A Study on Premenstrual Syndrome among Female Students of a Private University of Delhi NCR
Article Information
Surbhi Teotia1 , Sayantika Kumari1, Neha Taneja2*, Karuna Nidhi Kaur1, Aanchal Anant Awasthi2, Rajiv Janardhanan3
1Student, Laboratory of Disease Dynamics & Molecular Epidemiology, Amity Institute of Public Health, Amity University, Uttar Pradesh, India
2Assistant Professor, Laboratory of Health Data Analytics & Visualization Environment, Amity Institute of Public Health, Amity University, Uttar Pradesh, India
3Director & Head, Laboratory of Disease Dynamics & Molecular Epidemiology, Laboratory of Health Data Analytics & Visualization Environment, Amity Institute of Public Health, Amity University, Uttar Pradesh, India
*Corresponding author: Neha Taneja, Assistant Professor, Laboratory of Disease Dynamics & Molecular Epidemiology, Laboratory of Health Data Analytics & Visualization Environment, Amity Institute of Public Health, Amity University, Noida, Uttar Pradesh, India
Received: 29 August 2020; Accepted: 10 September 2020; Published: 06 October 2020
Citation:
Surbhi Teotia, Sayantika Kumari, Neha Taneja, Karuna Nidhi Kaur, Aanchal Anant Awasthi, Rajiv Janardhanan. A Study on Premenstrual Syndrome among Female Students of a Private University of Delhi NCR. Journal of Women’s Health and Development 3 (2020): 413-422.
View / Download Pdf Share at FacebookAbstract
Background: Premenstrual Syndrome (PMS) is one of the most common disorders of reproductive age. PMS is a set of physical and psychological symptoms that occurs during the luteal phase of menstrual cycle (14 days before menstrual period), resolved with the onset of menstruation and with a symptom-free interval afterwards. Aim: To assess the knowledge, most commonly reported symptoms, effects on educational activities and interpersonal relationships, treatment options and attitude of female university students towards PMS.
Methods: This cross-sectional study was conducted among 130 female students of a Private University of Delhi NCR. A pretested, self-administered questionnaire was used to collect the information. The data was compiled in Microsoft excel and analysed using SPSS 25 version. P-value <0.05 was considered statistically significant.
Results: The majority (80%) of female participants knew about PMS while only (43.8%) knew about PMDD. The most common affective and somatic symptoms among participants were irritability (74.6 %) and abdominal bloating (48.5%). More than half (53.8 %) of the female participants reported PMS impaired their College/work efficiency/ productivity and Concentration and (49.2 %) reported PMS impaired their Social life activities. The majority (90%) of female participants think that PMS is an important issue that should be discussed but (40.8%) did nothing to relieve their premenstrual symptoms. The female participants of age group between 23 and 30 years showed higher proportion of knowledge of PMS (n=52, 89.7 %) when compared to female participants of age group between 17 and 22 years and this association was statistically significant (P<0.05). The female participants who did exercise showed higher proportion of knowledge of PMS (n=82, 84.5 %) when compared to female students who did not exercise and this association was statistically signific
Keywords
Premenstrual Syndrome, Female Students, Private University
Premenstrual Syndrome articles Premenstrual Syndrome Research articles Premenstrual Syndrome review articles Premenstrual Syndrome PubMed articles Premenstrual Syndrome PubMed Central articles Premenstrual Syndrome 2023 articles Premenstrual Syndrome 2024 articles Premenstrual Syndrome Scopus articles Premenstrual Syndrome impact factor journals Premenstrual Syndrome Scopus journals Premenstrual Syndrome PubMed journals Premenstrual Syndrome medical journals Premenstrual Syndrome free journals Premenstrual Syndrome best journals Premenstrual Syndrome top journals Premenstrual Syndrome free medical journals Premenstrual Syndrome famous journals Premenstrual Syndrome Google Scholar indexed journals Female Students articles Female Students Research articles Female Students review articles Female Students PubMed articles Female Students PubMed Central articles Female Students 2023 articles Female Students 2024 articles Female Students Scopus articles Female Students impact factor journals Female Students Scopus journals Female Students PubMed journals Female Students medical journals Female Students free journals Female Students best journals Female Students top journals Female Students free medical journals Female Students famous journals Female Students Google Scholar indexed journals Private University articles Private University Research articles Private University review articles Private University PubMed articles Private University PubMed Central articles Private University 2023 articles Private University 2024 articles Private University Scopus articles Private University impact factor journals Private University Scopus journals Private University PubMed journals Private University medical journals Private University free journals Private University best journals Private University top journals Private University free medical journals Private University famous journals Private University Google Scholar indexed journals menstrual cycle articles menstrual cycle Research articles menstrual cycle review articles menstrual cycle PubMed articles menstrual cycle PubMed Central articles menstrual cycle 2023 articles menstrual cycle 2024 articles menstrual cycle Scopus articles menstrual cycle impact factor journals menstrual cycle Scopus journals menstrual cycle PubMed journals menstrual cycle medical journals menstrual cycle free journals menstrual cycle best journals menstrual cycle top journals menstrual cycle free medical journals menstrual cycle famous journals menstrual cycle Google Scholar indexed journals economically articles economically Research articles economically review articles economically PubMed articles economically PubMed Central articles economically 2023 articles economically 2024 articles economically Scopus articles economically impact factor journals economically Scopus journals economically PubMed journals economically medical journals economically free journals economically best journals economically top journals economically free medical journals economically famous journals economically Google Scholar indexed journals Gynaecologists articles Gynaecologists Research articles Gynaecologists review articles Gynaecologists PubMed articles Gynaecologists PubMed Central articles Gynaecologists 2023 articles Gynaecologists 2024 articles Gynaecologists Scopus articles Gynaecologists impact factor journals Gynaecologists Scopus journals Gynaecologists PubMed journals Gynaecologists medical journals Gynaecologists free journals Gynaecologists best journals Gynaecologists top journals Gynaecologists free medical journals Gynaecologists famous journals Gynaecologists Google Scholar indexed journals Obstetricians articles Obstetricians Research articles Obstetricians review articles Obstetricians PubMed articles Obstetricians PubMed Central articles Obstetricians 2023 articles Obstetricians 2024 articles Obstetricians Scopus articles Obstetricians impact factor journals Obstetricians Scopus journals Obstetricians PubMed journals Obstetricians medical journals Obstetricians free journals Obstetricians best journals Obstetricians top journals Obstetricians free medical journals Obstetricians famous journals Obstetricians Google Scholar indexed journals Molecular Epidemiology articles Molecular Epidemiology Research articles Molecular Epidemiology review articles Molecular Epidemiology PubMed articles Molecular Epidemiology PubMed Central articles Molecular Epidemiology 2023 articles Molecular Epidemiology 2024 articles Molecular Epidemiology Scopus articles Molecular Epidemiology impact factor journals Molecular Epidemiology Scopus journals Molecular Epidemiology PubMed journals Molecular Epidemiology medical journals Molecular Epidemiology free journals Molecular Epidemiology best journals Molecular Epidemiology top journals Molecular Epidemiology free medical journals Molecular Epidemiology famous journals Molecular Epidemiology Google Scholar indexed journals Analytics articles Analytics Research articles Analytics review articles Analytics PubMed articles Analytics PubMed Central articles Analytics 2023 articles Analytics 2024 articles Analytics Scopus articles Analytics impact factor journals Analytics Scopus journals Analytics PubMed journals Analytics medical journals Analytics free journals Analytics best journals Analytics top journals Analytics free medical journals Analytics famous journals Analytics Google Scholar indexed journals Visualization articles Visualization Research articles Visualization review articles Visualization PubMed articles Visualization PubMed Central articles Visualization 2023 articles Visualization 2024 articles Visualization Scopus articles Visualization impact factor journals Visualization Scopus journals Visualization PubMed journals Visualization medical journals Visualization free journals Visualization best journals Visualization top journals Visualization free medical journals Visualization famous journals Visualization Google Scholar indexed journals
Article Details
1.Introduction
Premenstrual Syndrome is one of the most common disorders of reproductive age that can be seen in different intensities in 85-90 % of women [1]. It refers to the emotional, behavioral and physical changes that occur in the late luteal phase of a woman’s menstrual cycle (one to two weeks before her periods) [2-6]. Symptoms usually last for six days and are resolved with the onset of menstruation, with a symptom-free interval afterwards [2]. Though more than 200 symptoms have been known to occur, the most frequently occurring symptoms include headache, fatigue, abdominal bloating, backache, breast tenderness, fatigue, anxiety, irritability, social withdrawal and depression [7-11]. Premenstrual Dysphoric Disorder (PMDD) is a severe form of Premenstrual Syndrome (PMS), which leads a significant loss of function due to unusual severe symptoms that occurs in 2–6% of women [12]. The underlying cause(s) of PMS remain unclear. It is believed that the trigger behind PMS is multi-factorial in nature, with perturbations in reproductive hormone levels being one of the major causes [13]. Epidemiological Surveys have estimated that the frequency of PMS symptoms is quite high about 80-90 % and about 5 % of women experience severe symptoms that the symptoms interfere with their daily activities [14].
The PMS symptoms could impact an individual’s interpersonal relationships, social interactions, occupational activities and productivity for her entire reproductive age life [15, 16]. Especially for young women, premenstrual symptoms can be related to academic performance impairments including poor grades [17] and absenteeism [18]. This disorder in young women is a significant public health problem, as increased incidence of depression and anxiety disorders were found in women suffering with PMS, which could economically burden the society indirectly in the form of absenteeism at work, frequent hospitalization and suicides [19]. With this background the present study was conducted to assess the Knowledge, most commonly reported symptoms, impairments affecting educational activities and interpersonal relationships, treatment options, and attitude of female students towards PMS.
2. Materials and Methods
This cross-sectional study was conducted among 130 female students of a Private University of Delhi NCR. The inclusion criteria were female students of college of 17-30 years of age and exclusion criteria were students suffering from PCOD/PCOS. A pretested, self-administered questionnaire was used to collect the information. The questionnaire comprised of three parts. The first part included questions on Knowledge of PMS and PMDD, Demographic data and Menstrual History. The second part included questions on symptoms of PMS. The third part included questions about impairments, treatment options and attitude towards PMS. Symptoms of PMS were assessed according to American College of Obstetricians and Gynaecologists (ACOG) criteria [20]. The data was compiled in Microsoft excel and analysed using SPSS 25 version for various descriptive statistics and bivariate analysis. P-value <0.05 was considered statistically significant.
3. Result
The study included 130 participants. Bivariate analysis of association between Socio-Demographic variables and Menstrual Patterns and knowledge of PMS is presented in Table 1. Majority of female participants (55.4 %) belonged to age group 17 and 22 years.10.8 % of study participants were obese. Majority of them 89 (68.5 %) were UG students. Majority of them 79 (60.8 %) were from Outside Delhi. Considering the stay 47 (36.2 %) stay in home and 83 (63.8 %) stay in hostel. Majority of them 97 (74.6 %) were doing the exercise. Only 39 (30 %) of them were consuming coffee on daily basis. 57 (43.8 %) were consuming tea on daily basis. Considering the drinking alcohol 39 (30 %) of them were drinking alcohol. In Table 1 it was found that the female participants of age group between 23 and 30 years showed higher proportion of knowledge of PMS (n=52, 89.7 %) when compared to female participants of age group between 17 and 22 years and this association was statistically significant (P<0.05). The female participants of PG course showed higher proportion of knowledge of PMS (n=38, 92.7 %) when compared to female participants of UG course and this association was statistically significant (P<0.05). The female participants who did exercise showed higher proportion of knowledge of PMS (n=82, 84.5 %) when compared to female students who did not exercise and this association was statistically significant (P<0.05). No statistically significant association was observed with BMI, residence, current stay, coffee consumption on daily basis, tea consumption on daily basis and drinking alcohol.
Regarding the age at menarche majority 83 (63.8 %) of female participants had their menarche at the age of >12 years. Majority of them 112 (86.2 %) had their menstrual cycle of ≤ 35 days. Regarding the days of menstrual bleeding majority111 (85.5 %) of them had menstrual bleeding of ≤ 5 days. Majority of female participants 110 (84.6 %) had normal/light menstrual flow. Regarding the regularity of cycle majority of them 109 (83.8 %) had regular cycle. Only 11 (8.5 %) had family history of PMS. More than half 76 (58.5 %) of females suffer from dysmenorrhea. In Table 1 it was also found that the female participants who had regular cycles showed higher proportion of knowledge of PMS (n=91, 83.5 %) when compared to female students who had irregular cycles and this association was statistically significant (P<0.05). No statistically significant association was observed with age at menarche, length of menstrual cycle, days of bleeding, amount of menstrual flow, Family history of PMS and dysmenorrhea. Knowledge of PMS and PMDD among study participants is presented in Figure1. 80% of study participants had knowledge of PMS and only 43.8% participants had knowledge of PMDD. The Premenstrual Symptoms according to ACOG criteria are presented in Figure 2. The most common affective symptoms among participants were irritability (74.6 %), angry outbursts (62.3 %) and anxiety (51.6 %). The most common somatic symptoms among participants were: abdominal bloating (48.5 %) and headache (40.8 %).
Effect of PMS on Educational activities and Interpersonal relationships and Treatments opted by female participants to relieve their premenstrual symptoms is presented in Table 2. Most frequent impairments seen in this study were: Concentration impairment (53.8), College/work efficiency/productivity impairment (53.8 %) and Social life activities impairment (49.2 %). Other impairments were: Home responsibilities impairment (46.9 %), Motivation impairment (46.9 %), Absenteeism from college (45.4 %), Relationship with friends/classmates/family impairment (42.3 %), Low scores/grades (25.4 %). The most frequent treatments opted by female participants were: Hot Pack (56.2 %), Traditional remedies (40.8 %) and (40.8 %) of female participants did nothing to relieve their premenstrual symptoms. Only (10.8 %) of female participants seeks gynecologist to relieve their symptoms. Use of painkillers (27.7 %), exercise/yoga (26.9 %), dietary supplements (26.2 %) and homeopathic medication (6.9 %) were less common among female participants in our study. Attitude of female participants towards PMS is presented in Table 3. Majority (90 %) of female participants think that PMS is an important issue that should be discussed, (84.6 %) of female participants want to talk to their family/spouse about PMS, (81.5 %) of female participants think that Menstrual leave should be an option at college/workplace and (72.3 %) of them were likely to consult a doctor for PMS.
|
Variables |
Frequency (%) |
Knowledge of PMS (No) n=26 (%) |
Knowledge of PMS (Yes) n=104 (%) |
P-value |
|
Age 17-22 years 23-30 years |
72 (55.4) 58 (44.6) |
20 (27.8) 6 (10.3) |
52 (72.2) 52 (89.7) |
0.014* |
|
BMI (kg/m2) Normal Overweight Obese |
78 (60.0) 38 (29.2) 14 (10.8) |
13 (16.7) 7 (18.4) 6 (42.9) |
65 (83.3) 31 (81.6) 8 (57.1) |
0.075 |
|
Course PG UG |
41(31.5) 89 (68.5) |
3(7.3) 23 (25.8) |
38 (92.7) 66 (74.2) |
0.014* |
|
Residence Delhi Outside Delhi |
51 (39.2) 79 (60.8) |
9 (17.6) 17 (21.5) |
42 (82.4) 62 (78.5) |
0.590 |
|
Stay Home Hostel |
47 (36.2) 83 (63.8) |
9 (19.1) 17 (20.5) |
38 (80.9) 66 (79.5) |
0.855 |
|
Exercise No Yes |
33 (25.4) 97 (74.6) |
11 (33.3) 15 (15.5) |
22 (66.7) 82 (84.5) |
0.027 * |
|
Consume Coffee on Daily basis No Yes |
91 (70.0) 39 (30.0) |
22 (24.2) 4 (10.3) |
69(75.8) 35 (89.7) |
0.069 |
|
Consume Tea on Daily basis No Yes |
73 (56.2) 57 (43.8) |
15 (20.5) 11 (19.3) |
58 (79.5) 46 (80.7) |
0.860 |
|
Drink Alcohol No Yes |
91 (70.0) 39 (30.0) |
22 (24.2) 4 (10.3) |
69 (75.8) 35 (89.7) |
0.069 |
|
Age at Menarche ≤12 years >12 years |
47 (36.2) 83 (63.8) |
12 (25.5) 14 (16.9) |
35 (74.5) 69 (83.1) |
0.259 |
|
Length of Menstrual Cycle ≤ 35 days > 35 days |
112 (86.2) 18 (13.8) |
20 (17.9) 6 (33.3) |
92 (82.1) 12 (66.7) |
0.199 |
|
Days of Bleeding ≤5 days >5 days |
111 (85.5) 19 (14.5) |
23 (20.7) 3 (15.8) |
88 (79.3) 16 (84.2) |
0.763 |
|
Amount of Menstrual Flow Normal/Light Heavy |
110 (84.6) 20 (15.4) |
23 (20.9) 3 (15.0) |
87 (79.1) 17 (85.0) |
0.763 |
|
Regularity of Cycle Regular Irregular |
109 (83.8) 21 (16.2) |
18 (16.5) 8 (38.1) |
91 (83.5) 13 (61.9) |
0.035 ** |
|
Family History of PMS No Yes |
119 (91.5) 11(8.5) |
25 (21.0) 1(9.1) |
94 (79.0) 10 (90.9) |
0.693 |
|
Dysmenorrhea No Yes |
54 (41.5) 76 (58.5) |
12 (22.2) 14 (18.4) |
42 (77.8) 62 (81.6) |
0.659 |
*/**P<0.05 is considered statistically significant. PMS-Premenstrual Syndrome, * Chi-square P-value, ** Fisher’s exact P-value
Table 1: Bivariate Analysis of association between Socio-Demographic Variables and Menstrual Patterns and Knowledge of PMS (n=130).
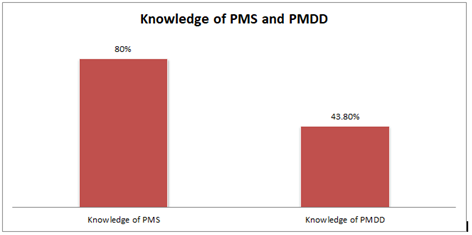
Figure 1: Knowledge of PMS and PMDD among study participants (n=130).
*PMS-Premenstrual Syndrome, PMDD-Premenstrual Dysphoric Syndrome
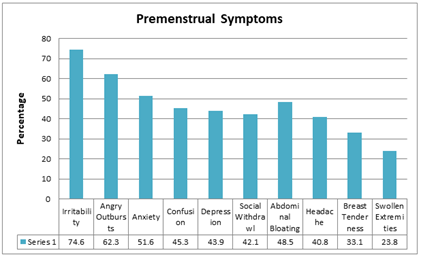
Figure 2: Premenstrual symptoms among study participants according to the American College of Obstetricians and Gynaecologists (ACOG) criteria (n=130).
|
Impairments |
n (%) |
|
Concentration impairment |
70 (53.8) |
|
College/Work Efficiency/Productivity impairment |
70 (53.8) |
|
Motivation impairment |
61 (46.9) |
|
Absenteeism from college |
59 (45.4) |
|
Low Scores/Grades |
33 (25.4) |
|
Social Life activities impairment |
64 (49.2) |
|
Home Responsibilities impairment |
61 (46.9) |
|
Relationship with Friends/Classmates impairment |
55 (42.3) |
|
Relationship with your Family impairment |
55 (42.3) |
|
Treatments Opted |
|
|
Hot Pack |
73 (56.2) |
|
Traditional Remedies |
53 (40.8) |
|
Painkillers |
36 (27.7) |
|
Exercise/Yoga |
35 (26.9) |
|
Dietary Supplements |
34 (26.2) |
|
Seeks Gynecologist |
14 (10.8) |
|
Homeopathic Medication |
9 (6.9) |
|
Do nothing to relieve symptoms |
53 (40.8) |
Table 2: Effect of PMS on Educational activities and Interpersonal relationships ant Treatments opted by female participants to relieve their premenstrual symptoms (n=130).
|
Characteristics |
n (%) |
|
Do you think PMS is an important issue that should be discussed |
117 (90.0) |
|
Do you want to talk to your Family/Spouse about PMS |
110 (84.6) |
|
Do you think Menstrual leave should be an option at college/workplace |
106 (81.5) |
|
Are you likely to consult a doctor for PMS |
94 (72.3) |
Table 3: Attitude of female participants towards PMS (n=130).
4. Discussion
PMS is common among women of reproductive age (15-49 years of age) [21]. It is accompanied by different symptoms that affect health [22, 23]. The mean age of the female students in this study was 22.32 ± 3.2 years. Similar mean age was found in study done by Mohib A et al [24] whereas the mean age of the students was less in studies done in West Bengal [25], Gujarat [26], Thailand [27] and Egypt [28]. The majority (80 %) of the female participants in this study knew about PMS while only (43.8 %) knew about PMDD. Similar findings were found in the study done by Mohib A et al. [24] where (96.4 %) of female students were aware of PMS while only (19 %) of females knew about PMDD, whereas a study done by Pal SA [29] in Pakistan reported that (98.8 %) of females were unaware of the phenomenon of PMS. In this study Irritability (74.6 %) was found to be the most commonly reported affective symptom which had been reported by several other studies [30-35]. Studies done in West Bengal [25] and Malaysia [36] also reported irritability as the most common affective symptom, whereas studies done in Gujarat [26] and Thailand [27] reported irritability as the third most common reported symptoms.
In our study Abdominal bloating (48.5 %) was found to be the most commonly reported somatic symptom, whereas a study done in West Bengal [25] reported abdominal bloating as the second most common somatic symptom and a study done in Thailand [27] reported abdominal bloating as the third most common somatic symptom. The most frequent impairments seen in this study were: Concentration impairment (53.8 %) and College/work efficiency/productivity impairment (53.8 %). Similar finding was found in the studies done in South India [37] and Gujarat [26] where the most frequent impairment was school/work efficiency/productivity impairment, whereas a study done in Thailand [27] reported Low scores as the most frequent impairment.
In this study the most frequent treatments opted by female students in order to relieve their symptoms were: Hot Pack (56.2 %) and Traditional remedies (40.8 %), whereas a study by Mohib A et al. [24] reported using analgesics (41%) and doing exercise (17.7 %) were the most common treatments opted by females to relieve their symptoms. In our study (40.8 %) of female participants did nothing to relieve their premenstrual symptoms. Similar finding was reported in the study done by Mohib A et al. [24] where (49.4 %) of females did nothing to relieve their symptoms. A positive attitude towards PMS was noted in our study with (90 %) of female participants think that PMS is an important issue that should be discussed, (84.6 %) of female participants want to talk to their family/spouse about PMS and (81.5 %) of female participants think that Menstrual leave should be an option at College/Workplace. These findings were similar to the study done by Mohib A et al. [24] Despite of the positive response only (10.8 %) of female participants seeks gynecologist to relieve their premenstrual symptoms. This result is comparable to the findings of a national survey done in Spain [38] where only (18.7 %) of females take medical advice for PMS. Despite of the positive response of female participants towards PMS in our study, there is lack of knowledge about the necessity to consult a doctor or seek treatment for their symptoms.
Limitations
The study has certain limitations. It included a small and selective sample size which comprises of college students. The reporting of premenstrual symptoms was based on retrospective recall of the participants which adds a recall bias in data collection.
5. Conclusion
Based on the findings of the present study, it can be said that: PMS is a common problem affecting the educational activities and interpersonal relationships of female participants significantly. Although a positive attitude towards PMS was noted in our study but (40.8%) of female participants did nothing to relieve their premenstrual symptoms and only (10.8%) of them seek gynecologist to relieve their symptoms. Despite of the positive response of female participants towards PMS in our study, there is lack of knowledge about the necessity to consult a doctor or seek treatment for their symptoms. Further research is required on a larger population.
Acknowledgement
The authors are very much grateful to all participants of the study for their kind cooperation.
Conflict of Interest
None
Source of Support
None
References
- Kwan I, OnwudeLoze J. Premenstrual Syndrome. Clinical Evidence 12 (2009): 806.
- Braverman PK. Premenstrual syndrome and premenstrual dysphoricdisorder. J. Pediatr. Adolesc. Gynecol 1 (2007): 3-12
- O’Brien PM, Eriksson E. Premenstrual syndrome. Lancet 371 (2008): 1200-1210.
- Silva CM, Gigante DP, Carret ML, Fassa AG. Population study of premenstrual syndrome. Rev SaudePublica 40 (2006): 47-56.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) (1994).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems.10thRevision (ICD -10). Geneva: WHO (1992).
- Zaka M, Mahmood KT. Pre-menstrual syndrome-a review. J Pharm Sci Res 4 (2012): 1684-1691.
- Mayo J, Joseph L. Premenstrual syndrome: a natural approach to management. ApplNutrSci Rep 5 (1999): 1-8.
- Mahesh A, Ali S, Tirmizi Z. Frequency and associated factors of premenstrual syndrome in Medical College girls premenstrual syndrome in medical. Med Channel 2014 (2011): 34-38.
- Sarkar AP, Mandal R, Ghorai S. Premenstrual syndrome among adolescent girl students in a rural school of West Bengal, India. Int J Med Sci Public Health 5 (2016): 5-8.
- Badkur D, Wanjpe A, Singh S, Chouhan DS, Sinha A. Premenstrual Syndrome among female students of colleges in Ujjain City, Madhya Pradesh. Natl J Commun Med 7 (2016): 75-78.
- Khajehei M. Aetiology, diagnosis and management of premenstrual syndrome. J Pain Relief 4 (2015): 193.
- Premenstrual syndrome (PMS) fact sheet. Office on Women's Health (2014).
- Magfirah: Dating Violence and Premenstrual Syndrome among adolescent girl in Senior High Schools of Purworejo District. Matern Child Health-Reprod Health Study ProgramPublic Health Science (2011): 1-6.
- Lavu D, Kadian S, O’Brien PMS. Biopsychosocial factors in premenstrual syndrome. In: Edozien LC, O’Brien PMS, editors. Biopsychosocial factors in obstetrics and gynaecology. Cambridge: Cambridge University Press (2017): 94-101
- Matsumoto T, Asakura H, Hayashi T. Premenstrual disorders: luteal phase recurrent enigmatic conditions. In: Lal M, editor. Clinical psychosomatic obstetrics and gynaecology: a patient-centred biopsychosocial practice. Oxford: Oxford University Press (2017): 175-198
- Tolossa FW, Bekele ML. Prevalence, impacts and medical managements of premenstrual syndrome among female students: cross-sectional study in College of Health Sciences, Mekelle University, Mekelle, Northern Ethiopia. BMC Womens Health 14 (2014): 52.
- Tadakawa M, Takeda T, Monma Y, Koga S, Yaegashi N. The prevalence and risk factors of school absenteeism due to premenstrual disorders in Japanese high school students-a school-based cross-sectional study. Biopsychosoc Med 10 (2016): 1
- Joshi JV, Pandey SN, Galvankar P, Gogate JA. Prevalence of premenstrual symptoms: preliminary analysis and brief review of management strategies. Journal of mid-life health 1 (2010): 30-34.
- ACOG Practice Bulletin. Premenstrual syndrome. Clinical management guidelines for obstetrician- gynecologists. Number 15. J Obstet Gynecol 73 (2001): 183-191.
- Batra P, Harper DM. Recognizing and treating the premenstrual symptom severity: impact on social functioning andtreatment seeking behavior. J Clin Outcomes Manage 9 (2002): 87-98.
- Campagne D, Campagne G. The premenstrual syndrome revisited. European Journal of Obstetrics &Gynecology and Reproductive Biology 130 (2007): 4-17.
- Dennerstein L, Lehert P, Bäckström T. Premenstrual symptoms. Severity, duration and typology: An international cross-sectional study. MenopauseInternational 15 (2009): 120-126.
- Aleena Mohib, Amara Zafar, Areeba Najam, Hafsa Tanveer, Rehana Rehman. Premenstrual Syndrome: Existence, Knowledge, and Attitude Among Female University Students in Karachi. Cureus 10 (2018): e2290.
- RanjanaMandal, Aditya Prasad Sarkar, SupritiGhorai. A study on premenstrual syndrome among adolescent girl students in an urban area of West Bengal. Int J ReprodContraceptObstet Gynecol (2015):
1012-1015.
- Raval CM, Panchal BN, Tiwari DS, Vala AU, Bhatt RB. Prevalence of premenstrual syndrome and premenstrual dysphoric disorder among college students of Bhavnagar, Gujarat. Indian J Psychiatry. Apr-Jun 58 (2016): 164-170.
- Buddhabunyakan N, Kaewrudee S, Chongsomchai C, Soontrapa S, Somboonporn W, Sothornwit J. Premenstrual syndrome (PMS) among high school students. Int J Womens Health 9 (2017): 501-505.
- Amany Edward Seedhom, EmanSameh Mohammed, Eman Mohammed Mahfouz. Life Style Factors Associated with Premenstrual Syndrome among El-Minia University Students, Egypt. Hindawi Publishing Corporation, ISRN Public Health (2013).
- Pal SA, Dennerstein L, Lehert P. Premenstrual symptoms in Pakistani women and their effect on activities of daily life. J Pak Med Assoc 61 (2011): 763-768.
- Steiner M, Maodougall M, Brown E. The premenstrual symptoms screening tool (PSST) for clinicians. Arch WomensMent Health (2003): 203-209.
- Steiner M, Peer M, Palova E, Freeman EW, Macdougall M, Soares CN. The premenstrual symptoms screening tool revised for adolescents (PSST-A): Prevalence of severe PMS and premenstrual dysphoric disorder in adolescents. Arch WomensMent Health 14 (2011): 77-81
- Tabassum S, Afridi B, Aman Z, Tabassum W, Durrani R. Premenstrual syndrome: Frequency and severity in young college girls. J Pak Med Assoc 55 (2005): 546-549.
- Nisar N, Zehra N, Haider G, Munir AA, Sohoo NA. Frequency, intensity and impact of premenstrual syndrome in medical students. J Coll Physicians Surg Pak 18 (2008): 481-484.
- Pearlstein T, Yonkers KA, Fayyad R, Gillespie JA. Pretreatment pattern of symptom expression in premenstrual dysphoric disorder. J Affect Disord 85 (2005): 275-282.
- Bansal M, Goyal M, Yadav S, Singh V. Premenstrual syndrome – A monthly menace. Indian J ClinPract 22 (2012): 491-494.
- Wong LP, Khoo EM. Menstrual-related attitudes and symptoms among multi-racial Asian adolescent females. Int J Behav Med 18 (2011): 246-253.
- SivanandhBudarapu, Haripriya Sadam, Harshitha K, DivyaNageswari M, Harshitha Reddy K, Gouri Dhanekula. A Study to Assess the Prevalence of Premenstrual Syndrome and Premenstrual Dysphoric Disorder and Various Coping Strategies used by Students in A Womens Medical College from South India. International Journal of Contemporary Medical Research 5 (2018): K1-K5.
- Lete I, Dueñas JL, Serrano I, Doval JL, Martínez-Salmeán J, Coll C, et al. Attitudes of Spanish women toward premenstrual symptoms, premenstrual syndrome and premenstrual dysphoric disorder: results of a nationwide survey.. Eur J ObstetGynecolReprod Biol 159 (2011): 115-118.
