female genital mutilation. Geneva: World Health Organization, 1997.
- Aseel Hamoudi. Late Complications of Childhood Female Genital Mutilation. Journal of Obstetrics and Gynaecology Canada 32 (2010): 587-589
- TC Okeke, USB Anyaehie and CCK Ezenyeaku . An overview of Female Genital Mutilation in Nigeria. Ann Med Health Sci Res 2 (2012): 70-73
- Linda Morison Caroline Scherf, Gloria Ekpo, Katie Paine, Beryl West, Rosalind Coleman, Gijs Walraven. The long?term reproductive health consequences of female genital cutting in rural Gambia: a communitybased survey. Tropical Medicine and International Health 6 (2001): 643-653
- Lorensen GJ. Female genital mutilation. Am J Obstet Gynecol 172 (1995): 1320–1321.
- Rizk DE, Mohammed KH, Joshi SU, Al-Shabani AY, Bossmar TR. A large clitoral epidermoid inclusion cyst first presenting in adulthood following childhood circumcision. J Obstet Gynaecol 27 (2007): 446-448
- Yoong WC, Shakya R, Sanders BT, Lind J. Clitoral inclusion cyst: a complication of type I female genital mutilation. J Obstet Gynaecol 24 (2004): 98-99
- Rouzi AA, Sindi O, Facharzt BR, Ba’aqeel H. Epidermal clitoral inclusion cyst after type I female genital mutilation. Am J Obstet Gynecol 185 (2001): 569571
- Hanly MG, Ojeda VJ. Epidermal inclusion cysts of the clitoris as a complication of female circumcision and pharaonic infibulation. Cent Afr J Med 41(1995): 22-24.
- Çöpçü E, Akta? A, Sivrioglu N, Çöpçü Ö, Öztan Y. Idiopathic isolated clitoromegaly: a report of two cases.
- Reprod Health 1(2004): 4.
- Linck D, Hayes MF. Clitoral cyst as a cause of ambiguous genitalia. Obstet Gynecol 99 (2002): 963966.
- Horejsi J. Acquired clitoral enlargement – diagnosis and treatment. Ann N Y Acad Sci 816 (1997): 369-372.
- Hak Soo Lee, Kyung Bin Joo, Ho Taek Song, Yong Soo Kim,Dong Woo Park, et al. Relationship between sonographic and pathologic findings in epidermal inclusion cysts. J Clin Ultrasound 29 (2001): 374383. 3.
- Wondimu Gudu. Acute vulvar pain in a lady with post circumcision inclusion cyst of the vulva containing stones: a case report. BMC Women’s Health 14 (2014): 2.
- Sudan Federal Ministry of Health. Sudan safe motherhood survey 1999.
- Çetinkur?un S, Narci A, Sahin O, Özkaraca E. Epidermoid cyst causing clitoromegaly in a child. Int J Gynaecol Obstet 105 (2009): 64.
- Albert Asante, Kenan Omurtag and Carla Roberts. Epidermal inclusion cyst of the clitoris 30 years after female genital mutilation; Fertility and Sterility® 94 (2010).
- Ozer Birge, Mustafa Melih Erkan, and Aliye Nigar Serin. Case report: epidermoid inclusion cyst of the clitoris as a long-term complication of female genital mutilation. J Med Case Rep 13 (2019): 109
- Fedele L, Fontana E, Bianchi S, Frontino G, Berlanda N. An unusual case of clitoromegaly. Letters to the Editor. Eur J Obstet Gynecol Reprod Biol 140 (2008): 287-288.
- Neslihan Çelik, ?ule Yalç?n, ?afak Güçer, ?brahim Karnak. Clitoral epidermoid cyst secondary to blunt trauma in a 9-year-old child. The Turkish Journal of Pediatrics 53 (2011): 108-110.
