A Case of Intrahepatic Biliary Atresia in Pediatrics
Article Information
Srikanth Darisi
Pharm D, Rajiv Gandhi University of Health Sciences, Karnataka, India
*Corresponding Author: Srikanth Darisi, Pharm D, Rajiv Gandhi University of Health Sciences, Karnataka, India
Received: 05 May 2021; Accepted: 17 May 2021; Published: 26 May 2021
Citation:
Srikanth Darisi. A Case of Intrahepatic Biliary Atresia in Pediatrics. Journal of Pediatrics, Perinatology and Child Health 5 (2021): 130-135.
View / Download Pdf Share at FacebookAbstract
The chief objective of this case report is to give a overview of how Biliary atresia (BA) occurs, presents, and management. Biliary atresia is a congenital abnormality with mostly affects the biliary tract (intrahepatic or extrahepatic) and often presents with symptoms of jaundice, the prevalence of this disease is more in Asian females than males. This case demonstrates a male patient of 6 months 8 days old he presented with fever, abdominal distension, severe anemia, and also yellowish discoloration of skin sclera and urine, he was diagnosed with intrahepatic biliary atresia, It is important to diagnose if it is intra hepatic or extrahepatic biliary atresia as the treatment Caries for both, Treatment in case of extrahepatic biliary atresia is Kasai procedure but the diagnosis in his case is intrahepatic biliary atresia Kasai procedure is not done, the patient is given symptomatic treatment and is enlisted for a liver transplant.
Keywords
Biliary Atresia, Chronic Liver Disease, Liver Transplant, Kasai Procedure, Pediatrics
Biliary Atresia articles; Chronic Liver Disease articles; Liver Transplant articles; Kasai Procedure articles; Pediatrics articles
Article Details
1. Introduction
Biliary atresia is a congenital malformation of the parts of the Biliary tract [1] or sometimes even absent, it is commonly caused due to CMV [2] mediated inflammation and also due to autoimmune-mediated bile duct destruction [3] and there is also a role of genetic mutation CFC1 gene; if left untreated it may even cause the cirrhosis and even death of liver cells [3] it is an inflammatory disorder which can involve any part the bile tree; from the removal of bile in the liver through intra-hepatic bile duct till the entry of bile into the intestine with the help of common bile duct, The incidence of biliary atresia is high in Asia and also the Pacific region; females are more prone to this disease more than males, it is also called as Newborn jaundice - biliary atresia.
2. Case Presentation
A 6 months male patient of 7.25Kgs was admitted to hospital with the chief complaints of abdominal distension, fever on and off since 4 months, Pale stools, yellowish discoloration of body, sclera, urine, decreased oral intake, sleep, irritability since 4 months, up on physical examination of the abdomen, patient was found to have firm tenderness, hepatomegaly, Splenomegaly, umbilical hernia, Vitals on admission were as follows heart rate of 140bpm, Respiratory rate of 25cpm, temp of 99.8°F, Spo2 of>95% Laboratory values reveled altered liver function test (T.Bilirubin- 12.14, D.Blilrubin-9.64mg/dL, Total protein of 5g/Dl, albumin -1.8g/dL, SGOT-151 IU/L, SGPT- 70IU/L), altered coagulation panal (PT-13.9 sec, INR-1.36), Total counts were elevated (25,100), Hb of 6.5g/dL, abnormal in Iron, USG abdomen showed Hepatomegaly, splenomegaly and contracted gall bladder, 2D echo was normal, Color doppler of liver was done : Non visualized main portal vein, small sized hepatic vein with monophasic flow, elevated PSV in hepatic artery with diastolic flow reversal, multiple cysts of variable size alone the intra and hepatic biliary radicals, ascites, for further evaluation CT Abdomen was done in which multiple well defined hypodense cystic lesions of varing size in the region of intrahepatic biliary radicals with central dot sign was seen, patient was diagnosed to have intrahepatic biliary atresia with decompensated liver disease, He was started on Inj. Vitamin K, Inj.Piptaz, Inj, Amikacin, Vitamin E, Vitamin A, Vitamin D3, Tab. Spironolactone, Furosemide, Syp, UDCA, SYP. Shelcal, Tab Vangancyclovir and is listed for a liver transplant.
3. Discussion
Classification of Biliary atresia
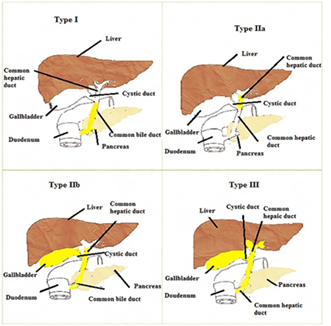
- Based on the area affected [4] (Figure 1)
- Based on the time of onset of disease: if symptoms appear within 2 weeks of birth it is called early-onset Biliary atresia, if symptoms appear after 2 weeks of birth it is said to be late-onset Biliary atresia [5, 6].
- Based on the organs involved
- SyndromicBA: - this type of BA is asso-ciated with various congenital abnormalities such as Asplenia, Polysplenia, cardiac or other inter-abdominal defects such as situs inversus, pre-duodenal portal vein, the absence of retro hepatic inferior vena cava, intestinal malrotation.
- Non-Syndromic BA: - It accounts for about 90% of the cases in which there is only a
It can be classified into different types such as TYPE 1 here common bile duct is being affected, TYPE2 it is of 2 types: 2a in this type common hepatic duct is affected, 2b in this type common hepatic duct, cystic duct, common bile duct are affected, TYPE 3this type of biliary atresia involves entire bile pathway which includes intrahepatic duct, common hepatic duct, cystic duct, and common bile duct.
Patients with Biliary atresia usually present with complaints of Jaundice within the second or third week of the birth which is characterized by the yellowish discoloration of skin, sclera, and urine, Alcoholic stools which is a result of less bile in the GIT due to obstruction or inflammation of the bile duct, infants may also have abdominal distension, liver enlargement the patient may have developed symptoms which include poor weight gain, irritability, and increase in blood pressure within the portal veins by the age of 6 to 10 weeks.
3.1 Screening of biliary atresia
Every case of jaundice that is persistent for more than 2weeks should be checked for the Biliary atresia.
- Ultrasound: This should be done after 12hours of fasting, if the gallbladder is shrunk despite fasting it can be suspected to be biliary atresia if there is any cyst in the liver hilum [6].
- Cholangiography: This test is performed when ultrasound is clear, to assess the morphology and patency of the Biliary Tree [6].
- Liver Biopsy: This can reveal the histological changes that occurred due to BA which include Bile plugs, Ductular proliferation, portal edema, and also fibrosis[6].
- Stool Color Cards [5]: Infant screening for BA is done by using Stool color cards in some countries, in which the color of the stool is monitored for about one month and is compared with color cards for diagnosis; the specificity of this test is low and the efficacy of this method is not yet proved As in Table No. 1.
It can also be caused by the CMV virus which can be diagnosed through the testing of antigen for CMV such as IGM and IGG.
Biochemical Liver Function Tests which include Abnormal LFT’s are seen In all cases of BA, Elevation in serum Bilirubin and SGOT, SGPT, ALP; Decrease in the serum protein is seen, alterations in LFT’s does not indicate the duration of disease but they reveal the extent of parenchymal damage [1]. This helps us to know if liver damage is present.
|
Stool color |
Remarks |
|
Red |
Bleeding lower gut or rectum |
|
White, Clay color. |
Antidiarrheal, lack of bile |
|
Green |
Antibiotics, bacterial infection |
|
Yellow |
Excess fat, small intestine infection |
|
Black(or) dark brown |
Iron supplements, bismuth sub salicylate, Bleeding in the upper digestive tract |
Table 1: Stool color and remarks.
3.2 Management
During the treatment, some common medications given to the patients include multivitamins mostly Fat-soluble vitamins as there will be a deficiency of this fat-soluble vitamin due to the absence of bile [7], other medications can include Lactulose, antiviral therapy (If the BA is caused due to CMV virus), Biliary atresia is the most common indication for liver transplant in newborn; if diagnosed early it can be treated with surgical intervention called a KASAI procedure also called hepatoportoenterostomy before the development of this KASAI procedure, patients with BA had a very low prognosis rate [3]. If diagnosed early i.e. within 60 days of birth a hepatoportoenterostomy can be performed, in this procedure the necrotic part of the bile duct is surgically removed and the healthy duct is connected to the intestine for the flow of the bile [8] and a need of liver transplant can be minimized; but the success of this procedure depends upon the early diagnosis of the disease and this procedure is referred to as KASAI procedure and is only done if the child age is less than 60 days, however in some cases the patient may need the liver transplant within 2 years after this procedure Common complications of this procedure include infection and failure of this procedure [9], If the KASAI procedure fails to restore the bile flow from the liver to the intestine the alternative treatment option which are available is a liver transplant which in most of the cases occur at the age of 2 years from the KASAI procedure and can also occur even before that if the condition is severe The success of KASAI procedure depends upon the age of performing the KASAI operation [10-13].
In the case of Intrahepatic BA, we can do a liver transplant by obtaining a liver from any cadaveric donor or from a living parent donor (The cadaveric donor is a donor who is of the same age only a few lobes of the liver are taken for this procedure), The mortality rate of patients waiting for a liver transplant has decreased in recent times due to the development of new techniques such as liver graft splitting [14], living related donor [15].
4. Conclusion
In this case reported, the cause of BA is due to inflammation which is mediated by CMV and the patient was diagnosed having BA with Caroli's disease (inflammation of intrahepatic bile ducts) and is listed for a liver transplant, The patient is started with antibiotics to help reduce the inflammation, antiviral therapy for CMV virus, other supportive measures such as multivitamins to treat the malabsorption due to decreased secretion of bile into the duodenum, According to recent research the best nutrition treatment for BA patients before liver transplantation include cycled enteral nocturnal feeding with daily oral feeds using formula (16)(17), After liver transplant it is recommended that the patient is on parental feeding for two days for recovery, later patient can have enteral feeding.
Acknowledgment
The author(s) would like to acknowledge, Karnataka College of Pharmacy, Karnataka, India for providing an institutional research platform and necessary facilities.
Competing Interests
The author(s) declare that they have no competing interests
References
- Sinha CK, Davenport M. Biliary atresia [Internet]. Journal of Indian Association of Pediatric Surgeons 13 (2008): 49-56.
- Fontenele JPU, Schenka AA, Hessel G, et al. Clinical and pathological challenges in the diagnosis of late-onset biliary atresia: Four case studies. Brazilian J Med Biol Res 49 (2016): 10-13.
- Feldman AG, Mack CL. Biliary atresia: Clinical lessons learned. J Pediatr Gastroenterol Nutr 61 (2015): 167-175.
- Ghazy RM, Adawy NM, Khedr MA, et al. Biliary atresia recent insight. Egypt Pediatr Assoc Gaz 66 (2018): 1-8.
- Hsiao CH, Chang MH, Chen HL, Lee HC, Wu TC, Lin CC, et al. Universal screening for biliary atresia using an infant stool color card in Taiwan. Hepatology 47 (2008): 1233-1240.
- Chardot C. Biliary atresia. Orphanet J Rare Dis 1 (2006).
- Venkat VL, Shneider BL, Magee JC, et al. Total serum bilirubin predicts fat-soluble vitamin deficiency better than serum bile acids in infants with biliary atresia. J Pediatr Gastroenterol Nutr 59 (2014): 702-707.
- Balistreri WF. Early diagnosis of biliary atresia. J Pediatr 166 (2015): 783-787.
- Lillegard JB, Miller AC, Flake AW. Biliary atresia. Fundam Pediatr Surgery, Second Ed (2016): 629-636.
- Chardot C, Carton M, Spire-Bendelac N, et al. Prognosis of biliary atresia in the era of liver transplantation: French National Study from 1986 to 1996. Hepatology 30 (1999): 606-611.
- Altman RP, Ully JR, Greenfeld J, et al. A Multivariable Risk Factor Analysis of the Portoenterostomy (Kasai) Procedure for Biliary Atresia Twenty-Five Years of Experience From Two Centers. Annals of Surgery. Lippincott-Raven Publishers 226 (1997).
- Karrer FM, Lilly JR, Stewart BA, et al. Biliary atresia registry, 1976 to 1989. J Pediatr Surg 25 (1990): 1076-1081.
- Mieli-Vergani G, Portman B, Howard ER, et al. Late Referral for Biliary Atresia- Missed Opportunities for Effective Surgery. The Lancet 333 (1989): 421-423.
- Gridelli B, Spada M, Petz W, et al. Split-liver transplantation eliminates the need for living-donor liver transplantation in children with end-stage cholestatic liver disease. In: Transplantation. Lippincott Williams and Wilkins (2003): 1197-1203.
- Living-related liver transplantation in children at Saint-Luc University Clinics: a seven year experience in 77 recipients. PubMed (2021).
- Ramaccioni V, Soriano HE, Arumugam R, et al. Nutritional aspects of chronic liver disease and liver transplantation in children. J Pediatr Gastroenterol Nutr 30 (2000): 361-367.
- Moreno LA, Gottrand F, Hoden S, et al. Improvement of Nutritional Status in Cholestatic Children with Supplemental Nocturnal Enteral Nutrition. J Pediatr Gastroenterol Nutr 12 (1991): 213-216.